Diagnosis and treatment for our system of care
NHS England’s Director for Long Term Conditions, who is among the speakers at the Health+Care Commissioning Show, examines the need for new models of care:
William Osler, apart from his eponymous conditions, was famed for his teaching and his aphorisms. One of my favourites is: “Listen to your patient, he is telling you the diagnosis”.
Which is why we need to listen to people with long term conditions when they say that what they want is: “My care is planned with people who work together to understand me and my carer(s), put me in control, co-ordinate and deliver services to achieve my best outcomes”.
Yet if we listen to the patient and look at some ‘population diagnostics’ it would seem we could do better?
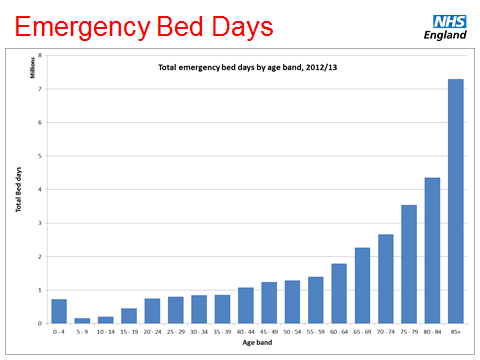
Across the population in England emergency bed day usage rises rapidly with age. The population aged less than 40 uses one million bed days a year. The population over the age of 85 uses seven million.
In addition, there are approximately 325,000 people in care and nursing homes. It is estimated 50 per cent do not get the support they deserve from the NHS. They have a 40 to 50 per cent higher rate of emergency admission than the general population over 75 and 42 per cent of admissions are in the last six months of life. There are, for comparison, 134,000 acute beds in the NHS.
More than 25 per cent of people admitted to acute hospitals have a co-morbid mental health problem. In older adults – over 65yrs – where delirium and dementia are more prevalent, the proportion rises to 60 per cent.
Of all hospital bed-days, 80 per cent are occupied by people with co-morbid physical and mental health problems and co-existing mental health problems are associated with a 45 to 75 per cent increase in service costs per patient (after controlling for the severity of physical illness).
With over 50 per cent of the population over the age of 18 self-reporting they have long term conditions, the diagnosis as to what ails the NHS is possibly that we need a new model of care? This is why the Five Year Forward View is so important – it sets out the treatment required.
Having visited two of the Vanguard sites, worked with integration pioneers, LTC Year of Care commissioning sites and visited forward thinking providers in both community and hospital settings, it seems to me that there is a desire and pull from professionals to change the ‘treatment’.
The way that community based care is being modelled to embrace the potential of digital technology; the way that the NHS is supporting and collaborating with the goodwill and assets that can be found, if you look, in every community; the collective working across GP practices, pharmacists, community services and collaboration with specialist services is transforming care.
The work to integrate mental and physical health services as the system begins to reconnect with whole person, rather than purely condition based care, is of critical value. Finally, it is the insight and understanding that one of the most powerful assets for the NHS is the person themselves.
This might best be illustrated by end of life care, where person centred care is so important. The Electronic Palliative Care System starts with a simple premise: develop a collaborative care plan with the individual which is used to support them. It is uploaded and made accessible wherever they are and at whatever time it is needed. Where implemented it has had a dramatic impact on place of death with less than 25 per cent of people dying in hospital compared with a national average nearer 50 per cent.
It seems to me the principles for treatment, given the problems we face, are a simple checklist for every community: to empower patients and carers, support and enable professional collaboration, deploy best practice and use our commissioning system, intelligently, to enable this to happen.
That is what the Five Year Forward View asks, that is what the Vanguards and Pioneers and others want to do. That is what we all must do.
It isn’t easy, but sometimes the treatment is worth it in the long run…

One comment
Mental Health Services within the NHS is improving, however like everything else, budget cuts are putting pressure on already strained services.