Advice on acute sector workforce models during COVID-19
Contents
- 1. Foreword
- 2. Maintaining acute services
- 3. Meeting the workforce requirement for the Phase 3 response
- Annex 1 Staffing enhanced and critical care services
- Annex 2: Medical workforce planning and deployment to support surge service delivery: HEE support
- Annex 3: Potential groups of staff to provide critical care nursing
- Annex 4: Redeployment of healthcare science staff to support critical care, high dependency units and those on oxygen therapy
- Annex 5: A framework for organising the allied health professions acute sector workforce to meet the Phase 3 COVID-19
- Annex 6: A framework for organising the acute sector pharmacy workforce to meet the Phase 3 COVID-19
Classification: Official
Publication approval reference: 001559 / C0833
10 December 2020
This guidance has been developed by NHS England and NHS Improvement with Health Education England.
1. Foreword
At the end of July, we asked local NHS systems to prepare for Phase 3 by:
- planning to restore all urgent and routine services
- delivering extensive flu (and in due course COVID-19) vaccination programmes
- managing the expected second surge in COVID-19 infections, now here and recognised in the decision to return the NHS to the highest level of emergency preparedness (level 4) from 5 November.
This document was developed by NHS England and NHS Improvement with Health Education England to provide an advisory framework to help support trusts to organise their workforce in a way best suited to deliver their Phase 3 plans and can be flexed to local circumstances, resources and demand. It is, of course, still for individual employing organisations and trusts to make appropriate decisions about staff models and care.
With the need to maintain acute, elective and screening services as far as possible, as well as the future pipeline of staff, the significant workforce boost to critical and acute care from redeploying staff from elective and outpatient services as well as trainees and students is not available this time, unless COVID-19 demand is extremely high.
Local systems are moving to expand critical care and enhanced care capacity so they can continue to deliver non-COVID-19 acute services and major surgery, as well as having enough capacity to meet their projected COVID-19 demand.
This advisory framework includes updated guidance on acute sector staffing for both COVID-19 and non-COVID-19 areas, taking into account learning from the first surge.
We are very grateful for the contribution all NHS staff are making during this difficult time. We want to help local systems support staff through this winter, both for their own health and wellbeing and that of their patients.
Professor Stephen Powis | National Medical Director | NHS England and NHS Improvement
Ruth May | Chief Nursing Officer for England
Professor Mark Radford | Chief Nurse, Health Education England and Deputy Chief Nursing Officer for England
Professor Wendy Reid | Executive Director of Education and Quality and Medical Director | Health Education England
2. Maintaining acute services
Key actions for acute providers
- Assess the clinical workforce required for services needed over winter, both in acute hospitals and expansion facilities, taking account of advisory guidance (included here) on critical care. Funding has been allocated to regions to support time for training additional staff for new roles in critical or enhanced care.
- Deliver additional workforce supply from the sources identified (including Bringing Back Staff regional hubs and NHS Professionals).
- Embed ongoing risk assessments as part of workforce planning and ongoing discussions with staff.
- Maintain the health and wellbeing of the whole workforce, working with staff-side bodies at all levels of the system to secure a consistent provision of practices and services that support this: https://www.nhsemployers.org/covid19. Local case volumes and mix, skill mix, establishment levels and absences due to sickness and self-isolation are likely to fluctuate rapidly during the acute phase of the second COVID-19 surge.
This section sets out learning from Wave 1 alongside the expectations and challenges around maintaining and restoring non-COVID-19 services for the teams which are most involved in supporting COVID-19 services.
Emergency department (ED) team
ED teams are adapting to deal separately with patients who have suspected or confirmed COVID-19 infection and patients with other emergency conditions. All major specialties should identify a consultant, as first on call, to offer rapid senior specialist advice to the ED team and to help minimise avoidable emergency admissions.
The Care Quality Commission (CQC) has published Patient FIRST, an online resource to help ED teams, trusts and the wider system to build on the positive changes from the first peak of the pandemic. For example, EDs may find it useful to route minor injuries elsewhere, eg to the fracture clinic, with appropriate staff support.
Adult ward teams
Medical staffing on non-COVID-19 wards should be kept at a level that maintains patient safety and optimises patient flow with regular input from senior decision-makers and support from a coherent wider professional team. Infection prevention and control (IPC) precautions (including twice-weekly asymptomatic staff testing and patient PCR tests on admission, at day 3, and day 5 and prior to care home discharge) are key to reducing the risk of transmission of COVID-19 infection from asymptomatic carriers to patients and staff and may be more challenging to maintain in the general wards and during activities such as shift handovers. Multidisciplinary teams (MDTs) should continue to meet, potentially remotely, to maintain high quality care and enhance patient flow through the system.
Respiratory team
The respiratory needs of COVID-19 and non-COVID-19 patients are different, and the nursing, medical and allied health professions (AHPs) support required will depend on patient acuity, the level of monitoring required and likelihood of deterioration (which may be higher for COVID-19 patients on respiratory support than COPD patients established on enhanced pharmacological and ventilatory support such as steroids and NIV).
All such patients should be assessed on admission and on a regular basis by a competent respiratory or acute medical practitioner, and cared for in the ward environment providing the safest available care (eg acute medical unit, acute respiratory unit, enhanced care unit, or high dependency or intensive care unit). Critical care outreach services (or similar) should be available to support rapid escalation of care if required.
Respiratory teams will also need to focus on respiratory outpatients and diagnostics to prevent avoidable acute respiratory presentations. To allow respiratory teams to focus on both areas, it may where feasible be appropriate to consider removing respiratory teams from the acute general internal medicine rota and backfilling from colleagues in other specialties.
Theatre teams
In some cases, elective surgery can be delivered at hub sites away from COVID-19 ‘hot’ areas. Full use should also be made of the contracted independent sector. High volume, low-risk planned surgery is an area where professional staff returning to practice through the Bringing Back Staff hubs are likely to be able to contribute and free up current surgical staff for acute work. Consultant surgeon triage of patients presenting to ED with possible emergency surgical conditions has been shown to enable a significant proportion of these to be managed without need for admission.
Theatre teams should be set up with consistent staffing where possible since this enhances productivity, patient safety and staff wellbeing. Anaesthetists are a key staff group for elective and emergency surgery and intensive care; therefore, their careful deployment is crucial. Supporting and enabling other professionals such as operating department practitioners (ODPs) and anaesthetic associates to work to the top of their licences will be important.
Imaging team
Imaging management teams will advise individual hospital trusts and regional teams on the current status of staffing levels, waiting times and acute and non-acute services. Working in close partnership with other regional sites potentially offers access to dedicated COVID-19 and non-COVID-19 (‘clean’) imaging sites in the event of a surge in COVID-19 cases. Many trusts have supported increased use of remote image reporting by radiologists unable to work on acute sites where there is a risk of COVID-19 infection.
Palliative and end of life care teams
This team will need to cover the whole hospital – wherever possible, segregated into sub-teams covering COVID-19 areas and non-COVID-19 services. It should be led by consultants in palliative medicine, supported by specialist nurses, chaplains and AHPs. These teams may require additional capacity drawn from other relevant areas, including elderly care and oncology.
Renal team
All renal providers should seek to identify a designated team for their COVID-19 response, including as a minimum a nurse lead, a medical lead and managerial support. They should be responsible for managing the day-to-day response, including collating data on staffing and availability of dialysis sessions. A separate clinical leadership team may be identified to liaise with critical care facilities across their catchment population.
Renal networks should provide a workforce plan for the network and to the COVID-19 regional management team. This should include measuring staffing absence and resilience, planning mutual aid within region between providers, and consider staff passporting to allow transfer of individuals between facilities (independent sector and NHS). The plan should have a clear escalation and de-escalation structure. A distinct element of workforce planning should cover support to critical care.
Providers should identify available nursing and other healthcare professionals capable of supporting dialysis sessions. Dialysis-competent staff should wherever possible not be redeployed from providing dialysis. Providers should review their overall workforce and wherever possible where appropriate reduce non-clinical activity to release staff time into dialysis facilities. Home dialysis programmes should be maintained and ongoing staff training accelerated. Lead providers should discuss staff deployment across their facilities to allow redeployment of staff and maintain activity.
3. Meeting the workforce requirement for the Phase 3 response
Overview of hospital care for COVID-19 and non-COVID patients
Acute care will continue to be provided at different levels and staffing ratios, depending on individual patients’ needs. Patients admitted to level 3/intensive care with COVID-19 have complex treatment requirements. However, clinical models for the care of the severely unwell COVID-19 patient have evolved with experience. Treating clinicians are deciding to manage a higher proportion of hospitalised patients on acute wards with respiratory support linked to developments in clinical understanding of the disease, proven therapeutics (eg steroids) and earlier detection of deterioration in the community leading to earlier hospital admission. These should mean that proportionately fewer level 2 and level 3 beds may be needed. Demand should also be reduced through the rapid take-up of virtual wards, in which people with COVID-19 in the community have regular remote monitoring, including assessment of their blood oxygen saturation.
This framework offers an approach to workforce, based on the best evidence currently available, to improve the management of and outcomes for hospitalised patients with severe COVID-19. The general approach centres on matching staffing to individual patients’ clinical needs, taking a ‘whole-hospital’ approach and systems-level approach to workforce, patient safety and outcomes. Mitigations in extreme circumstances will also need to include load-sharing approaches at regional and national levels.
Critical care (intensive and high dependency care) and enhanced care
Almost half of all critical care admissions are for the care of patients after major surgery. Local systems are planning to continue as much major surgery as possible through the winter to minimise impact on non-COVID-19 services. Many of these patients do not require advanced organ support and can instead be treated by enhanced care services, where the indicative nurse:patient ratio does not require 1:2 (level 2) or 1:1 (level 3), and a skills and competency approach to staffing is recommended.
Mutual aid between sites and organisations should be used before any dilution of intensive care staff; this includes considering moving staff (in teams) as well as patients. The rapid development of adult patient transfer services was a success in Wave 1 and supports mutual aid approaches.
Enhanced care can safely be provided with tailored staffing ratios for specific indications. This approach, in particular, may support the care of both COVID-19 and non-COVID-19 high acuity patients without an absolute indication for critical care admission. Adopting these distinct approaches during the pandemic will enable clinical care to be delivered more equitably, as well as aligning more closely to patient needs.
Based on experience during Wave 1, intensive care units (providing level 3 care) believe they will provide the best care and best support and staff wellbeing if they plan to maintain staffing ratios at a minimum of one critical care nurse to two level 3 beds (compared with the normal one-to-one ratio), supported by the MDT approach. A system-level approach will be required to support these staffing principles and to enable units to be decompressed to support patient safety, staff wellbeing and maintenance of COVID-19 compliant pathways for non-COVID-19 care.
Trusts and regions should estimate the number of surge beds they will provide and then seek to deploy an appropriate number of suitable other staff to receive basic critical care training via either the ESICM C19 SPACE academy or similar local initiatives. Funding has been allocated to regions to support time for training staff for new roles in critical or enhanced care. Reducing disruption to high priority non-COVID-19 services is essential; measures to prevent this include seeking to:
- avoid over-reliance on anaesthetics/theatre staff for surge capacity
- avoid deployment of respiratory and critical care specialists for anything other than these roles
- use critical care resources as efficiently as possible – for example, by implementing enhanced care perioperative services or acute respiratory units.
The exact arrangements for staffing expanded critical care and the triggers for stepping down elective work will need to be determined by trusts and local systems and agreed with regions. They should consider scale, location and layout of surge capacity. However, in principle advice is that the following staffing ratios should not be exceeded unless local and regional mutual aid options have been explored and exhausted and escalated appropriately:
- bedside trained critical care nurses to level 3 patients – 1:2 (see below)
- bedside registered nurses – 1:1 (including both core critical care staff and surge capacity staff)
- senior clinician: patient ratio – 1:15 (including both core critical care consultants and surge capacity staff)
- middle-grade staff to patients – 1:8 (including both core critical care and surge capacity staff)
- in addition to bedside nurses, on each shift there should be at least one co-ordinating nurse (or more, depending on the level of surge) and staff allocated to support data capture (sitrep and ICNARC case-mix programme for all surge areas); healthcare assistants or medical support workers will also be required to act as runners and support bedside nurses
- in surge conditions, in addition to senior medical staff providing direct patient care, there may need to be at least one co-ordinating consultant on each shift (or more, depending on the level of surge); they will be required to co-ordinate admissions and discharges across all units within the hospital and support decision-making about transfers and mutual aid with systems and/or regional colleagues.
Additional workforce supply
Regional ‘Bringing Back Staff’ hubs hold details of available additional staff. Local systems should where possible seek to address a COVID-19 surge by augmenting the workforce before considering redeployment, so that routine services are maintained as far as possible.
Local critical care networks may offer mutual aid so that staff, or (where clinically appropriate) patients, might be moved between sites to balance supply and demand. The interim COVID-19 digital staff passport should help staff move temporarily to another organisation to provide mutual aid.
Guidance is available for existing and returning staff deployed into new clinical roles and environments. As part of this, relevant staff should have undergone a risk assessment and been asked if they are satisfied with the mitigations in place.
Organisations should proactively look at the percentage of higher risk staff in their workforce to enable accurate modelling of workforce deployment in different scenarios. Augmenting acute and critical care services to meet projected local COVID-19 demand will often mean bringing together new teams. It will be important to provide appropriate induction and recognise the knowledge, skills and expertise of individual staff so each person’s contribution can be optimised and factored into workforce planning.
Staff returning to professional work after an absence will usually have been assessed to determine the appropriate level for them to work at before they are deployed (see NMC guidance for temporary registration). Some of these returners will be suitable to work at a senior level; others, particularly those out of practice for some time, may be better placed at a more junior level, such as a healthcare support worker or a medical support worker. Here is guidance on the latter role.
Helping staff to support critical care
Rostering should seek to ensure staff groups do not exceed recommended weekly working hours and they have sufficient time for rest and recovery between runs of shifts.
Anaesthetic capacity will be under particular pressure, so it will be important to enable anaesthetists to focus on what only they can do and rapidly train other staff to provide support services such as proning. Redeployment of anaesthetic trainees into ITU should aim to focus on senior trainees whose learning will not be interrupted as a result. For more information see the Royal College of Anaesthetists guidance on managing a second surge.
Trusts should identify the surge workforce as early as possible, to provide adequate time and access to resources for training and preparation, with the aim of achieving the best possible patient outcomes and support to staff. Before deployment into critical care, time should be allowed both for formal training and also for at least two shifts of supernumerary work shadowing fully trained intensive care staff. Funding has been allocated to regional nursing directorates to distribute to their trusts, to support staff time for this training.
Staff who move into critical care from another service should do so voluntarily. They should receive basic critical care training and should be prepared for the role by staff who know the realities of working in critical care, helping the redeployed person make a valid and informed choice. If staff are adequately prepared and redeployed voluntarily, this promotes the potential for growth and resilience. Colleagues redeployed into critical care will require closer supervision (for both patient safety and personal safety/welfare reasons), and ideally supervisors should be trained in active listening. When redeployed staff return to their normal roles, they should be given a chance to reflect on their work, thanked properly and actively monitored by their receiving supervisors. This should include being given the opportunity to discuss their mental wellbeing to check for long-term issues. Funding has been allocated to regional nursing directorates for distribution to trusts to support health and wellbeing of the workforce in critical, enhanced and acute respiratory care.
For medical staff, HEE has a hierarchy for determining their readiness to manage ventilated patients. More generally, doctors – as all other healthcare staff – should work as part of a multiprofessional and multispecialty team and may need to provide care for patients in a specialty in which they have no recent experience. Teamworking, effective induction, clinical supervision and support will therefore be essential to maintain patient safety. Additional training may be needed for this to happen safely for both staff and patients. HEE regional teams will support discussions on induction standards and training for clinical teams based on feedback from Wave 1. The postgraduate dean should be involved in any decision to redeploy doctors in training.
We know from Wave 1 that the redeployment of trainees must be reviewed regularly to support the educational needs of the workforce and allow doctors in training to continue to learn and to support other services. The same considerations apply to the postgraduate training of nurses, midwives and AHPs (eg district/school nursing, health visiting and PHE-related programmes).
For registered nursing staff, guidance covers categorisation of the potential groups available to care for critically ill patients.
The NHS Nightingale model makes detailed assumptions for bed:staff ratios and covers large numbers of other staff groups. For healthcare scientists the relevant information is in Deploying the HCS Workforce to Support COVID-19. The relevant information for AHPs and the pharmacy workforce, is here. The workforce required in full-time equivalent (FTE) terms that these ratios generate also depends on assumptions for the following variables. These will need to be tested against emerging data from local daily absence recording:
- shift length and frequency (eg 12.5 hours, two shifts per day)
- working week hours (eg maximum 48 hours on average) and seven-day working
- contingency for sickness/isolation/and other absence (eg 20% core ICU, 30% other).
Maintaining as far as possible the education and training of healthcare students and trainees is important to protecting future supply of trained healthcare staff.
In extreme situations, HEE will also act regionally to boost the numbers of healthcare workers, with a focus on those not currently in clinical practice:
- by asking doctors currently out of training programmes if they can return to the front line
- by working with medical schools to enable students to support healthcare provision within their competencies through additional working in healthcare assistant level roles, which do not affect their studies
- postgraduate deans will work at regional and system level to enable short-term surge responses, while ensuring that any decisions to move trainees take account of other regional and local surges which are also affecting clinical demand, staff sickness and total workforce availability. The doctor in training’s learning needs, stage of training and progression must be part of this decision-making.
The Nursing and Midwifery Council (NMC) has withdrawn the emergency standards for students from 30 September and published new recovery standards to support students, education and training.
Annexes
Annex 1 Staffing enhanced and critical care services
Overarching principles for critical care staffing
The following principles will require local adaptation to take into consideration the scale of surge, location and layout of surge critical care capacity, and how level 2 care (including non-invasive ventilation) and enhanced care (particularly postoperative) is to be provided.
The tables that follow provide guidance on staffing surge capacity, taking into consideration the need to maintain elective services where possible, provide safe staffing for critically ill patients and protect staff wellbeing. The principles for surge capacity nurse/patient and doctor/patient ratios have been described above. Outreach services will need to be strengthened as critical care demand increases.
Enhanced perioperative care model
Enhanced perioperative care (EPC) provides postoperative support for patients at high risk of complications. It is not a substitute for critical care and should not be used to routinely treat patients at immediate risk of deterioration. It is a bridge between normal ward care and critical care, which is of value to patients who require enhanced monitoring and support without complex interventions.
Patients who have been risk-assessed as being increasingly likely to develop complications may benefit from a short stay (up to 48 hours) in an enhanced care facility. Such patients would include, for example, those with postoperative 30-day mortality risk estimated at >1% using a validated system, patients undergoing specific types of high risk surgery, or patients who require specific interventions (eg management of complex pain or CPAP for obstructive sleep apnoea). The Faculty of Intensive Care Medicine and Centre for Perioperative Care has published guidance for the development and implementation of enhanced perioperative care services.
Enhanced perioperative care provides protocol-driven care which is then applied to meet individual patient needs. The exact interventions and protocols used are at local discretion. Typical nurse/ patient ratios are no lower than 1:4, with a multidisciplinary approach to ensuring the right skills are available to patients at all times. Critical care departments would normally be expected to be part of the governance of enhanced care services, although the care may be delivered predominantly by other professional groups.
Enhanced care has an important role to play in the support of high risk surgical patients at all times, but particularly during surges in emergency activity. Ringfencing enhanced care beds to support COVID-compliant pathways for surgical patients may reduce potential disruption to surgical services and prevent cancellation of major operations. In extreme surge, they could be used to provide additional critical care capacity.
Respiratory support unit model
Respiratory support units (RSUs) enable enhanced respiratory support to be delivered on respiratory wards outside the critical care environment. The capacity required will vary depending on the local circumstances around service models, oxygen flow capabilities and, in particular, critical care capacity. RSUs could provide higher level acute care for COVID-19 patients, predominantly using CPAP and high flow nasal oxygen therapy (HFNOT), as well as non-invasive ventilation (NIV) to non-COVID-19 patients.
The COVID-19 pandemic has highlighted the benefit of RSUs, when the use of CPAP, and in some acute providers (depending on oxygen flow rates) HFNOT, has meant that critical care admission can be reserved for patients requiring ventilatory support, and some hypoxaemic patients recover without the need for mechanical ventilation.
The needs of these patients are more intense than normal ward patients, requiring enhanced nursing, medical, AHP support and monitoring, an ability to respond to rapid deterioration and to escalate to critical care where agreed as part of the advanced care planning. However, they may not require the level of nursing or other support that intensive care patients do, particularly CPAP patients, who may not require regular arterial gas sampling, for example.
Such patients should be assessed on admission and on a regular basis by a respiratory specialist with experience and competence in managing non-invasive forms of respiratory support, and when advanced respiratory support is needed, cared for in the respiratory ward environment which provides the safest available care. Critical care outreach services (or similar) should be available to support rapid escalation of care if required. Careful consideration must be given to admission and discharge criteria, particularly considering the need for RSU versus level 2 care.
Support from renal services for critical care
During Wave 1 many renal services supported critical care to deliver renal replacement therapy, while continuing to maintain usual dialysis services. The main workforce pinch point was the pool of dialysis-capable nurses who provide the majority of dialysis activity in centres.
In anticipation of possible similar pressures in future, a critical care support plan should be developed by a designated leadership team with both renal and critical care input. It should consider the following elements:
- Reduce burden on critical care facilities by ensuring end stage renal failure patients who do not require critical care are repatriated as a matter of priority.
- Ensure people with single organ renal failure are moved from critical care to renal service inpatient beds as soon as possible.
- Consider whether medical staff with relevant competencies can be redeployed to support critical care. This includes both doctors in training and substantive posts.
- Provide regular advice to support the management of people requiring renal replacement therapy based on the clinical need of the patient and maximising resource utilisation.
- As part of implementing the Tier 1-3 renal critical care plan (see appendix to adult critical care service specification), consider training critical care nurses or redeploy dialysis unit nurses, technicians and medical support to provide renal replacement therapy. In the case of redeployment, staff should be appropriately screened and supported.
Adult critical care transfer services
The inter-hospital transfer of critically unwell patients may be needed to balance system and network capacity and decompress units under greatest operational pressure. Some regions have, or are rapidly developing, adult critical care (ACC) transfer services which require additional staff experienced in the delivery of critical care. Each transfer service requires at least one duty consultant on each shift who can provide regional co-ordination, triage and decision support as well as remote medical advice to transfer teams. Transfer teams consist of two appropriately trained and experienced staff (middle or senior-grade doctor and a practitioner, usually with critical care nursing or ODP background). The National Model for ACC Transfer Services provides more detail and is available from regional leadership teams and critical care operational delivery networks. During high levels of surge, it may be necessary on a risk-assessed basis to consider the utilisation of ambulance service resources (such as critical care paramedics) combined with appropriately experienced doctors.
Table 1: Example staffing ratios for intensive care* and tiered step-down of interventional services: nursing staff**
| ICU capacity | Other activity | Trained critical care nurse: patient ratio | First tier registered nurses*** or AHPs with critical care experience or who have had recent basic training (eg ESICM C19 space training) | Second tier of registered nurses who have undergone recent basic training | Registered nurses or other staff with transferable skills to critical care (eg ODPs, recovery nurses) | Healthcare assistants or clinical support workers |
| Within baseline | BAU maintained | 1:1 | Not used except for supernumerary training | Not used except for supernumerary training | Not used except for supernumerary training | Used as per normal staffing guidelines on unit |
| Baseline + up to 25% | First step-down | Not lower than 1:1.25 | Not lower than 1:5 | Not used except for supernumerary training | Not used except for supernumerary training | Not lower than 1:10 |
| Baseline + up to 50% | Second step-down | Not lower than 1:1.5 | Not lower than 1:6 | Not used except for supernumerary training | Not lower than 1:6 | Not lower than 1:5 |
| Baseline + up to 75% | Third step-down | Not lower than 1:1.75 | Not lower than 1:3.5 | Not used except for supernumerary training | Not lower than 1:7 | Not lower than 1:5 |
| Baseline + up to 100% | P1 and P2 services only | Not lower than 1:2 | Not lower than 1:4 | Not lower than 1:8 | Not lower than 1:7 | Not lower than 1:5 |
| Baseline + up to 150% | P1 and P2 services only | Not lower than 1:2 | Not lower than 1:4 | Not lower than 1:4 | Not lower than 1:4 | Not lower than 1:5 |
| Baseline + up to 200% | P1 and P2 services only3 | Not lower than 1:2 | Not lower than 1:4 | Not lower than 1:4 | Not lower than 1:4 | Not lower than 1:5 |
*Intensive care = level 3 care. Similarly, staffing ratios and skill mix could be adapted in surge conditions for level 2 (high dependency) care where staffing ratios are usually 1:2 trained nurse: patients (such units therefore in surge might be considered for 1:3 or 1:4 trained HDU nurses: patient ratios, supplemented by other qualified nurses to maintain a bedside ratio of 1:2. Exact staffing arrangements will depend on patent acuity and skill-mix of staff. Establishing and communicating processes to achieve prompt review and escalation of care are essential for working under both normal and surge conditions.
**At least one senior nurse will be required in addition to bedside nurses as a shift leader (and more as numbers increase beyond baseline establishment)
***Nursing staff brought into critical care should be selected on a volunteer basis and with consideration as to which elective services will be stepped down in sequence.
Table 2: Example staffing ratios for intensive care* and tiered step-down of interventional services: medical/advanced critical care practitioners
| ICU capacity | Other activity | Middle grade – anaesthesia or ICM trainee on core rota. Staff: patient ratio | Additional middle grade with recent ICM training or basic introductory ICM training on surge rota – clinician: patient ratio | Senior grade (training critical care consultant) – on co-ordinating duty:** clinician: patient ratio | Senior grade (trained critical care consultant) on core rota: clinician: patient ratio | Senior grade (senior staff with recent experience in critical care – eg anaesthetist, surgeon or physician with HDU experience/ ESICM training) on surge rota – clinician: patient ratio |
| Baseline | BAU maintained | 1:8 | Not used except for supernumerary training | – | 1:10 | Not used except for supernumerary training |
| Baseline + up to 25% | First step-down | 1:8 | 1:8 | 1:25 – non-resident | 1:15 – non-resident | 1:10 – non-resident |
| Baseline + up to 50% | Second step-down | 1:8 | 1:8 | 1:30 – resident | 1:15 – resident | 1:15 – resident |
| Baseline + up to 75% | Third step-down | 1:8 | 1:8 | 1:35 – resident | 1:15 – resident | 1:10 – resident |
| Baseline + up to 100% | P1 and P2 services only | 1:8 | 1:8 | 1:40 – resident | 1:15 – resident | 1:10 – resident |
| Baseline + up to 150% | P1 and P2 services only | 1:8 | 1:8 | 1:50 – resident | 1:15 – resident | 1:10 – resident |
| Baseline + up to 200% | P1 and P2 services only | 1:8 | 1:8 | 1:60 – resident | 1:15 – resident | 1:10 – resident |
*Intensive care = level 3 care. Where possible, trusts should seek to create separate enhanced care units for green surgical patients, and acute respiratory units for stable patients requiring non-invasive ventilation. These units will require lower nurse: patient ratios – see https://www.ficm.ac.uk/enhanced-care/enhanced-perioperative-care for further details.
**Coordinating consultant may have responsibility for outreach, coordinating admissions/discharges, liaison between units within hospital and with external systems/regional/national colleagues (e.g. for mutual aid, transfers etc.)
Annex 2: Medical workforce planning and deployment to support surge service delivery: HEE support
Guidance on the support available from HEE is at: www.hee.nhs.uk/covid-19/information-doctors-training-october-2020-onwards
Annex 3: Potential groups of staff to provide critical care nursing
In a joint statement in March the Nursing and Midwifery Council and other professional regulators formally acknowledged that during the coronavirus outbreak, healthcare professionals ‘may need to depart from established procedures in order to care for patients and people using health and social care services’.
As the coronavirus pandemic is an unprecedented situation, we recognise that nursing competency work in critical care surge will need to be altered for the duration of the pandemic to preserve life using every available resource.
During peak periods it is envisaged that non-critical care staff will be required to deliver nursing care under the supervision of critical care trained nurses.
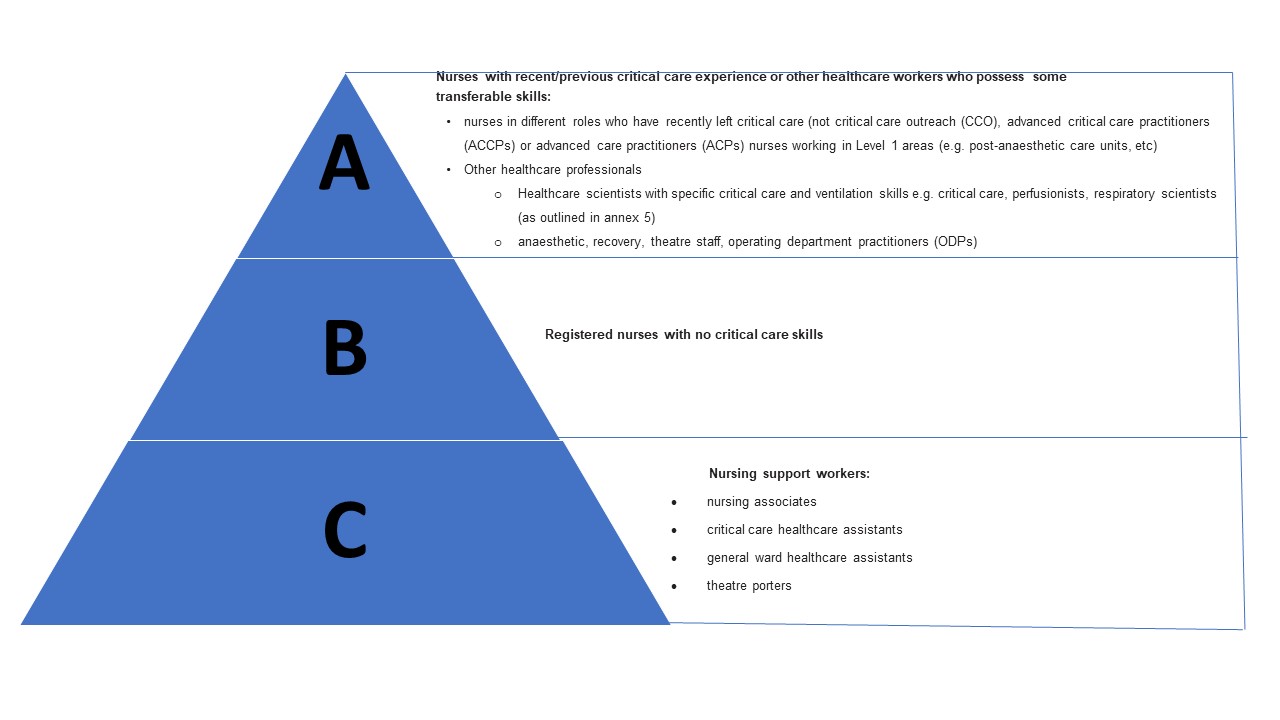
The types of staff available to care for the critically ill may be categorised as follows and identified by organisations:
Nursing staff deployment
A flexible pragmatic and staged approach with an emphasis on team-working rather than a ratio approach should be considered. Healthcare staff deployed to critical care surge areas will be required to work outside their normal practice area and this will cause anxiety for many, including the critical care nurses who will be supervising them. Any changes in working practice will need to be supported to ensure safe practice, safe patient care and staff wellbeing, appropriate supervision and delegation of care. Orientation to and support in the critical care environment are key. Skills will develop with day-to-day supervised practice, using the Step 1 competencies to guide practice and ensure a level of safety.
Training and consistency of the workforce is a key component. Non-critical care nurses ideally should receive condensed critical care training appropriate to their role in preparation for work in the critical care setting. This training should be organised and delivered by critical care nurses/educators and other appropriately qualified healthcare professionals.
Training should ideally be done sequentially so that the critical care nurses can concentrate on upskilling the theatre nurses/ODPs in the first instance.
Independent prescribing: A particular focus on supporting the COVID-19 response should be made to ensure the maximum impact of nurse/midwife independent prescribers.
There are no current plans to support the deployment of students in the next phase of the pandemic. This is designed to structure and support their onward learning. Only in extreme circumstances will this decision be revisited with the Department of Health and Social Care (DHSC), arm’s length bodies, regulators and trade unions. The following questions will need to be addressed when Health Education England considers escalation to the NMC, the Health and Care Professions Council and approved education institutions to consider students supporting the release of other nursing staff to critical care:
- Scale: numbers in year groups and importantly if age/ethnicity demographic data on students is available to assess risk: there are >100,000 medical/dental/nursing/midwifery students. There is also variation in the structure of course programmes regarding timing of clinical placements.
- Phasing of placements: the majority of students undertake clinical practice, many during the first two semesters (ie September-December, January-March), although first year midwifery students typically do not begin clinical practice until January.
- Risks: at university and on placement (ie onward progression, morbidity and mortality ,etc, care homes, social care placements). The majority of clinical placements are in NHS settings, some in social care, some in private providers. Logistics, volume and speed of testing both before ‒ and importantly repeatedly throughout ‒ placements will be challenging, particularly where programmes differ.
- Options: ranging from testing approaches to pausing all placements. COVID cases within university campuses should be broadly manageable, whereas off-campus containment, eg in social care and care settings, will be more challenging. The ‘bubble’ concept in healthcare students is not feasible, as most live and socialise in mixed population settings with non-healthcare peers.
- Scope for alternative experience: for example through simulation in line with the appropriate regulator guidance
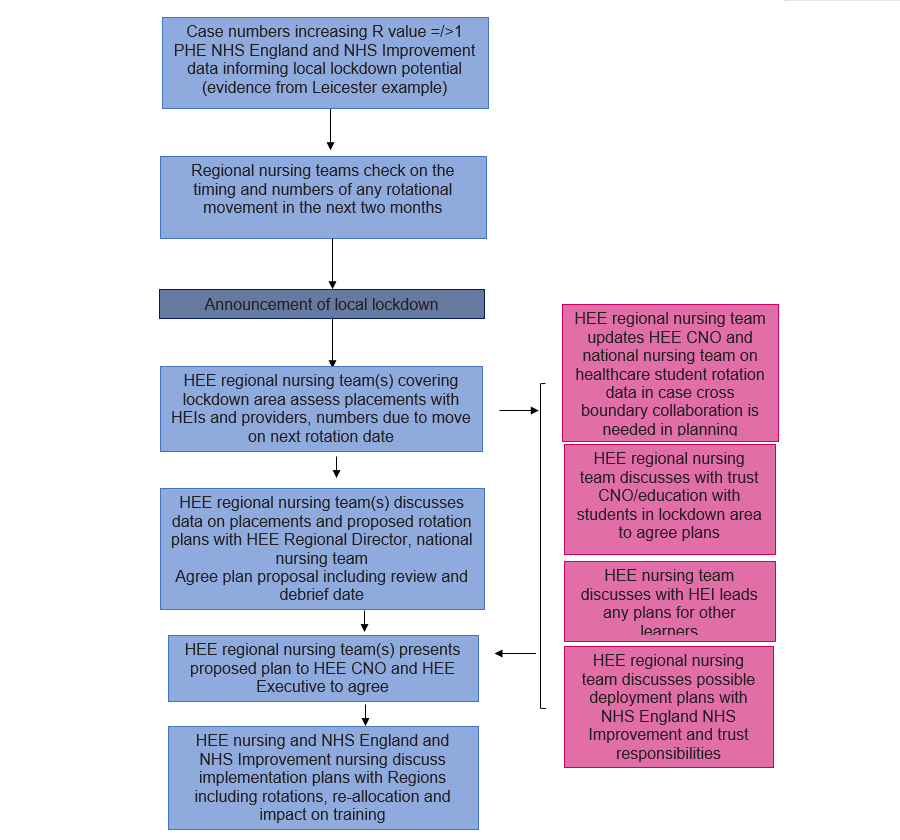
Working in partnership with the NHS England and NHS Improvement lead for infection prevention and control, HEE has identified several key triggers for a discussion in regions about actions to mitigate escalation and the case for any deployment of learners:
- increasing admissions to acute services
- outbreak numbers >50 case per 100K population
- R rate =/>1.0
- workforce sickness and absence increases >3% of staff
- increasing children’s absentee rates (across all education years)
- increasing admission to critical care and ventilated/oxygen supported (V/O) beds.
Escalation flow diagram
Nurses with recent/previous critical care experience of some transferable skills. (Category ‘A’)
Suspension of elective surgery will allow the delivery of training programmes including simulation training, which should be designed using the supernumerary competencies from the Step 1: National Competency Framework for Registered Nurses in Adult Critical Care.
Registered nurses with no critical care skills (Category ‘B’)
Training should be designed for non-critical care staff in critical care using Non–critical care staff in critical care – emergency induction document.
Nursing support workers (Category ‘C’)
Training and simulation to focus on team working for turning/washing/proning.
Additional education resources such as clinical contact details, clinical guidelines and education packages should be easily available and readily accessible across the hospital for nurses and other professionals working in unfamiliar situations.
Annex 4: Redeployment of healthcare science staff to support critical care, high dependency units and those on oxygen therapy
More information can be found in Deploying the healthcare science workforce to support the NHS clinical delivery plan for COVID-19: Version 2, 5 April 2020 – https://www.england.nhs.uk/coronavirus/publication/deploying-the-healthcare-science-workforce-to-support-the-nhs-clinical-delivery-plan-for-COVID-19/
Annex 5: A framework for organising the allied health professions acute sector workforce to meet the Phase 3 COVID-19
Introduction
Allied health professionals (AHPs) are integral to the delivery of multidisciplinary care in the acute sector and often AHPs working in the acute sector also have a role across patient pathways and into community settings. They are vital in the decision-making process, so ensuring they are part of the multidisciplinary team, embedded in the clinical model, is crucial for patients to ensure the provision of holistic and high quality care.
AHPs are involved in many clinical areas of the hospital, building links for the sharing of skills and procedures. This positively impacts on patient flow and reduces the need to move patients through the system, providing continuity of care at all stages and levels. The skills required vary among the range of professions represented within the team but there are some core themes:
- highly developed clinical reasoning
- rapid but effective decision making
- patient focused goal setting.
AHPs produced a collaborative AHP statement in March which identified the need for AHPs to potentially work in unfamiliar circumstances or surroundings, or work in clinical areas outside their usual practice for the benefit of patients, individuals and the population as a whole.
AHPs have a key role in the acute sector, directly influencing the quality of care a patient receives and the decisions made around all aspects of an individual’s admission, treatment, rehabilitation and discharge from an acute sector setting. They have played a vital role in leading and delivering the ‘COVID19 hospital discharge service requirements’ and should continue to do so.
AHPs work across all acute sector pathways of care. They are: art therapists, drama therapists, music therapists, podiatrists, dietitians, occupational therapists, operating department practitioners, orthoptists, osteopaths, prosthetists and orthotists, paramedics, physiotherapists, diagnostic radiographers, therapeutic radiographers, speech and language therapists.
Framework for assessing AHP workforce demand and capacity
Developing workforce safeguards contains recommendations to support provider organisations in making informed, safe, effective, and sustainable workforce decisions, and identifies examples of best practice in the NHS. It was developed with sector leaders and frontline staff and builds on the National Quality Board’s (NQB) guidance.
Trusts are required to comply with the ‘triangulated approach’ to deciding staffing requirements described in NQB’s guidance. This combines evidence-based tools (where they exist), professional judgement and outcomes.
AHPs are usually centrally deployed, working peripatetically, allowing flexibility in care delivery. Patients are referred to AHPs on an individual needs based assessment. This allows for efficient and effective deployment and redeployment of the workforce.
In the absence of nationally published, evidence-based staffing tools, the following simple framework which requires local assessment of patients’ needs, acuity, dependency and risks, and local assessment of staffing establishment (capacity and capability) can help ensure the right staff with the right skills are in the right place at the right time.
Daily monitoring and regular review will be required in a rapidly changing environment.
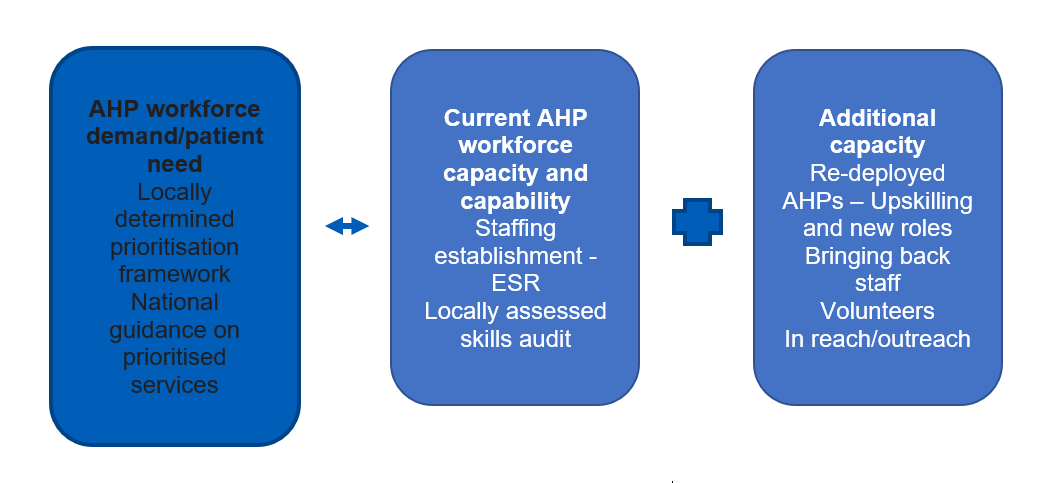
Assessing AHP workforce demand/patient need
The challenge for such a flexible workforce is to ensure that the right staffing resource, capacity and competence is deployed and redeployed to meet the demands required across the system:
- treatment of COVID-19 patients in hospitals and expansion facilities
- maintenance of essential non-COVID-19 prioritised services in the hospitals
- treatment and management of COVID and non-COVID-19 patients in the community.
AHP services and teams will have local prioritisation processes that should be followed. Teams should start their shift by allocating individual roles to ensure key services are covered and sickness is noted.
Understanding the workforce skills required for COVID-19 and non COVID1-9 pathways, coupled with the principles of ratios (where available) in deployment, will provide a practical framework for deployment decisions at local and regional levels.
1. Assessing current AHP workforce capacity and capability for establishment setting
The AHP workforce is diverse. Each profession will have its own skillset, and within each profession, each member of staff will have their own specialism and their own level of expertise. These differentiating criteria are not visible from coding in the electronic staff record (ESR) but are important considerations when organising and deploying the workforce in response to COVID19.
To rapidly gain insight into the AHPs with the most impact on COVID-19 and non COVID patient pathways, it is necessary for the acute sector to categorise staff by (1) area of work and (2) level of skill and experience.
Area of work
Examples of area of work:
- respiratory / critical care
- elderly care / frailty
- neurology / stroke
- paediatrics
- oncology / palliative care
- occupational health
- trauma and orthopaedics
- general medicine
- general surgery
- emergency department / urgent treatment centre / fracture clinic
- musculoskeletal (msk) / pain management / rheumatology
- pelvic, obstetrics and gynaecology (women’s health)
In addition to or instead of area of work capacity could be analysed using a methodology bespoke to the current challenges.
COVID-19 caseload (with sub-categories of area of work).
Trust’s priority/at risk pathways currently being restored (with sub-categories of area of work).
Services with a critical role in improving / protecting acute capacity, eg admissions avoidance and discharge teams etc
Services/professions who could provide a vital support function to others, eg ODPs in
ICU supporting continuous mechanical ventilation, airway management and Emergency care, such as (resuscitation and intubation) along with generic airway management and podiatrists supporting community nursing teams with vascular assessment and wound care preventing hospital admission.
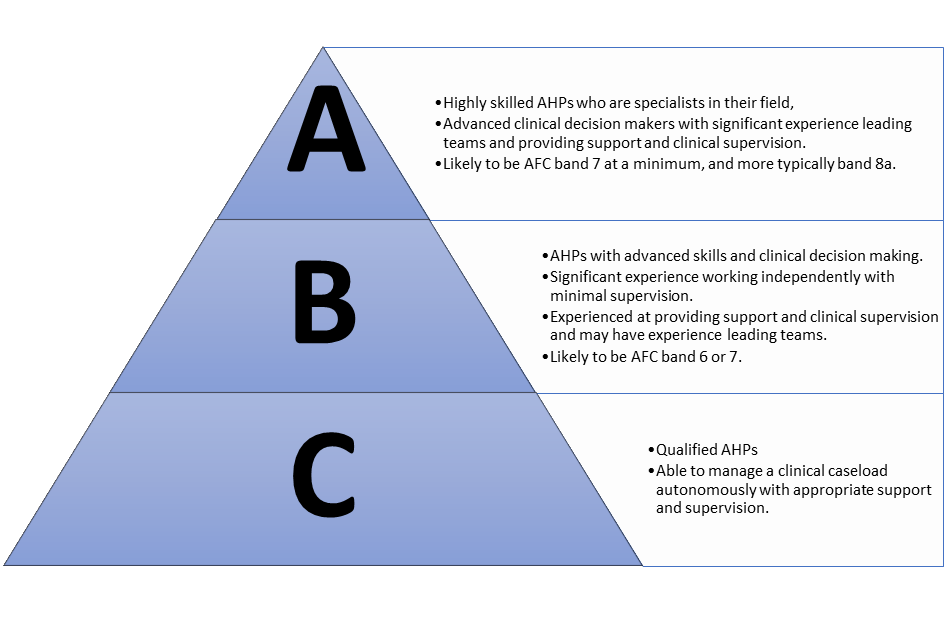
The ABC framework can be used to understand the skill mix in an establishment of staff. It AHP staff according to their skills, competencies and level of experience. Assigning every staff member to a category can help indicate whether there are enough staff with the right skills to meet predicted demand.
It is important that staff are coded accordingly so that rosters can be drawn up that demonstrate an acceptable ratio of category A to category B and category C AHPs. This is particularly important where AHPs may not be working in their usual teams, and where new staff and returners will be included in service delivery.
Using this category method on each roster will enable deployment decisions that balance clinical leadership and supervision across the service.
Other considerations to ensure effective deployment of safe and effective capacity and capability deployment are:
- AHP leadership: All staff must be aware of who is leading, strategically (Chief AHP), professionally, clinically and operationally, the service. Clear governance and accountability help ensure quality and safety of patient care.
- Working patterns/rosters: Working patterns may need to be redesigned for some AHPs delivering services; for example, an increased presence of staff at night and out of hours, and/or consideration of seven-day services.
- Productivity: All teams should also review their clinical processes and ensure they are streamlined to reduce duplication and optimise patient care.
2. Additional capacity
Further redeployment of clinical staff may be needed. The process for this should consider individual staff circumstances, including previous experience and, in some cases, health and current medical history.
3. Principles for staffing deployment and redeployment
A range of existing and returning staff have been and will continue to need to be rapidly deployed into new clinical roles and environments not traditional in their normal scope of practice. In a joint statement the Health and Care Professions Council and the General Osteopathic Council, alongside other professional regulators, have formally acknowledged that during the coronavirus outbreak, healthcare professionals ‘may need to depart from established procedures in order to care for patients and people using health and social care services’.
There are a range of initiatives to support our NHS people and the health and care organisations in which they are working. COVID-19: Deploying our people safely’ summarises the key considerations for the safe redeployment of staff and deployment of those joining the NHS in temporary support of our existing workforce.
Further principles for considerations are:
- Supervision: All AHPs should be appropriately supervised when delivering clinical care. Clinical supervision is a vital part of AHP practice as set out in the HCPC Standards of Proficiency and the Key Characteristics of Effective Supervision.
- Competency: Deploying and redeploying staff may require staff who would not usually work across a certain pathway or in a certain team to require assessment of their competences to ensure that were required they receive the necessary training to enable them to deliver care. They may also not feel confident in this work and will initially need additional support which should be considered in the supervision model. Consideration should also be given to previous experience and site familiarity.
- Training: Health Education England e-Learning for Healthcare (HEE e-LfH) created an e-learning programme in response to the Coronavirus (COVID-19) global pandemic. The programme is freely available and contains, for example but not exhaustive, learning resources AHPs deployed into different clinical specialties and specific training programmes for AHPs working in acute and critical care.
- Induction: All AHPs redeployed to a new clinical area/site should receive an induction. This induction should concentrate on clinical considerations to deliver safe patient care, life support and personal protective equipment (PPE) training. Induction should occur as a priority so that staff are prepared for redeployment.
- Staff health and wellbeing: Local support mechanisms for AHPs should be developed as a priority: https://people.nhs.uk/ provides guides and further information to support this. Employers have a moral and statutory duty of care to protect and preserve their employees’ health and safety. Further guidance can be found here https://www.nhsemployers.org/COVID19/health-safety-and-wellbeing/supporting-staff-health-and-safety
Annex 6: A framework for organising the acute sector pharmacy workforce to meet the Phase 3 COVID-19
This annex aims provides advice and guidance to the secondary care pharmacy workforce to ensure pharmacy services can continue to support patients and contribute to the NHS COVID-19 response, including surge areas and Nightingale hospitals.
1. Safety principles for staff and patients
- The acute hospital chief pharmacist is responsible for safe and effective use of medicines across the trust and for the deployment of pharmacy staff.
- Redeployed pharmacy team members should normally work to the limits of their usual framework of competence and experience but may have to work outside their usual teams, hierarchies and places of work.
- Pharmacy staff undertaking new roles will require support during the surge. Individuals should follow the General Pharmaceutical Council guidance for practice and undertake an assessment with their employer to ensure their competence meets the required role.
- Pharmacy team members should not be removed from roles which would leave core pharmacy services understaffed to the extent they become unsafe for the COVID-19 response.
- Pharmacists who are independent prescribers may need to broaden their scope of practice to support the COVID-19 response. This should be undertaken with sufficient planning, training, supervision and local approval. Those supervising prescribing pharmacists should normally be independent prescriber pharmacists.
- Redeployed pharmacy team members may be at increased personal, physical or mental health risk, because of their lack of experience in their new working environment. Induction and orientation will be key, as well as professional support, supervision and the assignment of a designated contact person.
- Established medicines governance systems should be used throughout, overseen by the chief pharmacist, medical director and the chair of the drugs and therapeutics committee (or equivalent). There will be occasions where these three individuals will need to make decisions rapidly and without the usual full process.
2. Principles for pharmacy staff deployment
Supervision: The chief pharmacist is responsible for ensuring adequate supervision across the pharmacy workforce. All redeployed pharmacists and pharmacy technicians should be appropriately supervised and professionally supported when delivering clinical care and pharmacy services. This supervision should include escalation and referral processes. This should be delivered by a senior pharmacist who routinely works in the service, although it is recognised that through necessity there is likely to be a higher number of those redeployed per supervisor than would be the case under usual circumstances. Unregistered pharmacy support staff who are redeployed should be supported according to the same principles by a senior pharmacy technician.
Professional practice: Pharmacy professionals should continue to practise within their code of ethics and make themselves familiar with the latest guidance from the General Pharmaceutical Council regarding deploying their services during the COVID-19 response Pharmacy team members and employers will be expected to ensure indemnity is in place. The employer will confirm the expected roles and how individual professionals will be deployed.
Competency: It is likely that staff will have variable experience across the key specialties. However, they may not feel confident in this work and will initially need additional support. Consideration should also be given to this experience and site familiarity. While recognising that pharmacists may be asked to work in unfamiliar roles, no pharmacist should be asked to undertake work in which they do not feel competent.
Independent prescribing: A particular focus on supporting the COVID-19 response should be made to ensure the maximum impact of pharmacist independent prescribers – both those registered and prescribing and those who are registered but not routinely prescribing. The latter will need to assure themselves they are sufficiently competent in the area they are asked to use their prescribing skills in.
Medicines preparation and administration: Pharmacy technicians and other appropriate staff who are being deployed to carry out medicines preparation and administration roles must have adequate supervision and training to ensure they are safe and competent to fulfil these roles.
Rosters: Working patterns may need to be redesigned with an increased presence of staff at night and out of hours. All staff may need to contribute to on-site, on-call rotas. The impact this may have on staff morale should be considered and plans to support staff should be prioritised.
Staff wellbeing: Working outside usual systems can be stressful and can impact on wellbeing and staff morale. Local support mechanisms for pharmacy teams should be developed as a priority. Rosters should also be designed with the assumption that a proportion of staff will be unavailable due to sickness. Teams may choose to start their shift by allocating individual roles to ensure key services are covered and sickness is noted. Organisations will have their own local prioritisation processes, which should be followed. Priority roles will depend on the setting and include clinical support to critical care and emergency departments, ensuring safe, timely and resilient supply of medicines from supplier to patients, providing advice to healthcare professional and patients on the use of medicines.
Service leadership: The chief pharmacist must ensure team structure is clear and supports escalation, supervision and productivity. This helps to ensure quality and safety of patient care.
Staff tracking: Organisations need robust measures to ensure all the pharmacy team are identified and contactable, and their attendance/absence is tracked appropriately, including their contributions to on-call rotas.
Further escalation: Further redeployment of clinical staff may be needed, and the process for this should consider individual staff circumstances, including their previous experience and, in some cases, their own health and current medical history. The following suggests initial redeployment steps; however, the scale of the incident may require an expansion of redeployment beyond these.
3. Deploying in specific circumstances
Critical care
Critical care should be a priority for staff deployment. Due to the knowledge and skill set required to provide clinical pharmacy in critical care, consideration will need to be given to significant induction, supervision and support for pharmacists and pharmacy technicians. This applies for both COVID and non-COVID presentations.
Emergency department
Many local organisations have a planned redesign of services in emergency departments, including front-door streaming, rapid assessment and triage and patients being seen directly by specialties without prior ED assessment. Pharmacy services will need to work with clinical colleagues to safely support any changes.
Medicine (respiratory)
It is likely that there will be a large increase in medical admissions as a result of COVID-19. Many of these will require specific respiratory support of varying levels. Pharmacy teams will need to consider how they best support this patient group.
End of life care
There is a need to prepare for a flexible and responsive approach to supporting individuals in a range of settings. It is expected the demand on specialist team skills will exceed usual capacity, and pharmacy teams will need to prepare to support the care of patients at this time, with solutions being determined by local need.
Medicines aseptic preparation and manufacture in NHS hospital pharmacies
The demand for these services will increase significantly and should be protected as best as possible from staff redeployment unless considered essential. Hospital chief pharmacists across a locality should plan for collaboration and efficiency in these services.
4. Nightingale Hospital pharmacy workforce planning
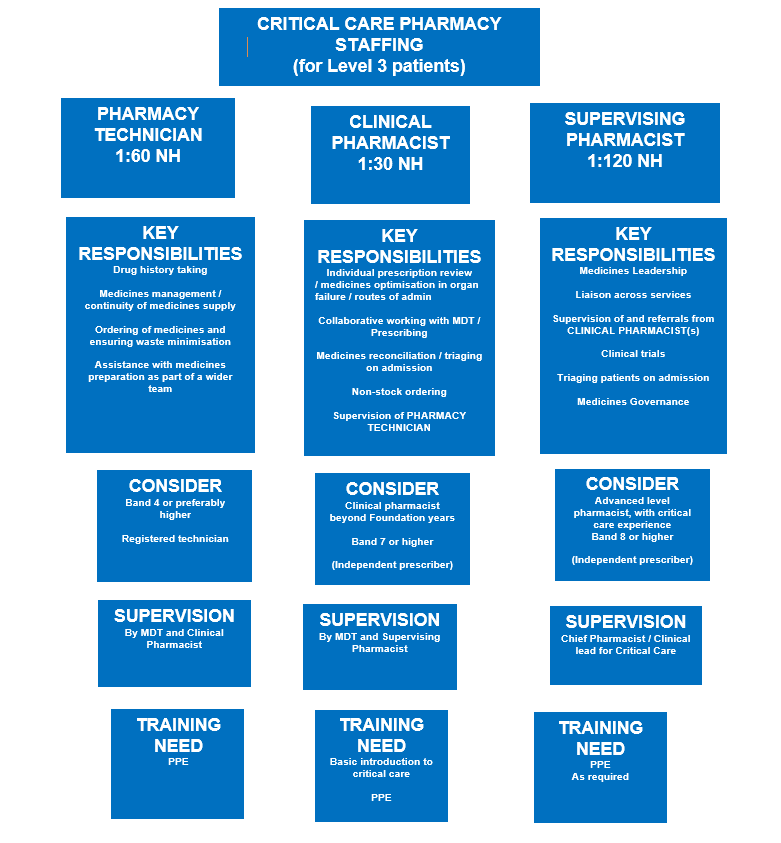
To support safe patient care and local decision making, this guidance outlines the workforce requirements for staffing critical care and general medicine (level 0/1) based on published guidance and the current planning in NHS Nightingale Hospitals. Diagram 1 outlines staffing ratios (NH) for critical care based on professional consensus, expert critical care pharmacy input and initial workforce plans from NHS Nightingale hospitals.
The ratios are the midpoint of the range of staffing ratios and are presented as a single number in line with previously published consensus guidance. The model below is predicated on a senior pharmacy leadership having been established and providing overarching leadership and accountability for the pharmacy services across the Nightingale hospital. Clear governance between an NHS Nightingale Hospital site and an established trust is required for all clinical models.
Diagram 1: Critical care pharmacy model
4.1 Principles for determining workforce requirements
The principles set out below support decision making in modelling and delivering pharmacy services in NHS Nightingale Hospitals and surge critical care capacity.
The focus of the pharmacy service in NHS Nightingale Hospitals should be medicines continuity and patient safety, rather than medicines optimisation. Key aims of the pharmacy workforce:
- To provide safe and effective patient care by providing timely clinical pharmacy input into individual decisions relating to the use of medicines
- To manage medicines supply, reduce waste and ensure shortages are managed safely
- To ensure the safe and timely supply of the right medicine to the right patient.
The pharmacy workforce will deliver this service through:
- connection with the wider MDT in each NHS Nightingale Hospital to understand the changing patient mix and staffing availability
- ensuring continuous learning
- a developing operational plan that informs daily decision making on priority services, distribution of staff and tasks
- ensuring supervision, induction, indemnity and staff well-being are identified, agreed and implemented.
4.2 Principles of critical care pharmacy service provision
Level 3 critical care patients require clinical support from a wide range of professionals, including highly trained clinical pharmacists. To ensure that patients in this category receive the right care, critical care pharmacists will have to support non-specialist clinical pharmacists in a supervisory capacity as they work to care for these patients. The pharmacy staffing skill mix can be further supported by the inclusion of appropriately trained pharmacy technicians in an MDT. Staffing requirements for L0-L2 critical care patients will by its nature be different to this skill mix.
Close working between clinical pharmacy and operational pharmacy teams is particularly important to maximise the provision of injectable medicines in ready to administer or ready to use format, and ensuring waste is minimised.
Table 1 compares the workforce models for Level 3 critical care from consensus guidance to the initial models from the NHS Nightingale hospitals. These models may also provide senior pharmacy leaders in local pharmacy services with guidance on how a service might be redesigned to support both NHS Nightingale hospital and local critical care surge capacity.
Table 1: Critical care Workforce: consensus guidance and Nightingale hospital models
| Workforce requirement | Consensus guidance | Nightingale Hospital |
|---|---|---|
| Critical Care Level 3
(ventilation or 2 or more organ failure) |
Range of 4.2-6 pharmacists per 60 level 3 beds for 5 days per week. The consensus of critical care pharmacists, the United Kingdom Clinical Pharmacy Association and the Royal Pharmaceutical Society is that there should be at least 0.1 WTE 8a specialist clinical pharmacist for each single Level 3 bedFor the larger hospital with more than one ICU, the critical care pharmacy service is best delivered in a team approach. An example of the team used for a hospital with 100 critical care beds would be band 8 specialist critical care pharmacists, comprising: a band 8C consultant pharmacist, a band 8b (as deputy), 2 to 3 at band 8a and 3 to 4 at band 7(Source: FCIM) |
Range of 1.9 – 3 pharmacists per 60 level 3 beds**
Including Experience Critical Care Pharmacist 0.5 – 0.6 Supporting Clinical Pharmacist 1.4 – 2.4 Pharmacy Technician 0.5 – 1.2 **In the development of the workforce plan for field hospitals the following have been key considerations
|
Table 2 describes the workforce model that have been developed for operational pharmacy services – including medicines preparation, logistics, leadership and medicines supply.
Table 2: Operational pharmacy workforce model
| Site based workforce requirement for 60 beds ** | Headcount per shift for 60 beds ** | |
|---|---|---|
| Aseptic medicines preparation | Pharmacists Pharmacy Technicians Pharmacy Support Workers |
0.24 – 1 0.24 – 1 0 – 3.6 |
| Logistics and procurement |
Pharmacy Technicians (inc roles in CDs, logistics) |
0.12 – 1.42 0.84 – 2 Highly variable |
| Leadership and governance | Chief Pharm 1 Logistics lead 1 Logistics leads Governance lead E&T lead |
1 1 1 0 – 1 |
** These are indicative. The variation in workforce model is significant and related to the clinical model of the Nightingale Hospital, the services provided by the host trust pharmacy team and the contribution made by non-pharmacy staff in the Nightingale hospital itself
4.3 Supply of pharmacy workforce
The availability of staff will be a major constraint on the operating model of pharmacy. To ensure services can be delivered safely it is vital to secure staff from a range of sources. A key approach is collaborative working within each NHS region, with support from Regional Chief Pharmacists and the HEE regional pharmacy Dean, working closely with the NHS Nightingale hospital workforce cell. The process of securing workforce from local NHS trusts will be aided by escalation via the NHS Nightingale Hospital operational leadership and Regional Chief Pharmacist. A balance will need to be made between the workforce requirement for the individual trust including its surge capacity and the contribution to the Nightingale Hospital. All potential routes to secure workforce should be considered, including temporarily registered returners, etc, and the HEE pharmacy dean will be well placed to support the process of identifying sufficient workforce.
The workforce contribution to the Nightingale Hospital from a local NHS trust pharmacy service will require an assessment of the workforce available at the host trust to support local patient care, and any surplus in staffing may be used to support extra capacity or Nightingale hospital demands. Depending on the need to support the Nightingale hospital workforce, this assessment should be based on the minimum staffing required to maintain medicines continuity and patient safety. In this assessment of workforce, the local trust should consider the impact of the clinical model operating on the NHS Nightingale hospital.
Consideration should be given to developing the Nightingale hospital model to the time pharmacy staff will need to support other healthcare professions in the use of medicines, eg varied clinical expertise forming the wider critical care team, or new treatment protocols and administration routes.
