Accessing medicines for detainees released during COVID-19
Contents
- Introduction
- Accessing medication on release from prescribed places of detention
- Prescribing and access to GP or hospital specialist prescriptions
- Repeat prescriptions
- Community pharmacy services
- Controlled drugs / substance misuse medicines
- How do people access paracetamol and other symptomatic relief?
- How do patients access urgent medicines without a prescription?
- References
- Appendix 1: Template letter to enable a representative to collect medicines on behalf of a patient in isolation
Publications approval reference: 001559 / C0281
A guide for the probation service and youth offending teams (YOTs) and other support workers
29 September 2020, Version 2
Introduction
This is a guide to support probation and youth offending teams and other teams supporting people released from custody on accessing medicines and pharmacy services during the COVID-19 outbreak.
The key web-sites for information about COVID-19 are shown in the references on page seven. These are updated daily and will need to be regularly checked for relevant information.
Accessing medication on release from prescribed places of detention
NHS England and NHS Improvement directly commission healthcare and pharmacy services within prisons, immigration removal centres, and the children and young people secure estate which includes young offender institutions for people under 18 years, secure training centres and secure children’s homes.
Usually, people released from prison and other detainees released from custody are given at least seven days supply of medication or a prescription (ie FP10 or FP10MDA) they can have dispensed at a pharmacy. During COVID-19, health and justice (HJ) providers may increase the quantities supplied on release to up to 28 days and provide FP10MDA prescriptions for substance misuse treatment for 14 days. However, if releases are unplanned or due to a reduction in prescribing and pharmacy services for HJ, some people may be released without a supply of their medicines or a prescription.
To prevent medicines shortages, pharmacies are not ordering excess medication and GPs are discouraged from prescribing higher quantities than 28 days’ supply. It is essential that you discourage your clients from requesting more medicines than they would usually receive or need.
People who are self-isolating and need to evidence this can do so by accessing a letter on- line via NHS 111. This means they no longer need to get a letter as evidence from a GP. Information about this is available here.
There is an NHS App for patients to use if they have a smartphone or tablet. The App allows people to:
- book appointments – search for, book and cancel appointments at their GP surgery, and see details of their upcoming and past appointments
- order repeat prescriptions – see their available medicines and request a new repeat prescription
- check their symptoms – search trusted NHS information and advice on hundreds of conditions and treatments, and get instant advice or medical help near to where they are
- view their medical record – securely access their GP medical record, to see information like their allergies and their current and past medicines.
Prescribing and access to GP or hospital specialist prescriptions
It is important that detained people who are not registered with a GP, register with one as soon as possible after their release so the GP can provide prescriptions. Registration via online consultations is being provided as described in national primary care guidance. This also has information about how practices can register a homeless person. Temporary registration with a GP may be possible if the detained person is released on a temporary licence or to a temporary location.
During COVID-19, many GP services are asking patients to call before they attend or request registration. It is important to ensure that detainees call the GP before going to the surgery or practice as they may be refused entry because of social distancing measures.
GPs may be using remote consulting services such as video or telephone conferencing to speak with patients. At the end of this type of consultation the GP may electronically send a prescription straight to a pharmacy meaning the patient will not have to go to the GP surgery to collect a prescription.
Please note that most GP surgeries use electronic transfer of the prescription using the Electronic Prescription Service (EPS) rather than paper prescriptions. These electronic prescriptions can be dispensed at any community pharmacy or the patient can nominate a specific pharmacy for it to be sent to. More information about the EPS service is available here.
If a released person is having medicines that are usually supplied by the hospital, for example HIV or Hepatitis C medicines, they will need to contact the hospital specialist as soon as possible to make arrangements for follow up care and prescriptions.
Repeat prescriptions
When a released person asks the GP for a repeat prescription for medicines prescribed in custody, the GP may need information from the HJ healthcare team to confirm this request before they can supply the prescription. If released people are given information about their medicines and health needs by the releasing site, it is important that this is given to the GP as quickly as possible to avoid delays in care.
Repeat prescriptions can take several days to be issued and dispensed by the pharmacy. This means ordering the prescription at least seven days before the current supply runs out. This is why people released from custody should register with a GP or contact the GP promptly to request their repeat prescriptions, as the GP will need to spend additional time verifying the medicines needed.
GPs are being encouraged to use electronic repeat dispensing (eRD) to improve how patients can collect repeat prescriptions for long-term conditions where the patient is stable, ie the medication regime is unlikely to change for the period of time prescribed for. This service involves the GP issuing a batch of electronic prescriptions that can be supplied by
the community pharmacy each month for a set number of months. This means the patient doesn’t need to request a repeat prescription from the surgery each month. Note that most controlled drugs cannot be prescribed using eRD. The GP or community pharmacist will have more information about how this works for their patients. There is also information available here.
The NHS App now has a new feature that allows patients to view and change their EPS pharmacy nomination. Being able to update nominations in the NHS App means patients can more easily choose the pharmacy that is right for them during the COVID-19 pandemic and beyond. The NHS App team at NHS Digital have been working on this development for some time, but its release has been prioritised to help patients and primary care teams better cope with ordering and obtaining prescriptions during the pandemic.
Having a pharmacy nomination in EPS removes the need for patients to collect prescriptions from GP practices and drop them off at a pharmacy, supporting the public to observe social distancing. The pharmacies download their nominated prescriptions regularly during the week and this assists them to have the medications ready for collection, rather than patients having to wait for the medicines to be dispensed. It is also intended to help reduce the nomination-setting burden on pharmacy teams and GP practices during this busy time. To nominate a distance selling pharmacy (DSPs), patients must register with the pharmacy through their website or contact them directly. This is because DSPs normally need to collect additional information on patients that are nominating their pharmacy beyond simple demographic data, so they are able to provide an appropriate service when the first nominated script arrives for the patient.
Community pharmacy services
Community pharmacies have received a letter from NHS England and NHS Improvement providing them with information about released prisoners and other detainees add link.
Usual opening hours for pharmacies can be checked here. However, there are new arrangements in place that give pharmacies some flexibility in the hours in which they need to open to the public during the COVID-19 pandemic.
Specifically:
- If under significant pressure, at the discretion of the pharmacist, pharmacies may close their doors to the public for up to 2.5 hours a day, including lunch.
- Community pharmacies are expected to be open to the public, and not working behind closed doors, between 10.00am-12 noon and 2.00pm-4.00pm as a minimum (if these are contracted core or supplementary hours).
- Similarly, 100 hours pharmacies should be open and not working behind closed doors from 10.00am-12 noon and 2.00pm-6.00pm as a minimum.
A sign on the door must give information about how to contact the pharmacy if urgent help is needed.
Prescriptions issued from a prison or young offender institution when individuals are released are exempt from charge (this is because the practice address shown on the prescription has the prefix ‘HMP’). Unless the person is exempt from prescription charges, any further prescriptions issued by a GP, hospital or other community services will hav e to be paid for. Guidance about prescription exemption for prisoners who are released on temporary licence during COVID-19 is expected from Her Majesty’s Prison and Probation Service (HMPPS).
The NHS prescription charge is currently £9.15 for each prescribed item, which means that there is a charge for each different drug or medical appliance on your prescription. A prescription prepayment certificate (PPC) could save money for people needing more than four medicines in three months or 12 medicines in 12 months. These can be bought from the NHSBSA.
A community pharmacy home delivery service during the COVID-19 outbreak is being commissioned from community pharmacies to ensure delivery of medicines to eligible patients who should not present in a pharmacy. This is delivered locally based on local lockdown restrictions and applies to specific patients.
Controlled drugs / substance misuse medicines
During this time, it is not expected that the community services for drug and alcohol services will close, however, they may reduce the number of face-to-face sessions that they offer. It is important that you contact these providers to receive their advice on making appointments and accessing medicines.
The arrangements for prescribing and dispensing of medications, including methadone and buprenorphine may change due to pharmacy closures, staff unavailability and patients having to self-isolate or maintain social distancing. For example, supervised consumption services and daily collections will increasingly be reserved for the most vulnerable people. The local community substance misuse providers will have information about their plans for this.
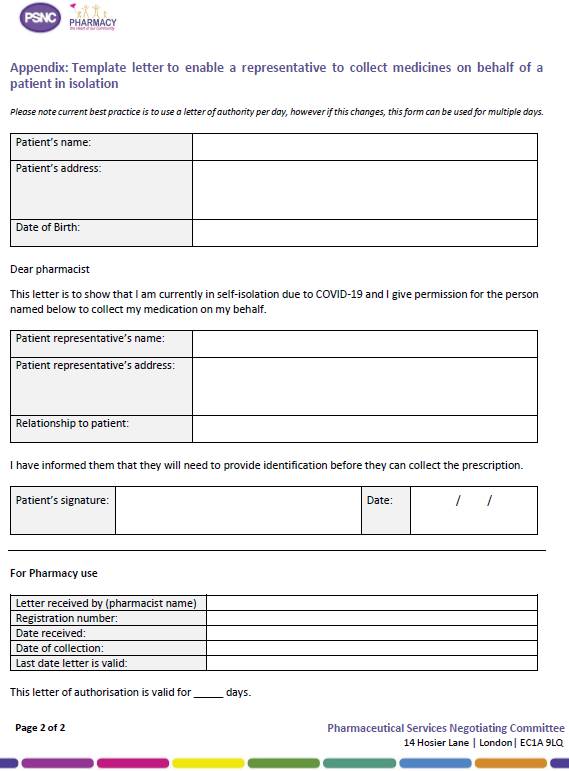
If a person is self-isolating and is already under the care of a drug and alcohol team or receiving a controlled drug for other treatments (eg pain or ADHD medicines), they may need to provide a letter to the pharmacist to allow a nominated- duly authorised person to collect their medication for a controlled drug. The person will need to take identification to the pharmacy. An example of the letter can be found in Appendix 1. This letter can be used for clients who are on daily, and other collections of their medicines. If a letter can’t be provided to the pharmacist, the keyworker cannot request the pharmacy supply the medicine to another person as this authorisation must come from the patient. The pharmacist will need to check that the request from the patient is valid by:
- speaking to the client’s key worker and/or prescriber to confirm they are aware that the client is self-isolating and that a nominated person is collecting their medicines
- asking the client to call the pharmacy and confirm who is collecting their medicines.
If people are self-isolating and have medication at home, it is very important to make sure that medication is kept out of sight and reach of children.
How do people access paracetamol and other symptomatic relief?
Pharmacies, supermarkets and other retailers should be tried first as some stock is available. If supplies cannot be sourced from these outlets, pharmacies are providing paracetamol to specific patients by packing down supplies usually used to dispense prescriptions for paracetamol. This route should only be used where the need for symptomatic relief is urgent due to COVID-19symptoms (GPhC, 2020).
How do patients access urgent medicines without a prescription?
Every effort should be made via the GP or out of hours (OOH) services to obtain a prescription as this is the safest option. Please note that a GP OOH service will only prescribe medicines liable to misuse in limited circumstances and will not usually prescribe medicines such as methadone or buprenorphine. People should avoid going to accident and emergency to request medicines.
There are two options (as set out below) for people who need an urgent medicine, but who are unable to obtain a prescription before they run out. Neither of these will allow a supply of CDs under current legislation.
1. NHS Community Pharmacist Consultation Service (CPCS) – via NHS 111
The NHS Community Pharmacist Consultation Service (CPCS) was launched by NHS England and NHS Improvement on 29 October 2019, to progress the integration of community pharmacy into local NHS urgent care services, providing more convenient treatment closer to patients’ homes. The CPCS offers patients the option of having a consultation with a pharmacist following an initial assessment by an NHS 111 call handler. The call handler can make a digital referral to a convenient pharmacy, where the patient can receive advice and treatment for a range of minor illnesses or for an urgent supply of a previously prescribed medicine.
Community pharmacies will be using telephone consultations with people where possible rather than face to face consultations. Through their conversation with the patient, it may be appropriate to advise the patient not to go into the pharmacy, and to complete the NHS CPCS referral via telephone. Some patients may need access to over-the-counter medicines to support self-care for minor illness or to pick up an urgent supply of their usual prescription medicines and so it might be appropriate to discuss how they are delivered or if a friend, relative, carer or community volunteer is able to collect them. Should the patient need to be escalated or referred to an alternative service, the pharmacist can arrange this.
This service is continuing during COVID-19 and in addition to calling NHS 111, NHS 111 Online urgent medicines supply service now makes CPCS referrals to community pharmacies where people need urgent access to their usual prescribed medicines. The current legislation does not allow emergency supplies of controlled drugs Schedules 2&3 but will allow up to five days of Schedules 4&5 via NHSCPCS.
2. Emergency supply using current legislation or NHS commissioned services if a GP practice is closed
Legislation, including legislation triggered by the COVID-19 pandemic, allows community pharmacists to supply urgent medicines under specific circumstances. In an emergency, a community pharmacist can supply prescription only medicines (POMs) to a patient (who has previously been prescribed the requested POM) without a prescription at the request of the patient using medicines legislation. Normally, an emergency supply of medicines is undertaken as a private service, at a cost to the patient or as part of the NHS Community Pharmacist Consultation Service requiring referral from NHS 111 (see above). In some locations, local commissioned NHS services allow the supply of medicines and appliances at NHS expense under arrangements where the pharmacist deems that the patient has a need for the medicine during the temporary closure of their GP practice during COVID-19. The current legislation does not allow emergency supplies of controlled drugs. More information about emergency supplies for controlled drugs can be found here.
References
GPhC. (2020, March 31). Q&A: Coronavirus. Retrieved from Q&A: Coronavirus: https://www.rpharms.com/about-us/news/details/Packing-down-paracetamol
NHS. (2020, March 28). Coronavirus (COVID-19): Symptoms and what to do. Retrieved from Coronavirus (COVID-19): Symptoms and what to do: https://www.nhs.uk/conditions/coronavirus-covid-19/symptoms-and-what-to-do/
NHS. (2020, March 27). NHS. Retrieved from Advice for everyone Coronavirus (COVID-19): https://www.nhs.uk/conditions/coronavirus-covid-19/
NHS England. (2020, March 31). Novel Coronavirus (COVID-19) Standard Operating Procedure. Retrieved from Community Pharmacy: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/Novel- coronavirus-COVID-19-standard-operating-procedure-Community-Pharmacy-v2- published-22-March-2020.pdf
NHS England. (2020, March 31). Preparedness letter for community pharmacy: 19 March. Retrieved from Updates and Guideance: https://www.england.nhs.uk/coronavirus/wp- content/uploads/sites/52/2020/03/preparedness-letter_primary-care_community- pharmacy-19-march-2020.pdf
PSNC. (2020, March 31). What doe sthe patient pay? Retrieved from NHS Prescription Charge: https://psnc.org.uk/dispensing-supply/receiving-a-prescription/patient- charges/
Public Health England. (2020, March 27). Coronavirus (COVID-19): What is social distancing. Retrieved from publichealthmatters: https://publichealthmatters.blog.gov.uk/2020/03/04/coronavirus-covid-19-what-is- social-distancing/
RPS. (2020, March 31). Packing Down Paracetamol. Retrieved from Packing Down Paracetmaol: https://www.rpharms.com/about-us/news/details/Packing-down- paracetamol
Appendix 1: Template letter to enable a representative to collect medicines on behalf of a patient in isolation