Your COVID recovery guidance
Contents
- Equality and Health Inequalities Statement
- Clinical case definition of post-COVID syndrome
- What is your COVID recovery?
- How will the online rehabilitation platform work?
- The development of your COVID recovery
- Evidence of effectiveness
- Accessibility
- Patient cohorts
- Target population
- Your COVID recovery access and training for services and systems
- Patient assessment
- Decision to refer
- Referral
- Your COVID recovery platform content
- Information governance and data protection
- Further information
- Appendices
Your COVID Recovery
Guidance for the online interactive platform
Equality and Health Inequalities Statement
Promoting equality and addressing health inequalities are at the heart of NHS England and NHS Improvement’s values. Throughout the development of the policies and processes cited in this document, we have:
- Given due regard to the need to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it; and
- Given regard to the need to reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities
Clinical case definition of post-COVID syndrome
This guidance refers to patients who meet the clinical case definition of post-COVID syndrome.
The National Institute for Health and Care Excellence (NICE), the Scottish Intercollegiate Guidelines Network (SIGN) and the Royal College of General Practitioners (RCGP) have defined post-COVID syndrome as:
Signs and symptoms that develop during or following an infection consistent with COVID-19 which continue for more than 12 weeks and are not explained by an alternative diagnosis. The condition usually presents with clusters of symptoms, often overlapping, which may change over time and can affect any system within the body. Many people with post-COVID syndrome can also experience generalised pain, fatigue, persisting high temperature and psychiatric problems.
Post-COVID-19 syndrome may be considered before 12 weeks while the possibility of an alternative underlying disease is also being assessed.
The rationale behind this is available here.
What is your COVID recovery?
Your COVID Recovery is an online platform with two key components:
-
- An open publicly available site containing general information on all aspects of recovering from COVID-19 including physical, emotional and psychological wellbeing. The site offers general advice on recovery, returning to work and information for families and carers of patients with post-COVID syndrome (also known as Long COVID). It also signposts to other agencies such as the British Lung Foundation and the Samaritans. The information on this site will be reviewed as the evidence and national guidance for management of the conditions develops. This site launched on 31 July 2020 and has had over 120,000 visits.
- An online, interactive rehabilitation platform specifically for patients with post-COVID syndrome, that is tailored for individuals and requires referral and face to face assessment from a healthcare professional. This will be live on 31 October 2020, to be rolled out using a phased approach, and is to be offered as an adjunct rather than a replacement for usual primary care support and rehabilitation services that are available.
How will the online rehabilitation platform work?
- After logging in with a personal code, patients are able to set their own goals, and access interactive rehabilitation components that are specific to their goals. There is a symptom tracker.
- Each local system will nominate a group of healthcare professionals that will be trained to accept referrals to and support patients using Your COVID recovery. These clinicians will be able to access the patients’ data and view their progress via an administration area of the platform.
- There will be an ‘ask the healthcare professional facility’, which the local provider will be responsible for responding to the registered patients’ communications would be routed to the trained healthcare professionals, who can respond according to the local arrangements.
- Each rehabilitation centre will have a discrete administration site to view patient progress through the site and respond to ‘ask the healthcare professional facility’ questions at a local level ensuring full local ownership of the caseload.
- There will be patient discussion forums for the development of local communities of patients with post-COVID syndrome.
The development of your COVID recovery
The content, and clinical assurance of all content has been provided by an expert advisory group, with the support of patients who have lived experience of COVID-19, their families and carers. Membership of the advisory group includes clinicians from cardiac and pulmonary rehabilitation services, allied health professionals and psychological services, and from the national respiratory working group and the national cardiac rehabilitation expert advisory group, of the national CVD-Respiratory programme.
Content has been developed and reviewed by representatives from:
- AbSent
- Association of Chartered Physiotherapists in Respiratory Care (ACPRC)
- Association for Respiratory Technology and Physiology (ARTP)
- British Association for Cardiovascular Prevention and Rehabilitation (BACPR)
- British Association of Parenteral and Enteral nutrition (BAPEN)
- British Cardiovascular Society
- British Dietetic Association
- British Geriatric Society
- British Lung Foundation/Asthma UK
- British Psychological Society
- British Rhinological Society
- British Society of Rehabilitation Medicine
- British Thoracic Society
- Chartered Society of Physiotherapy (CSP)
- Fifth Sense
- Ministry of Defence
- National Rehabilitation Association
- NHS England and NHS Improvement
- Physiotherapy for Breathing Pattern Disorders
- Physiotherapy Pain Association
- Primary Care Respiratory Society (PCRS)
- Royal College Occupational Therapists
- Royal College of Speech and Language Therapists
- Rehab Alliance channels (via CSP)
- UK Sepsis Trust
- University Hospitals of Leicester NHS Trust
- University of Leicester
- Vocational Rehabilitation Association UK (VRA)
Evidence of effectiveness
Whilst it is impossible to provide evidence of effectiveness of this particular platform for this novel disease, the approach to self-management via an online platform has been based on the successful implementation of two rehabilitation platforms also developed by University Hospitals Leicester; Activate Your Heart and SPACE for COPD.
Activate your heart
Initial data from Activate Your Heart (AYH) was analysed, with results showing
- Reduction in waiting times for patients accessing their education from 11 to 3 weeks.
- Patient choice increasing, with 65% who completed AYH stating that they would not have attended an out-patient programme.
- Initial assessment attendance improving from 44% to 57%, with completion rates at 73%.
- Over a four-week period, 15 hours of a band 6 cardiac rehabilitation professionals time was released.
- Cost savings were made; the AYH programme costs around £330 including initial and final patient assessments compared to £700 for conventional rehabilitation.
- There is the potential for readmissions to secondary cost to be reduced if more patients access cardiac rehabilitation programmes in a timely manner.
SPACE for COPD
The “Ready for Home” survey revealed that patients receiving the intervention reported feeling better able to arrange their life to cope with chronic obstructive pulmonary disease (COPD), knew when to seek help about feeling unwell, and more often took their medications as prescribed, compared to usual care (P<0.05). Healthcare professionals’ support was an essential factor for all patients; feedback on their progression was also described as an important facilitator to exercise.
Accessibility
An equality impact assessment has been carried out for Your COVID Recovery.
The following considerations have been given to accessibility:
- A paper workbook that replicates the content of the digital platform is being developed for people who do not have access to or who are unable to use the online platform.
- The platform has been reviewed by national leads for learning disability and/or autism to ensure good levels of accessibility for people with a learning disability and for people that need an easy read option. Changes will be made to the platform at its next refresh to improve accessibility further.
- The platform has also undergone a black, Asian and minority ethnic (BAME) group review.
- Options for the platform to be translated into other languages are being explored and will form part website refresh.
Patient cohorts
Anybody with COVID may develop ongoing post-COVID symptoms that warrant further assessment and support.
The patient cohorts are defined by NICE as:
- Acute COVID-19 infection
Signs and symptoms of COVID-19 for up to 4 weeks. - Ongoing symptomatic COVID-19
Signs and symptoms of COVID-19 from 4 weeks up to 12 weeks - Post-COVID19 syndrome
Signs and symptoms that develop during or following an infection consistent with
COVID-19 which continue for more than 12 weeks and are not explained by an
alternative diagnosis. The condition usually presents with clusters of symptoms, often
overlapping, which may change over time and can affect any system within the body.
Many people with post-COVID syndrome can also experience generalised pain,
fatigue, persisting high temperature and psychiatric problems.Post-COVID-19 syndrome may be considered before 12 weeks while the possibility of an alternative underlying disease is also being assessed.
Target population
The target population for the Your COVID Recovery platform is people with ongoing symptoms after an illness clinically indicative of COVID-19 or who have had a positive SARS-Cov-2 test, regardless of whether they were admitted for their acute illness or remained at home or in a care home.
The platform is suitable for people who can self-manage or who have somebody that can support them to access and use the platform, or who can use the paper manual as an alternative.
Your COVID recovery access and training for services and systems
Services that would like to offer their patients access to the Your COVID Recovery platform should contact University Hospitals Leicester NHS Trust at yourcovidrecovery@uhl-tr.nhs.uk in order to register their services onto the platform and to access the training materials in the form of a manual and a short presentation. Additional virtual training events will also be available which enable the referrer to look through the platform and access the modules the patient will work through. Technical support will be offered only to sites that have undertaken the virtual training.
Patient assessment
A face to face assessment and potentially diagnostic testing prior to referral is needed primarily to ensure that the ongoing symptoms a person reports are attributed to post-acute COVID and are not a consequence of a serious underlying condition.
Once the assessment has indicated that the patient has post-COVID syndrome, consideration should be given to whether the patient would benefit from specialist referral, from referral to existing rehabilitation services, or to the new post-COVID assessment clinics. Your COVID Recovery is an adjunct to these services and may be used as an adjunct to existing services or as a standalone supported self-management tool.
If referral to Your COVID Recovery is being considered there will need to be:
- Shared decision making with the patient about the suitability of the platform for them taking into account their readiness, ability and capacity to self-manage an online rehabilitation programme, and their ability to access a digital device to use online platform or their ability to use the paper manual.
Assessment of the inclusion and exclusion criteria defined by the University Hospitals Leicester NHS Trust and are based on The British Thoracic Society (2020) (Appendix A)
Decision to refer
Systems will have different services and pathways for managing people with post-COVID syndrome once the patient has been assessed to rule out non-COVID related conditions. There are a number of options for the next stage of assessment and referral to Your COVID Recovery. These include nominating a primary care network, virtual COVID ward/multidisciplinary team or community rehabilitation service to register with Your COVID Recovery and to be the point of further assessment and referral for the patient. These services would also provide the online monitoring and further support for the patient and carry out the post rehabilitation assessment. Communication with the patients GP would need to be maintained in the usual way.
Prior to referral the patient should complete a standardised 1 minute sit to stand test using pulse oximetry. Clinical judgement based on this test and the GP assessment should inform the healthcare professional whether the patient is suitable for self-management on Your COVID Recovery or whether they would benefit from referral to other rehabilitation, to other services or back to their GP.
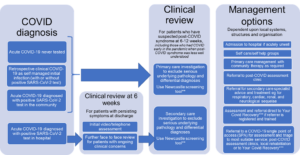
A proposed referral pathway consistent with the pathway in the NHS England and NHS Improvement guidance for the commissioning of post-COVID assessment clinics is outlined below:
Post COVID syndrome referral routes*
(subject to amendment further to NICE/SIGN/RCGP guidance publication)
Image showing Post COVID syndrome referral routes from COVID diagnosis to clinical review through to management options.
Clinical review includes assessment through to investigations.
Management options are dependent on local systems structures and organisation.
* Based on a pathway from the Royal College of General Practitioners House of Lords report (2020) . Pathway likely to be amended further to NICE/SIGN/RCGP post-COVID syndrome guideline publication.
**Newcastle post-COVID screening tool available the NHS England and NHS Improvement post-COVID assessment clinic commissioning guidance
***Your COVID Recovery is an online interactive platform for patients with post-COVID syndrome. Patient referral requires registration with yourcovidrecovery@uhl-tr.nhs.uk and a patient assessment that includes a 1 minute sit to stand test.
Referral
- A code for the patient to access the platform is generated by the healthcare professional via a separate part of the site. The code is emailed to the patient. The healthcare professional or the patient can create an account using this code.
- The clinician area enables the healthcare professional to view a dashboard for each patient so that they can monitor each patient’s progress and communicate online with the patient.
- At registration the system asks for additional information about the patient which can be inputted by the healthcare professional or the patient. This includes the 1-minute sit to stand test.
The patient completes a self-assessment on how COVID is affecting their wellbeing and daily life which becomes their ‘symptom thermometer’, one of the trackers that the patient will be able to access to monitor their progress.
Your COVID recovery platform content
There are 16 interactive programme modules that a patient self-select via the platform. These contain a range of videos, power points and reading for patients to undertake. These can be found in Appendix C.
- There are four stages to the programme. When a patient starts each stage, they will be asked to complete a series of tasks.
- At the outset this includes setting goals based on what’s important to the patient and taking an activity safety quiz.
- All information is added to the healthcare professional’s area on the site. From here, the professional can review and monitor the patient’s progress through the programme and communicate with the patient.
- As the patient moves through each stage of the programme, they are given a fresh set of tasks to complete.
- This includes looking at their goals and trackers to monitor their progress, together with signposting to resources and information on the symptoms and difficulties they may be experiencing.
- At the end of Stage 4, patients will be asked to review their goals and re-complete some of the tests they took at the outset to review their progress.
- There is a peer support network which is set up by local systems further to their registration and training. These networks will enable patients in a local rehab system to share experiences with one another and have elements of social support through their rehabilitation.
- Patients will be able to ask their referrer questions when engaged with the platform. Setting up this facility is also covered in the Your COVID Recovery training.
Information governance and data protection
All data is encrypted to AES-256 standard and is stored in University Hospitals Leicester data centre which is a hardened security environment. All data is encrypted during transmission and when stored in the database.
Further information
For further information in relation to the platform, please contact yourcovidrecovery@uhl-tr.nhs.uk.
Appendices
Appendix A
Your COVID Recovery rehabilitation criteria
* developed by University Hospitals of Leicester based on the British Thoracic Society (2020)
Inclusion criteria
- Age 16 or older
- Ambulatory with or without walking aids (no assistance)
- Independent with sit to stand
COVID related criteria - Symptom history suggestive of COVID-19 infection (fever, cough, fatigue or loss of smell/taste)
Or - Patients with persisting symptoms most likely due to COVID-19 but who didn’t require hospital admission. Many of these patients may not have been tested for COVID-19 and diagnosis will have been made on best clinical judgement. Other medical conditions that may present with similar symptoms will need to be excluded
- Patients presenting with respiratory symptoms with an in-patient stay +/- evidence of pneumonia
- Patients who had a prolonged hospital stay who received high flow of oxygen therapy or non-invasive ventilation
NB. For all COVID related symptoms other medical causes should be excluded.
Exclusion criteria
- Those with suspected active COVID-19 infection, particularly if COVID-19 was not confirmed during an initial influenza like illness
- Any new + ve COVID screen, applies to patients and those living in same household or in their ‘Bubble’. Review 14 days post initial onset of symptoms
- < 1/12 post COVID diagnosis (potential for transmission if virus remains active, as per present research findings)
- Patients admitted with COVID-19 but presenting predominantly with problems related to neurological, cardiac, renal, or polytrauma or other body systems. They may be better suited to alternative specific predefined rehabilitation pathways for rehabilitation e.g. complex neurological or stroke rehabilitation
- Patients presenting with COVID-19 with co-existent active cancer requiring treatment decisions and plans, would be best initially managed on the cancer pathway
- Patients with persisting rehabilitation need requiring in-patient multidisciplinary rehabilitation following a prolonged or severe hospital admission. The proposed rehabilitation detailed here does not replace this but may take place at a later date
- New onset of symptomatic palpitations
- History of falls / unexpected or more than 1 year requiring medical attention. Patients presenting with fall-related injuries should be referred to appropriate local falls prevention services
- Difficulty with walking and balance
- History of syncope
- Active neurological or psychiatric illnesses which prevent engagement with rehabilitation. (these may need to be addressed first)
- Known history of poorly controlled diabetes or hypertension.
- Any contra-indications absolute or relative to exercise training as listed below
- Had a cardiac event within the last 6 weeks
- Severe musculoskeletal or neurological disorders that limit mobility
- Severe psychiatric disorders
- Patients presenting a) from nursing homes, b) with severe frailty, c) in the end of life period and d) with overwhelming palliative care needs may not benefit from this rehabilitation intensity, nature and style and be better managed using alternative pathways
Appendix B
Platform modules
- Goal setting
- Swallow, voice and communication
- Nutrition
- Sleep
- Pain
- Breathlessness
- Cough
- Fatigue
- Fear and anxiety
- Mood and emotions
- Memory and thinking
- Getting moving again
- Muscle weakness
- Managing my day
- Return to work
NHS England and NHS Improvement
Skipton House
80 London Road
London
SE1 6LH
This publication can be made available in a number of other formats on request.
© NHS England and NHS Improvement
Publication approval reference: 001599