Access to national workforce supply routes for PCN groupings
Contents
- 1. Introduction
- 2. Workforce deployment model
- 3. National workforce supply routes
- 4. Onboarding and engagement
- 5. Indemnity and insurance
- Appendix 1: Workforce deployment model
- Appendix 2: Drawdown process
- Appendix 3: PCN health and safety guidance
Classification: Official
Publication approval reference: C1392
COVID-19 vaccination programme
Version 3 , 18 August 2021
Updates since version 2 (published 14 January 2021) are highlighted in yellow.
This guidance is correct at the time of publishing. However, as it is subject to updates, please use the hyperlinks to confirm the information you are disseminating to the public is accurate.
If you have any queries about this workforce guidance, please contact PCNPO.WorkforceEscalation@nhs.net.
1. Introduction
General practice continues to have a significant role in the roll-out of the COVID-19 vaccination programme, working with other providers in their primary care network (PCN) grouping to ensure coverage for the local population.
The national workforce supply routes have been established to provide additional capacity over and above local workforce teams. The routes allow PCN groupings to access both clinical and non-clinical staff and volunteers, via a designated lead organisation in each integrated care system (ICS).
This guidance sets out detailed instructions which PCN groupings will need to access the national workforce supply routes, on the following key points:
- overall approach to workforce capacity planning for COVID-19 vaccination
- roles and responsibilities of organisations within the proposed workforce deployment model
- additional workforce that may be available from national workforce supply routes, including the proposed drawdown approach
- onboarding and engagement arrangements, including indemnity and insurance.
Where PCN groupings are mentioned in this document, we are referring to practices that collaborate to deliver the services under the ES, which may include established PCNs, and additional neighbouring practices and/or other groups of practices working together. Practices within the PCN grouping must have signed a collaboration agreement, to work together as a joint enterprise and the patients who attend for COVID-19 vaccinations will attend what is deemed to be a temporary single medical practice, for the purpose of regulation 3(8)(b) of the Human Medicines Regulations 2012. Where lead providers are mentioned in this document, we are referring to the lead organisation regarding workforce supply within the ICS, which may be referred to locally as a lead employer, workforce bureau, or some other alternative.
2. Workforce deployment model
To support PCN groupings, this guidance provides additional information on the processes to access and onboard additional workforce.
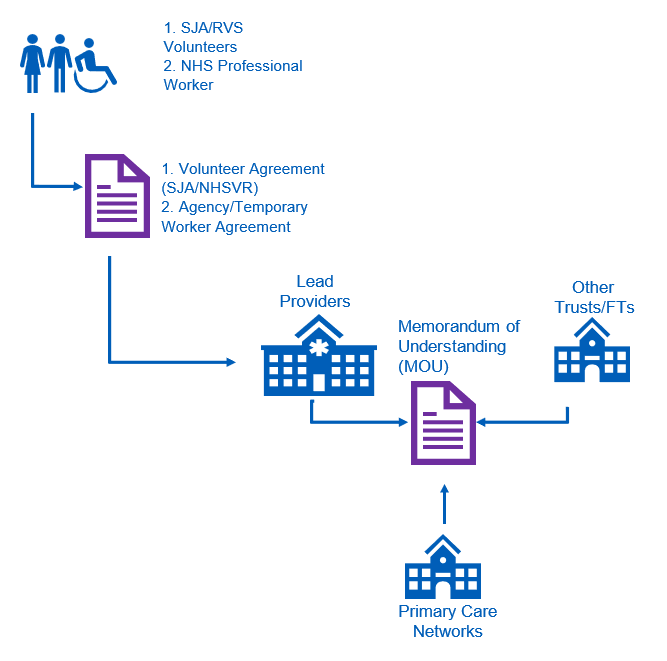
The workforce deployment model depends on a number of allocated responsibilities for PCN groupings, clinical commissioning groups (CCGs) and appointed lead providers in each ICS. A visual diagram of the workforce deployment model for the national workforce supply routes can be found in Appendix 1.
Responsibilities of PCN groupings
PCN groupings should review this guidance in their planning for COVID-19 vaccination. As mobilisation continues, PCNs should continue to identify their staffing requirements and future workforce gaps, as well as put in place contingency arrangements for staff absence. PCNs should contact the lead provider in their area for additional support and to access additional staff resource, via the national workforce supply routes.
It is important to note that within this document it is not possible to take account of the complexity and variety of service delivery arrangements across PCN groupings. Therefore, it is not intended for this guidance to replace local decision-making within a PCN, from either the perspective of an employer or a provider. Moreover, arrangements between PCNs and lead providers regarding support will be agreed locally and the purpose of this guidance is to provide more information on the likely arrangements to be implemented locally.
Responsibilities of CCGs
It is expected that CCGs will provide local workforce mobilisation and support to PCN groupings, facilitating the utilisation of resources and expertise available locally.
Responsibilities of lead providers
Each ICS has a designated lead provider which will act as a workforce hub for the other providers in the local area, including PCN groupings.
The lead provider will work with all providers (including PCN groupings) to provide workforce support, such as:
- Communications with local providers and PCN groupings.
- Completion of regional workforce reporting.
- System-level workforce planning and gap analysis.
- Liaison and drawdown of national workforce supply routes.
- Management of rostering systems (for volunteer or national workforce supply routes).
- Oversight and delivery of statutory and mandatory training.
The exact balance of responsibilities between lead providers and other providers (including PCN groupings) will be agreed locally in line with the needs and resources of the system.
The lead provider can also provide support to PCN groupings on local recruitment, and subject to a local agreement, such as a memorandum of understanding (MOU) being in place, may be able to employ additional staff on behalf of the PCN grouping.
An updated list of named contact details for the lead provider in each ICS has been shared with PCN groupings to enable planning and liaison to take place.
Finally, although outside the scope of this guidance, it is important to note that other healthcare providers, for example community pharmacy or dental providers, may also be able to support with workforce supply, through a sub-contracting arrangement, which should be locally agreed and funded through the PCN grouping.
3. National workforce supply routes
PCN groupings will be supported to access the nationally sourced pools of staff and volunteers on a similar basis as other providers.
| Supplier | Overview of support to be provided | Roles provided by supplier | Contracting route |
|---|---|---|---|
| NHS Professionals (NHSP) | NHSP recruited a large number of staff, registered and non-registered and is responsible for the end-to-end process, from managing centralised demand to recruitment, virtual training and confirming employment hosting arrangements. More details are available here. |
|
Commissioned sites will be able to make requests for additional staff via their lead provider and put in place a collaborative agreement with them. The sites will be required to fund these posts locally through Agenda for Change pay rates. To access resource, LVS should follow the drawdown processes for the national workforce supply routes, listed in Appendix 2 |
| St John Ambulance (SJA) | SJA will manage and deploy volunteers to vaccination sites, including vaccinators. This is available across all seven regions. More details are available here. |
|
Commissioned sites can make requests for additional volunteers via their lead employer and put in place a collaborative agreement with them. Commissioned sites will not be required to fund these staff locally. To access resource, providers should follow the drawdown process for the national workforce supply routes, listed in Appendix 2 |
| Royal Voluntary Services (RVS) | The NHS Volunteer Responders programme, delivered by Royal Voluntary Service and the GoodSAM app, provide volunteers for non-clinical volunteering roles such as stewarding. The system lead provider identifies volunteers needed. |
|
Commissioned sites can make requests for additional volunteers via their lead employer and put in place a collaborative agreement with them. Commissioned sites will not be required to fund these staff locally. To access resource, providers should follow the drawdown process for the national workforce supply routes, listed in Appendix 2. |
| Occupational Health (OH) Providers | Multiple OH providers can provide additional registered OH professionals. |
|
An existing framework is in place with 23 suppliers for NHS organisations to access additional OH provider support. Commissioned sites can make requests for additional staff via their lead provider and put in place a collaborative agreement with the lead provider but will be required to fund these posts locally. |
Practices will have to locally fund the cost of paid clinical and administrative staff sourced from national providers (such as via NHS Professionals or Bring Back Staff) on the agreed Agenda for Change pay scales for the job role, but voluntary staff will be provided at no charge to the PCN grouping. Role descriptions are available from lead providers for volunteers provided by St John Ambulance and the NHS Volunteer Responders, or for temporary workers recruited by NHS Professionals. Where PCN groupings decide to undertake local recruitment themselves or subcontract from other providers, they are not required to use national job descriptions.
It is important to note that incorporation of these supply routes or roles as part of a PCN grouping’s proposed vaccinating team is not mandatory. Local alternatives may be available to provide additional capacity, such as through the use of additional hours worked by existing staff, sub-contracting arrangements or working with other providers such as out of hours services. As with the seasonal flu programme, practices within their PCN groupings are also encouraged to work with their CCG and local volunteer organisations. The local staffing model chosen must depend on local workforce characteristics and the need to maintain safe staffing and clinical supervision arrangements. The clinical lead of the PCN site providing the COVID-19 vaccination service is responsible for ensuring that appropriately trained and competent staff are in place to deliver the services.
4. Onboarding and engagement
Where PCN groupings identify a workforce need that cannot be filled locally, they can seek to secure workforce via the national workforce supply routes. This section sets out the responsibilities of both lead providers and PCN groupings under these arrangements.
A COVID-19 vaccination programme overview pack for staff and volunteers will be used to support onboarding and will be provided to volunteers from St. John Ambulance, NHS Volunteer Responders, as well as workers being engaged by NHS Professionals.
Lead providers should:
- Provide the face-to-face training required and assure themselves of other training and programme induction provided, using appropriate competency assessment and training needs analysis.
- Undertake assurance of pre-employment checking and occupational health clearance.
- Ensure the volunteers and temporary workers have appropriate uniform for their assigned role.
- Put in place appropriate rostering to support the needs of the PCN groupings.
- Take lead responsibility for health and safety, but this is delegated to the PCN/practice for site-specific health and safety and onboarding.
- Follow normal engagement processes, including the completion of a volunteer agreement for volunteers or an honorary contract for staff. An example volunteer agreement is supplied for local providers to review and adapt for local use.
- Put in place a collaborative agreement or MOU between the lead provider and the PCN grouping to facilitate sharing of volunteers and staff among both PCNs and other NHS providers. An example MOU is supplied for local providers to review and adapt, if necessary. Where staff or volunteers are assigned onwards to another NHS provider or PCN grouping, there should be no need for an additional local agreement at each site, provided that an appropriate MOU is in place.
PCN Groupings should:
- Assure themselves of the competency and performance of staff and volunteers deployed to a designated site.
- Raise any volunteer or temporary workers performance issues with the lead provider.
- Ensure that NHS volunteer responders do not work with vulnerable persons or children, unless in a fully supervised capacity.
- Deliver an ‘on-site’ orientation and induction, in line with local procedures. This should normally include the following key information:
- site welcome
- satisfactory identity verification of deployed volunteer or worker
- access to IT and workstation assessment
- explanation of site flow
- induction to operating procedures
- supply of site-specific personal protective equipment (PPE)
- confirmation of completion of all training requirements
- completion of legal documentation to enable administration of vaccine, eg signing of Patient Group Direction or National Protocol (where appropriate)
- confirmation of named site contact for any queries and the clinical supervisor contact for any concerns
- local health and safety instructions (eg fire safety); further detail on the local site responsibilities for health and safety are outlined in Appendix 3.
5. Indemnity and insurance
The Clinical Negligence Scheme for General Practice (CNSGP) provides clinical negligence indemnity cover for all staff engaged by a GP practice under the CNSGP regulations. It covers NHS activities delivered by a Part 4 contractor under a primary medical services contract (including an NHS standard contract with Schedule 2L – Provisions Applicable to Primary Medical Services), a Primary Medical Services sub- contractor or the provision of ‘Ancillary Health Services’ for a Part 4 contractor or Primary Medical Services sub-contractor such as a Local Enhanced Service.
The COVID-19 vaccination enhanced service is nationally agreed and as such is considered primary medical services for the purposes of cover under CNSGP. A national tripartite letter has been produced which sets out the indemnity arrangements for the vaccination programme and can be accessed here.
NHS Resolution has also uploaded FAQs to its website to support PCN groupings to understand the indemnity and insurance requirements. These can be found here.
Appendix 1: Workforce deployment model
Appendix 2: Drawdown process
Volunteers deployed from the national workforce supply routes
- PCN groupings should contact the lead provider for their ICS to place a request for volunteers.
- The request must include the nature of the roles requested (eg clinical vaccinator/non-clinical volunteer), the time period requested, the details of the vaccination site, including a site contact.
- The lead provider will work with the national providers of volunteers and identify suitable candidates.
- The lead provider will assign these volunteers to the PCN grouping and communicate where a request cannot be covered.
- Once the volunteer is assigned, the lead provider will ensure the training requirements of the role are fulfilled and confirm the shift with the volunteer.
- The lead provider will then pass the details of the volunteer to the PCN grouping for local site onboarding. An MOU (or local equivalent, such as a collaborative agreement) is required to be in place to facilitate the sharing of staff from the lead provider to other providers.
- The PCN grouping will ensure that the volunteer is met on site at the start of their shift, so that local site onboarding can be completed.
- If there are any issues regarding the volunteer placement, the PCN should escalate these to the lead provider.
Temporary workers deployed from the national supply route
- PCN groupings should contact the lead provider for their ICS to place a request for temporary workers from the national workforce supply.
- The request must include the nature of the roles requested (eg clinical vaccinator/non-clinical worker), the time period requested, the details of the vaccination site and a site contact.
- The PCN grouping must undertake to pay the lead provider for the total cost of workers successfully placed with the PCN grouping. This can be agreed by parties agreeing to an MOU (or local equivalent, such as a collaborative agreement).
- The lead provider will work with the national provider of temporary workers (NHS Professionals) to identify suitable candidates.
- The lead provider will assign temporary workers to the PCN grouping and communicate where a request cannot be covered.
- Once the temporary staff member is selected, the lead provider will assure themselves that the training requirements of the role are fulfilled and confirm the shift with the volunteer.
- The lead provider will then pass the details of the assigned temporary staff to the PCN grouping for local site onboarding. An MOU (or local equivalent) is required to be in place to facilitate the sharing of staff from the lead providers to other providers.
- The PCN grouping will ensure that the temporary worker is met on site at the start of their shift so that onboarding can be completed.
- If there are any issues regarding the placement of temporary worker, the PCN should direct these to the lead provider.
- The lead provider will invoice the PCN grouping, in line with the relevant local agreement or MOU.
Appendix 3: PCN health and safety guidance
The practice/PCN, on behalf of the lead provider shall:
- Provide information in connection with any risks to health and safety involved in the assignment, including high-risk areas where exposure prone procedures take place, as well as the PCN policy for mitigating such risks.
- Be responsible for the health and safety, fire safety and security of volunteers or workers on the PCN site which shall include, provision of fire safety instruction and ensuring fire safety equipment is in place.
- Provide volunteers or workers with all necessary personal protective equipment to undertake the tasks required.
- Undertake the necessary risk assessment where the proposed volunteer or worker is known to be at potential individual risk, including, without limitation, by being pregnant.
- Inform the lead provider of all outbreaks of infection, as declared by the practice or PCN.
- Inform the lead provider where a volunteer or worker is injured, infected, or attacked.
- In the event of a Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013 (RIDDOR) reportable incident, PCNs must inform the lead provider immediately, who will liaise work with the practice/PCN to prepare an incident report.
- The PCN shall comply with all statutory obligations applicable to it in relation to volunteers or workers assignments, including without limitation those arising under the Health and Safety at Work Act 1974, the Employment Rights Act 1996, the Management of Health and Safety at Work Regulations 1999 and the Working Time Regulations 1998.
