Clinical validation of surgical waiting lists: framework and support tools
Contents
- Clinical validation of surgical waiting lists
- Section 1: Framework
- Section 2: Operational guidance
- Appendices
- Appendix A: Shared decision-making (SDM) tool
- Appendix B: Frequency asked questions
- Appendix C: Supporting distressed patients
- Appendix D: Waiting list prioritisation
- Appendix E: Resources for trusts and patients
- Appendix F: Potential impact of each stage of clinical prioritisation
- Appendix G: Admitted waiting list review process flow
Classification: Official
Publications approval reference: C0760
Clinical validation of surgical waiting lists
Framework and operational guidance
Version 2, December 2021 [Changes from previous version have been highlighted in yellow. This includes the addition of the operational guidance which can be found from page 7-12]
Section 1: Framework
Most long-waiting patients on the surgical waiting list will have agreed to undergo operative treatment before the coronavirus pandemic started. Many people’s circumstances may have changed as a result of the pandemic or other factors since then, and some patients may now have changed their minds about having surgery or wish to defer this until the pandemic is over. Similarly, some people’s condition may have changed, which they may not have wanted to inform their GP or specialist about.
The clinical validation of surgical waiting lists project will produce a clinically validated waiting list that allows operating lists to run effectively by:
- Checking on a patient’s condition and establishing any additional risk factors
- Establishing the patient’s wishes regarding treatment
- Providing good communication with patient and carer and GP
- Introducing the P6 categories that allows patients to postpone surgery but remain on the waiting lists
This project is supported by the Academy of Medical Royal Colleges (AoMRC) as well as relevant medical royal colleges and specialist societies. It has been reviewed by the NHS England and NHS Improvement legal cell.
1.1 Principles
The principles are:
- Times have changed: patients now face different risks and their social and economic circumstances may have changed.
- Local design and delivery of the validation process: core standards but locally interpreted. No patient’s care should be delayed by the validation process: those trusts that have started to clinically validate their surgical waiting lists should continue.
- Arrangements to support patients who change their mind about surgery after the initial conversation must be inplace.
- Appropriate consultation to meet a patient’s needs: remote or face to face.
- Narrowing of health inequalities: e.g. support for people with communication difficulties,11 including those whose first language is not English; appropriate
arrangements for those with a learning or behavioural difficulty or a mental health problem that may impact on their capacity to make an informed decision.
The project is about making the best mutually agreed decisions with patients and is not an exercise to reduce numbers on waiting lists.
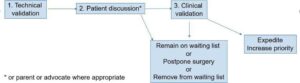
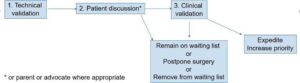
Waiting lists should be validated in two or three stages:
- Technical validation: ensure the waiting list is accurate and up to date
- Patient discussion: patients are contacted by a locally determined competent team to establish their wishes
- Remote clinical consultation: for patients who wish to discuss their situation in more detail using shared decision making (SDM)
1.2 Use of the P5 category
Since 2015, patients have been able to remain on the waiting list for treatment, even if this extends their RTT pathway beyond 52 weeks. The P5 category was created to allow patients to defer treatment/investigation due to concerns over COVID-19. Both the P5 and P6 codes ensure patients remained on active, visible waiting lists.
According to previous operational guidance, P5 pathways were to be re-reviewed within six months of their original review, and this process could continue indefinitely. However, with the immediate risks of the COVID-19 pandemic diminishing, it has now been decided that the P5 category will be removed from 4th January 2022. All P5 patients should be re- reviewed and allocated to one of the remaining P codes. Next steps for the patient will be determined by existing Referral to Treatment (RTT) rules (where appropriate) in line with local access policies, and patient discussion.
1.3 Use of the P6 category
Patients who have been offered two dates for treatment and have declined to accept but still wish to remain on the waiting list will be coded as P6. This is in line with current patient choice guidance but enables us to quantify the number of patients who fall into this category.
Pathways recorded in the P6 category should continue to be managed in line with current waiting list rules and local access policies, allowing for patient choice delays where clinically appropriate. Patients will continue on active RTT pathways (where relevant) and remain on active waiting lists. There will still be a requirement for these pathways to be reported via the waiting list minimum data set (WLMDS) to enable us to quantify the number of patients choosing to delay treatment for social reasons.
To note:
- The clinician and provider retain responsibility for any changes to the patient’s pathway.
- The patient’s GP must be notified of the outcome of the discussion. Patient initiated follow-up should be considered where appropriate
- Patients are free to change their minds. Trusts must provide a contact telephone number and/or email for patients to contact should they change their mind within 28 days.. Beyond that date, the patient will need to be re-referred by their GP.
- The local patient advice and liaison service (PALS) should be made aware of the project
- Local teams should design their own system for waiting list validation.
- Implementation: the Elective Care Recovery and Transformation team will support implementation, initially with a soft launch at pilot sites in the North West to identify any specific training issues.
- This framework includes tools and other resources that local teams might consider adapting for local use:
- A shared decision-making tool for use when a patient requests a clinical review (Appendix A)
- Frequently asked questions, both for trusts and patients (Appendix B)
- Supporting distressed patients (Appendix C)
- Clinical prioritisation (Appendix D)
- Pre-habilitation options (weight loss, activity, mental health, diabetes, smoking). These provide generic national resources but local options should be substituted when available
- Template pre-habilitation advice sheet and list of national resources
- Template letters to patients published in word to allow easy local adaptation (published separately)
Section 2: Operational guidance
The information in this section has been compiled to support the national framework for consistency across systems and providers.
The clinical prioritisation programme is part of the third phase of the NHS response to COVID-19 and is designed to support the prioritisation of waiting lists as part of the recovery of elective activity. The priority is to ensure that all patients on an admitted patient care pathway have been reviewed and clinically prioritised to support discussions with patients about their planned care, to give greater clarity of the number of patients awaiting procedures at each priority level, to inform service capacity planning, and support the booking of patients.
2.1 Data quality validation
Data Quality issues and potential errors should be reviewed and corrected as far as possible prior to clinical validation in order to provide as accurate and up-to-date list as possible for clinical review. Data quality issues may be identified through the national validation programme feedback reports and data, or through local data quality reports.
Issues likely to affect the management of the patient’s pathway should be prioritised. For admitted pathways potential issues are likely to include:
-
- Past TCI dates
- Potential duplicates
- Missing waiting list or pathway information (eg due date, intended procedure)
- Decision to admit but no waiting list entry
- Patients on an admitted waiting list without an active RTT clock
The data quality of pathways with a decision to admit is usually better than for other pathway stages due to regular validation processes. Data quality validation should not delay the clinical prioritisation process, but checks should be completed to an adequate level to support the generation of a list of patients awaiting admission for treatment to be contacted by the trust.
2.2 Administrative validation
Patients (or for paediatric patients a parent or appropriate guardian) should be contacted by letter, telephone, or email to confirm their current circumstances, needs and preferences relating to their planned treatment, so that up-to-date information is available to support the clinical prioritisation process.
The trust should consider appropriate patients to contact and the appropriate means, taking into account those patients who may have TCI dates already booked in the near future, when the patient was added to the admitted waiting list, and when the patient was last contacted. The means of contact is likely to depend on the volume of patients, urgency of booking, patient demographics, and staff availability.
- Patients should be asked to indicate whether they still require treatment or whether they have been treated elsewhere or their condition has otherwise resolved.
- Patients should be asked to provide details of any periods of unavailability, and the general reason for this, patients reluctant to come in due to hospital due to Covid – 19 would fall into this category. The patient will remain on the waiting list in line with national RTT rules, and this information will be used to support planning and booking their treatment. These patients will be categorised P6.
Clear information should be provided to the patient about next steps. Some patients will proceed to a shared decision-making discussion with a clinician, and information should be provided about this to enable patients to participate fully in that discussion with an appropriate clinician. This will include where further information is needed to enable the clinical team to assign or update a prioritisation category, where patients are undecided about whether to proceed with treatment, or wish to discuss their condition and their treatment options, or where a patient has been listed for a procedure included in national guidance on evidence- based interventions.
If contacting by letter or e-mail patients should be given adequate time to respond (at least two weeks from receipt of letter) and clear information about the need to respond and next steps if they do not. Further attempts must be made to contact any patients who do not respond to the letter, or who cannot be contacted by telephone. Some of these attempts should be made outside of normal working hours, as well as contacting the patient’s GP or referrer.
Information provided by patients should be recorded on the trust PAS on the patient pathway information, to provide information to support clinical prioritisation and booking instructions.
Patients should not be removed from the waiting list without a clinical decision and communication and agreement with the patient.
Administrative validation should be completed to an adequate level to enable identification of those patients on the admitted waiting list with a clear decision to proceed with their planned treatment, and those patients where further information, or a shared decision- making discussion is required. A list of those patients requiring further review should be generated to support the clinical validation process.
2.3 Clinical validation
Information provided by the patient on their current condition, fitness and availability to proceed should be collated to enable a specialty level review of the admitted waiting list.
Where a patient has indicated that they wish to proceed with surgery for a routine procedure, and there are otherwise no indications requiring a shared decision making discussion between the patient and an appropriate clinician, a clinical priority category may be assigned and recorded based on the locally agreed process appropriate for the patient’s condition/procedure. A separate clinical discussion with the patient will not usually be required.
The specialty team may also be able to identify those patients potentially suitable for treatment in the Independent Sector based on this information.
For patients where a shared decision-making discussion is appropriate (either required by the clinician or requested by the patient), a clinical review should be undertaken by an appropriate clinician in accordance with the national guidance on clinical validation of surgical waiting lists.
The list of patients to be reviewed should be ordered to enable patients with the most urgent conditions to be reviewed first based on the information available (such as urgency indicated at referral or decision to admit, procedure type, specialty, and length of time that the patient has been waiting for treatment).
Appropriate information should be available to support the process, including information provided by the patient during the administrative validation process on their current condition, fitness and availability to proceed.
The discussion with the patient should include the following elements:
- The clinician’s assessment of the patient’s priority level
- The patient’s current condition and symptoms, and any other clinical conditions or factors that may affect their treatment
- The patient’s understanding and agreement to the planned treatment or procedure, or whether there are more suitable alternative options
- For patients listed for a procedure included in national guidance on evidence-based interventions, or in local policy on procedures of low clinical value or limited clinical effectiveness, options for alternative treatment or condition management should be discussed, and next steps agreed with the patient
- The patient’s fitness to proceed to treatment– if the patient is not currently fit to proceed, the reasons for this should be established, whether this is likely to be a short- term or long-term reason, and if any treatment or other steps required to optimise the patient for surgery. The patient’s pathway should be managed in accordance with RTT rules, so that patients are not removed from the waiting list due to a short-term condition
- Whether the patient is potentially suitable to be treated in the Independent Sector or a hub waiting list (where this is the case, we recommend that this information is captured on the local IT system to allow easy identification of these patients)
- The patient’s availability. Where a patient is unavailable, timescales about their period of unavailability should be noted and an appropriate timescale for further contact and re-review should be agreed.
Updated note on the use of P5 and P6
The P5 category was created to allow patients to defer treatment/investigation due to concerns over Covid-19. Both the P5 and P6 codes ensured patients remained on active, visible waiting lists, whether this is due to COVID-related issues or non-COVID- related issues. COVID-related issues may include clinical risk factors, anxiety about COVID-19, or that the patient is currently self-isolating. Where a patient is unavailable, timescales about their period of unavailability should be noted and an appropriate timescale for further contact and re-review should be agreed. This is to be recorded as P6 from 4th January 2022.
According to previous operational guidance, P5 pathways were to be re-reviewed within six months of their original review, and this process could continue indefinitely. However, with the immediate risks of the COVID-19 pandemic diminishing, it has now been decided that the P5 category will be removed from 4th January 2022 onwards. All P5 patients should be re-reviewed on one further occasion and allocated to one of the remaining P codes. Next steps for the patient will be determined by existing Referral To Treatment (RTT) rules (where appropriate) in line with local access policies, and patient discussion.
Patients who have been offered two dates for treatment and have declined to accept for non- Covid reasons, but still wish to remain on the waiting list will be coded as P6. This is in line with current patient choice guidance but enables us to quantify the number of patients who fall into this category.
Pathways recorded in the P6 category should continue to be managed in line with current waiting list rules and local access policies, allowing for patient choice delays where clinically appropriate. Patients will continue on active RTT pathways (where relevant) and remain on active waiting lists. There will still be a requirement for these pathways to be reported via the waiting list minimum data set (WLMDS) to enable us to quantify the number of patients choosing to delay treatment for social reasons.
The outcome of the discussion should be recorded on the trust PAS as part of the patient pathway information, including the priority category and date that the review was undertaken. The outcome should also be confirmed in writing to the patient and their GP or referrer.
The completion of clinical validation should support a trust waiting list view of patients to be booked by clinical priority and wait time, with appropriate supporting information to enable their treatment to be planned, including information about the patient’s fitness to proceed and availability. This list should support capacity planning including the identification of patients clinically suitable for treatment in the Independent Sector.
Maintaining a clinically stratified waiting list
The review information, including the priority category and the clinical review date (ie the date that the priority level is assigned) should enable the trust to identify any patients requiring re- review if they are not treated within the indicated timescale, or for re-contact at an appropriate time for those patients in the P6 category. Patients remaining on the waiting list should be re- reviewed no later than 6 months after their previous review.
To support ongoing maintenance of the waiting list, and reduce the need for re-review, the above points to be discussed with the patient should be included when a new decision to admit is made, so that the prioritisation category and supporting information can be recorded as part of the patient’s waiting list entry.
2.4 Links for further information
- RTT rules are unchanged and should be followed. RTT guidance, and the latest Q&As relating to RTT measurement and COVID-19
- National guidance on clinical prioritisation of surgical waiting lists
- The Elective Care IST Waiting List Review guide provides general advice on waiting list validation.
- Evidence-based interventions programme
Appendices
Appendix A: Shared decision-making (SDM) tool
- Within the context of waiting list support for patients, the SDM tool may be used by clinicians for planning for patient care and delivery
- SDM is the process whereby patients and clinicians work together to make evidence- based decisions centred on patient values and preferences – The example provided has been adapted for the clinical validation of waiting lists
- Senior clinicians should have increased ownership of waiting list management, particularly for patients with the highest clinical need or length of wait. This is in line with surgical and medical prioritisation guidelines
Classification: Official
Overview (for patients on surgical waiting lists)

Appendix B: Frequency asked questions
Patient questions
1. How long will I have to wait for my operation?
Unfortunately, at the moment we can’t be certain. The pandemic has had a big impact on the NHS and we are trying to resume services and keep patients safe at the same time as we continue to treat COVID-19 cases. We are reviewing all patients to see what they want and prioritise those in most urgent need. We are doing our utmost to ensure you get the treatment you require as soon as possible.
2. I have breached the 18 week wait. What are my options?
As per the NHS constitution, you have the right to access certain NHS services within maximum waiting times or, if this is not possible, for the NHS to take all reasonable steps to offer you a range of suitable alternative providers. However, the pandemic may be limiting these alternative services.
However, it should be noted that although the challenges of the COVID-19 pandemic are now diminishing, some services may still be affected meaning that access to alternative services could be limited.
3. What if I get worse?
If your symptoms get worse, please contact us on [insert contact number]. Alternatively, you can contact your GP or call NHS 111 for advice.
4. What if I change my mind?
You are always free to change your mind. If we agreed that you would come in for surgery/treatment and you decide you no longer wish to have this, or you now decide you would like it when previously you chose not to, please contact us on [insert contact number] or email us on [insert email] and we can discuss your options with you.
5. What about my right to choose?
We are contacting all patients on our surgical waiting list to find out what their symptoms and needs are now, rather than at the time their surgery was booked. This will allow you and your clinician together to agree what is best for you now. If you still require surgery, you can choose between going ahead or postponing it. You may be offered treatments other than surgery, where these are appropriate for you. You don’t need to decide what you want to do when speaking to your clinician on the telephone; you can let us know within [x] weeks following your consultation by contacting us on [insert contact number].
6. Do I need to have a laptop or smart device to have a consultation?
We’re most likely to ring you. Where we can run video consultations, we can use this if you have the right electronic equipment [adapt as locally appropriate].
7. Is it safe to go ahead with my surgery? Will I catch COVID-19 in hospital?
Our hospital follows very strict rules for preventing all types of infection, including COVID-19. You will be cared for in a low risk area and all patients who are admitted to this area will have had a negative swab test, like you. No staff who have COVID-19 symptoms or come into contact with someone with symptoms are allowed to work in the hospital.
8. Can I have a cancellation slot?
It’s impossible to give one answer to this question as it will depend on how our local services are organised and whether this is appropriate for you. However, cancellations do occur and we may consider introducing a system to allow patients to be called in at a late stage (allowing for pre-operative screening and testing) [adapt as locally appropriate].
Trust questions
1. What about the patient’s right to choose?
Clinical validation enables clinicians to gain up to date understanding of a patient’s conditions and by talking to their patients, joint decision-making between clinician and patient. Patients will be given the choice between having surgery/treatment (where required) and postponing this, if they prefer to wait. Patients will also be offered the option of alternative treatments where appropriate.
2. How will clinical validation be applied?
Validation will be undertaken by the clinician responsible for the patient’s care. Patients can then be prioritised for treatment, in line with the FSSA guide
3. We have previously done clinical validation. What will be different this time?
If you have already completed or have commenced clinical validation, including direct contact with patients, since the pandemic commenced, there is no need to repeat if you are confident that the current waiting list is an accurate reflection of the patient’s wishes.
For those that have not started this process, the current status of patients needs to be validated. This clinical validation is based on joint decision-making and also allows patients to be prioritised using the FSSA prioritisation system. Patients should be contacted to explain that they will have a remote appointment to discuss their current symptoms and situation. At a review held with the patient either online or using the telephone, a joint decision should be made and confirmed in writing to the patient, with a copy sent to their GP. The patient will then be prioritised based on this review.
4. Is additional funding available for clinical review?
You will need to discuss this with your local line manager. Remote consultations are most efficient if they are organised like a clinic and performed in a session. ‘Cold calling’ patients does not work. These remote clinics are part of direct clinical care.
5. Does the consultation have to be done face-to-face, by video or by telephone?
Face-to-face consultations should be avoided if possible but for some groups of patients, this will be the only way to ensure good communication and to prevent them from being disadvantaged.. We anticipate that most consultations will be by telephone, but video consultation can be used where both the trust and the patient have this facility.
6. What if the patient does not want treatment?
Patients can choose to delay or decline treatment. We advise that the patient is informed of any alternatives to surgery (if available) and any risks associated with delays in treatment. A clinical decision should be made on whether the patient should be discharged back to primary care or remain under review. Patient initiated follow up may be a good option for some.
7. What happens to the PTL position on the waiting list?
The patient continues to wait for treatment and is therefore visible and reported as part of national weekly and monthly returns. This does not alter current reporting for patients who have chosen to defer treatment.
Appendix C: Supporting distressed patients
Understandably some patients may become distressed or angry when contacted about their surgery.
Trusts can give their patients support via PALS and should ensure this team understands the validation process.
Ensure you have information leaflets outlining the co r angry when contacted about their surgery.
Trusts can give their patients support via PALS and should ensure this team understands the validation process.
Ensure you have information leaflets outlining the complaints process, and can post these to patients if required.
Make sure that junior staff have someone to escalate any concerns to. These are useful resources:
Appendix D: Waiting list prioritisation*
| <1 month | P2 |
| <3 months | P3 |
| >3 months | P4 |
| Patience wishes to postpone surgery due to non-COVID-19 concerns | P6 |
* Based on the prioritisation tool produced by the Federation of Surgical Specialty Associations and endorsed by all surgical colleges.
** This decision needs to be discussed with the patient within six months.
Appendix E: Resources for trusts and patients
| For providers |
| For patients |
Classification: Official sensitive
Appendix F: Potential impact of each stage of clinical prioritisation
Appendix G: Admitted waiting list review process flow
Classification: Official Sensitive
NHS England and NHS Improvement
Skipton House
80 London Road London
SE1 6LH
This publication can be made available in a number of other formats on request.
© NHS England and NHS Improvement Publication approval reference: C0760
25 | Clinical validation of surgical waiting lists: framework and tools