Analogue to Digital
The NHS is becoming more digitally accessible, with technology at the heart of how we deliver faster, more efficient and more personalised care.

Across the North East and Yorkshire, services are using innovation to improve both patient and staff experience. AI tools are helping free up clinician time. New digital phone systems are making it easier for patients to contact GP practices. Digital consultations, shared care records and smart data tools are creating a more joined-up and responsive system.
By putting digital tools at the centre of how we plan, deliver and manage care, we’re helping patients get the right support more quickly — and giving staff more time to focus on what matters most.
Explore how services across the North East and Yorkshire are evolving to improve outcomes, enhance access and strengthen care in the places people live.
▼ Getting the most out of the NHS App podcast
The NHS App plays a key role in the 10 Year Health Plan’s shift from analogue to digital, making it easier for people to manage their health and access services in one place. In this podcast, NHS App Head of Product James Higgott joins host James Butcher, alongside App Ambassadors from North East and Yorkshire, to talk about how the app is evolving and what features people find most useful. They discuss recent improvements such as easier login, ordering repeat prescriptions, checking test results, and how the app supports accessibility, including for people who are deaf. The conversation reflects how digital tools like the NHS App are helping to create a more modern, connected and user-friendly health service.
🎧 Listen now: Getting the most out of the NHS App
▼ Opening the Front Door to Care podcast
In this episode of the Transforming Primary Care podcast, a panel of NHS App Ambassadors are joined by Dr Shanker Vijay, GP and digital transformation lead in the London region, to discuss their work helping people make the most of the app. Together, they explore how the app is opening up access to health services, what primary care teams need to know about the tools available through it, and how ambassadors are supporting communities to understand and use its features.
🎧 Listen now: Opening the Front Door to Care
You can also read the full transcript here.
▼ Rollout of eCDR across CHFT, helping to release 58 days of trips to Pharmacy for colleagues
The rollout of our electronic controlled drugs register (eCDR) is now complete at Calderdale and Huddersfield NHS Foundation Trust, and is showing some fantastic results which is helping give colleagues more time back in the day for patient care. 
Every area in the Trust that dispenses controlled drugs is now using the system. eCDR is a software application, which means orders for controlled drugs (CDs) are sent using a computer to be prepared by pharmacy colleagues. Once the order is ready, the requester is notified and can then collect the order from the pharmacy department.
The trust are already seeing the benefits, including:
- Around 1,400 hours, or 58 days, of wasted trips (to and from Pharmacy) have been released back to nursing colleagues to give them more time to care.
- Orders are electronically sent overnight and are ready as soon as Pharmacy opens, a saving of 10 to 15 minutes each time an order is placed – that’s around 88 days.
- Completing audits is now quicker and the time taken on stock checking has also been reduced.
- There is improved compliance with CD documentation regulations and CQC compliance, as every transaction is signed and/or witnessed as required, without the ability to ‘cross out’.
- Processing and receipt back to the ward/department is quicker. Pharmacy can distinguish immediately all the order requirements e.g. patient’s own/urgent etc. This reduces delayed or omitted doses of CDs to patients.
▼ WYAAT implements data sharing software to support faster and more accurate diagnoses for patients across our hospitals
Five of WYAAT’s trusts can now see pathology and other diagnostic test results from across the region, using ICE OpenNet technology.
Clinicians working across five of our six trusts can now instantly access test results from across our WYAAT pathology network, following the successful roll-out of Clinisys’ ICE OpenNet.
Clinisys ICE OpenNet is an order communications and results reporting system that is used extensively in NHS hospitals and GP practices to enable clinicians to see pathology and other test results obtained at various NHS trusts.
Across WYAAT, ICE OpenNet has been used to link five of our six hospitals request and test result platforms, meaning consultants, nurses, and other clinicians can now view results from across the network: avoiding unnecessary repeat testing, saving print costs and time-consuming calls, and supporting better-informed patient diagnosis and treatment decisions. Airedale NHS Foundation Trust is expected to go-live with this software later in the year.
With the roll-out across our WYAAT trusts almost complete, the WYAAT pathology network is looking at how it can share results with neighbouring primary and community organisations and with the local shared care record, which includes data from a wider range of trust, GP, and local authority systems.
▼ How the NHS App helps people with hearing difficulties access NHS services
Emmanuel Chan, a Clinical Nurse Specialist in mental health services for deaf patients, is using his expertise to champion the NHS App as a powerful tool for empowering patients and improving access to care. From supporting digital transformation during the pandemic to leading research into how deaf communities engage with health technology, Emmanuel is helping patients and staff alike make the most of the NHS App. Read his full story — including how he works with carers, promotes uptake across teams, and supports inclusive innovation through the App Ambassador programme.
▼ Doncaster and Bassetlaw Teaching Hospitals has partnered with Annalise.ai to enhance diagnostic services.
Doncaster FT have used a system called Annalise.ai Head CT, to help triage and assess patients in their A&E department.
Doncaster currently outsource their head CT scanning when patients come in on a night. The CT images are sent to a company in Australia who assess the images and then send the results back to the clinicians in the UK.
The Annalise solution, using AI that has been trained on Head CT images, is able to assess the images and triage these cases based on their acuity.
Initial estimates from Doncaster suggest savings of around £250,000 per annum on this single use case.
▼ How Sheffield Health and Social Care NHS Foundation Trust has implemented a modern EPR system called RIO.
Sheffield Health and Social Care NHS Foundation Trust (SHSC) has implemented a modern Electronic Patient Record (EPR) system, Rio, as part of its vision to improve the mental, physical and social wellbeing of the communities it serves. This digital transformation marks a major step forward in standardising care, enhancing safety, and improving patient experience across the Trust.
Previously reliant on a bespoke EPR system that introduced significant process variation, SHSC migrated to Rio to simplify clinical pathways and reduce complexity. Over 1,000 separate assessment forms were reduced to around 100, with standardised care plans and risk assessments now used across all services. This has improved record consistency and enabled clinicians to deliver safer and more effective care.
The new EPR supports direct input of Patient Reported Outcome Measures (PROMs), guided by a chatbot, improving data quality and patient engagement. Clinicians can also access GP records directly through Rio, reducing delays and medication errors. The system includes strong cybersecurity features, such as smartcard authentication and comprehensive audit trails.
Usage data shows the impact: daily logins rose by up to 150%, PROMs submissions increased by 220%, and access to GP records grew by 234% after launch. This increased engagement reflects improved clinician confidence and more efficient working.
The implementation process was collaborative, involving staff across the organisation and incorporating lived experience through service user involvement in co-designing key features, including care plans. This ensured the system met both clinical needs and user expectations.
Rio now provides a foundation for future digital integration, including participation in the national Shared Care Record and the Federated Data Platform. This will enable more joined-up care, support the ‘Home First’ model, and empower patients through the NHS App.
A lessons-learned event in June 2025 highlighted the project’s successes and challenges. NHS England has expressed interest in using SHSC’s experience as a national case study to support other trusts on similar journeys.
▼ How AI at Sheffield Teaching Hospitals NHS Foundation Trust is predicting kidney failure six times faster than expert human analysts

Sheffield Teaching Hospitals NHS Foundation Trust has developed and implemented a ground-breaking artificial intelligence (AI) tool that predicts kidney failure in patients with autosomal dominant polycystic kidney disease (ADPKD) six times faster than traditional manual methods. Used in specialist kidney clinics, the tool provides rapid and highly accurate analysis of total kidney volume, a key predictor of future kidney lifespan, by automating the segmentation of MRI scans that would otherwise take up to an hour per patient to complete manually. Trained on hundreds of kidney images by Principal Scientist Jonathan Taylor and refined with input from radiographers and clinicians, the AI now delivers results in under a minute.
Professor Albert Ong, Consultant Nephrologist and Clinical Lead for Genetics, emphasised the importance of this advancement, particularly for ADPKD patients who often reach kidney failure by age 50 and require urgent dialysis or transplant once deterioration begins. Already in use at Sheffield’s 3D Lab since 2022, the technology has potential for global rollout, especially in clinics lacking specialist imaging expertise, marking a major step forward in accessible, precision-driven renal care.
▼ Cutting the Wait: How Digital Messaging Transformed Physiotherapy at Friarage Hospital
A digital innovation led by Senior Specialist Physiotherapist Linda Furness at Friarage Hospital has drastically reduced physiotherapy waiting lists by over 80%. In response to a post-COVID backlog that left nearly 800 patients in Hambleton and Richmondshire waiting for care in early 2024, the team implemented a simple yet highly effective solution using Communication Annex software.
By replacing postal appointment letters with a two-question SMS, asking patients if they still required treatment and if they could attend at short notice, the service streamlined booking processes, reduced administrative strain, and allowed patients to confirm appointments within minutes. This change brought the waiting list down to just 152 patients within a year. The system’s impact is demonstrated by patient Stephen Brooks, who was contacted four days after elbow surgery and seen by a physiotherapist within 14 days of his injury, and applauded the new approach taken by Linda and her team.
They not only maintained the process consistently over the year but also trained staff and introduced a satisfaction survey to monitor ongoing improvements. The result is a more responsive, patient-friendly service that is delivering care faster and more efficiently.
More information can be found on the trust’s website: Physio’s effective change cuts waiting list by more than half – South Tees Hospitals NHS Foundation Trust
▼ ‘World first’ as Newcastle uses AI to predict how burns will heal
Newcastle Hospitals NHS Foundation Trust has become the first in the world to trial a groundbreaking artificial intelligence tool, DeepView, to predict how burns will heal—offering clinical teams vital insight in less than a second. Developed by Spectral AI, the technology combines multispectral imaging with AI to assess wound depth on the first day of injury, well before traditional methods like laser doppler imaging, which typically require a 48-hour wait. 
Deployed at the Royal Victoria Infirmary’s Northern Regional Burn Centre, the system has already been used in more than 100 adult cases, delivering high-quality, portable imaging directly to wards and theatres.
Consultant Burn Surgeon Mr Christopher Lewis praised the tool’s speed and diagnostic value, having shared the centre’s pioneering experience at an international burns conference. With global interest already growing, this world-first deployment not only enhances decision-making for burn care in Newcastle but has the potential to revolutionise early treatment strategies for burns patients around the world.
More information can be found on the trust’s website: ‘World first’ as Newcastle uses AI to predict how burns will heal – Newcastle Hospitals NHS Foundation Trust
▼ Ambient Voice Technology
Ambient Voice technology is a sophisticated AI system designed to enhance communication and documentation in clinical settings. This technology allows for automatic transcription of conversations between clinicians and patients, ensuring accurate and efficient documentation.
Modality are a Supergroup of GP practices that operate across the country, with a large presence in West and East Yorkshire. The recently adopted an ambient voice solution called Heidi.
Heidi has grown in popularity due to its simple and effective used and aggressive pricing and marketing. Modality have adopted the use of Heidi in clinical consultations with patients, where the system helps to capture the notes from conversations between the clinician and their patient. These notes are then presented back to the clinician for review and insertion into the patients record.
Estimated savings from other studies, indicates that ambient voice technologies may result in upwards of 16% efficiency gains for the clinician.
▼ Rollout of a powerful new AI solution across WYAAT
West Yorkshire Association of Acute Trusts (hospitals across West Yorkshire and Harrogate)
WYAAT is leading the national rollout of a powerful new AI chest X-ray solution designed to speed up lung cancer diagnosis and improve patient outcomes.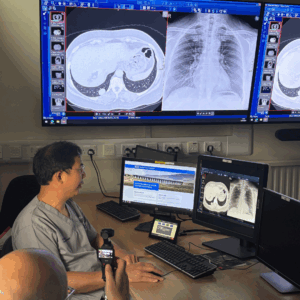
Developed by Annalise.ai and funded through NHS England’s AI Diagnostics Fund, the software can detect up to 124 potential findings in under a minute, providing clinicians with annotated images to support quicker and more accurate decision-making.
With around 400,000 chest X-rays taken across the YIC trusts each year, the tool acts as a “second pair of eyes,” helping to prioritise urgent cases and enabling earlier intervention for conditions like lung cancer, where early diagnosis increases the five-year survival rate twentyfold.
The system is now live across all of our WYAAT trusts:
- Airedale NHS Foundation Trust
- Bradford Teaching Hospitals NHS Foundation Trust
- Calderdale and Huddersfield NHS Foundation Trust
- Harrogate and District NHS Foundation Trust
- Leeds Teaching Hospitals NHS Trust
- Mid Yorkshire Teaching NHS Trust

Dr Daniel Fascia, Clinical Lead for YIC, praised the initiative for reducing diagnostic delays and tackling backlogs exacerbated by the pandemic. The deployment is part of a broader transformation of imaging services, with national leaders, including Peter Kyle MP, hailing it as a vital step in harnessing innovation to save lives across the NHS.
▼ University of Sheffield/NIHR
AI is already demonstrating its potential. There is already significant application to support people with depression and anxiety. Without it, the default for many patients in accessing mental healthcare is ‘trial and error’: they try several therapies in the pursuit of one that actually works, extending distress and delaying recovery. Funded in part by Mindlife UK and supported by the National Institute for Health and Care Research Clinical Research Network, investigators led by the University of Sheffield have developed a pioneering artificial intelligence tool that helps NHS professionals personalise treatment plans for patients with depression, improving recovery outcomes and speeding up care. Tested through a three-year clinical trial involving over 900 patients across Lancashire, Rotherham and Doncaster, the tool demonstrated significantly improved outcomes for stratified care over standard stepped care, albeit at an additional cost. This is an early example of the potential for AI to deliver clinical benefits in mental health services.
▼ RAIDR: Rethinking Readiness for Surgery
A clinically led collaboration in the North East has developed the RAIDR platform, an innovative digital tool that integrates patient health information from surgical waiting lists with primary care records into an interactive dashboard accessible to anaesthetists and other secondary care clinicians. This platform enables preoperative assessment teams to visualise the health profiles of all patients awaiting surgery and identify opportunities to enhance their health before the procedure. It also facilitates the risk stratification of patients to optimise the use of low-risk pathways.
Currently, targeted support is provided through the North East and North Cumbria Waiting Well programme, which includes initiatives such as opioid deprescribing, weight management, and intensive support for better diabetes management, alongside addressing wider determinants of health and well-being. These efforts significantly reduce the likelihood of surgery cancellations or postponements, improve the management of long-term health conditions, and bolster preventive health strategies. This is particularly important as patients at higher risk often face socioeconomic challenges or belong to protected groups, underscoring the program’s commitment to equity in healthcare access and outcomes.
Since the Waiting Well programme started 20,000 people have been contacted to offer targeted support, and more than 4,100 people have accepted an offer of support. For those who eligible for the targeted support, the programme has a public-facing website called Get Set For Surgery, which is the ‘universal offer’ from the programme which can be used by anyone who is waiting for surgery or treatment.
▼ Staff time savings and more surgeries for patients in North Cumbria
The shift from analogue to digital is changing how the NHS delivers care, making services faster, more connected and more efficient. At North Cumbria Integrated Care NHS Foundation Trust, the Federated Data Platform is helping staff save time, improve coordination and ensure more patients receive the treatment they need. With a near real-time view of waiting lists, clinical teams can prioritise patients more effectively and work together to manage care from referral to recovery.
▼ Robotic surgery boosts precision and recovery at North Tees
Digital innovation is transforming surgical care in the NHS. North Tees and Hartlepool NHS Foundation Trust has introduced its first surgical robot to support patients needing knee replacement surgery. The ROSA robotic assistant helps surgeons plan and carry out procedures with greater precision, leading to better outcomes and faster recovery. The investment is part of the trust’s surgical hub development, supporting more efficient, high-quality care for patients.
▼ Training Tomorrow’s Surgeons: Bradford Leads the Way in Robotic Innovation
As part of the shift from analogue to digital set out in the 10 Year Health Plan, Bradford Teaching Hospitals NHS Foundation Trust is helping to equip the future surgical workforce with the digital skills they’ll need. The Trust recently hosted the first regional robotic surgical skills event for trainee surgeons across Yorkshire, showcasing how precision robotics and digital tools are enhancing care. Robotic-assisted procedures allow for greater accuracy, faster recovery, and better outcomes for patients — and by investing in training today, the NHS is ensuring tomorrow’s clinicians are confident in using these technologies to deliver safer, more personalised surgery.
▼ DAISY the Robot: Scarborough Hospital Trials AI to Support Faster, Smarter Triage
Could a robot help patients get seen faster in A&E? That’s what Scarborough Hospital is exploring through DAISY, a new AI-powered triage system being piloted in its emergency department. Developed in partnership with the University of York, DAISY helps patients take their own vital signs and answer symptom-based questions, producing a clinical summary for staff to review. It’s designed to support and not replace medical staff, freeing up time and helping to prioritise care more effectively. The pilot reflects the ambitions of the 10 Year Health Plan’s digital shift: harnessing innovation to streamline services, improve outcomes and ease pressure on frontline teams.
▼ Airedale Empowers Cancer Patients with New App to Support Personalised Care
Airedale NHS Foundation Trust is supporting the 10 Year Health Plan’s shift from analogue to digital with the rollout of the Careology app for cancer patients. The app gives patients an easy way to track symptoms and side effects, manage their medications, and receive appointment reminders using their own device. It also allows clinicians to monitor this information in real time, helping them spot signs of deterioration earlier and provide timely support. Family members and caregivers can access the app too, helping coordinate care and communication. By offering more personalised, proactive support outside hospital settings, the initiative aims to improve patient experience and reduce unnecessary admissions. It’s a clear example of how digital tools are helping to modernise care and make services more responsive, connected and centred around individual needs.
This shift is transforming how people interact with the NHS, from managing prescriptions and appointments to accessing advice and test results on the go. The NHS App will become the main way people organise and manage their care, with features like 24/7 support, personalised health tools and direct access to approved digital services.
By 2028, every patient will have a secure, single digital health record that can be accessed across the NHS. This will make care safer, faster and more coordinated and will help staff spend less time on admin and more time with patients.
