Deploying the clinical and non-clinical optical workforce to support the NHS clinical delivery plan for COVID-19
Contents
- 1. Background and definitions
- 2. Aim
- 3. Objectives
- 4. Principles
- 5. Key considerations
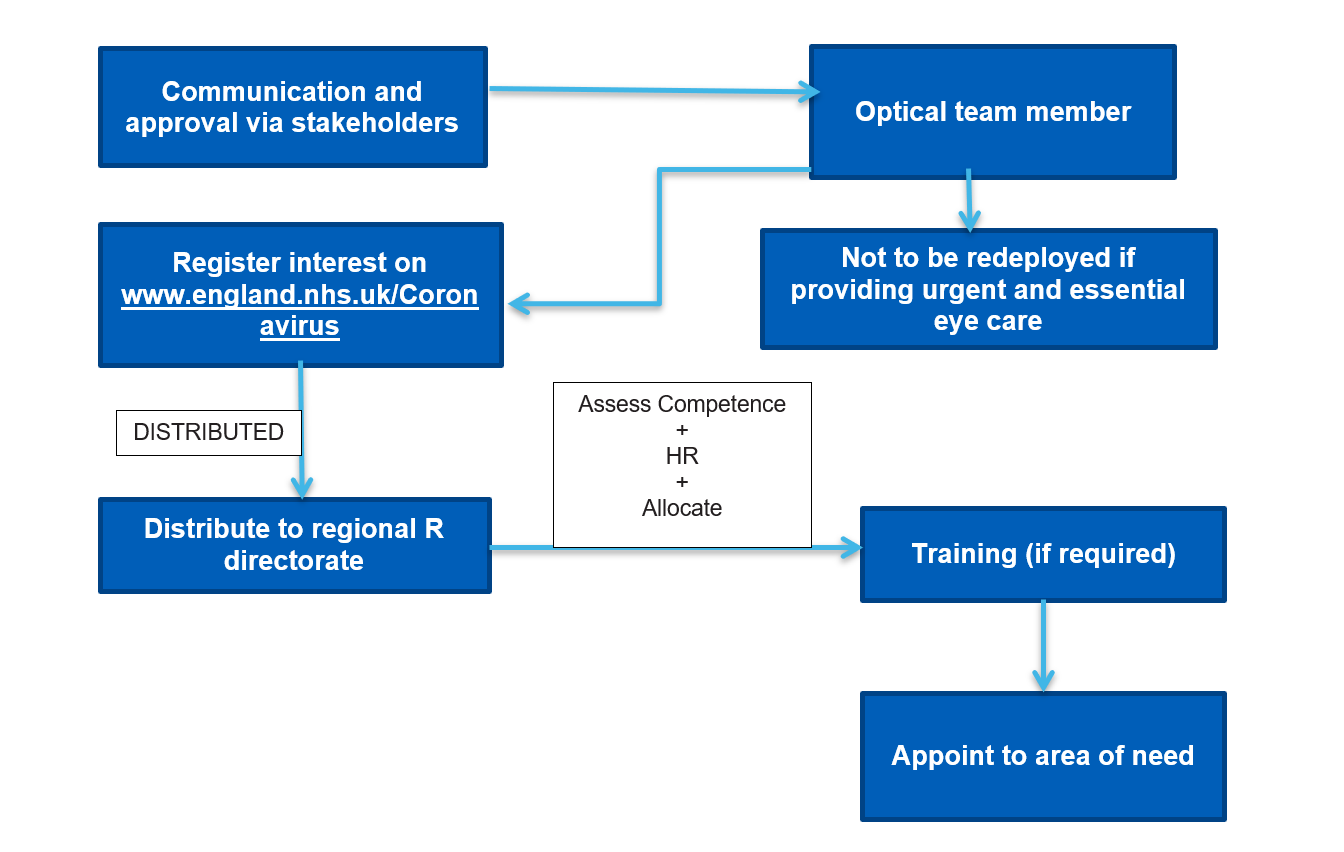
- 6. Redeployment pathway
- 7. Workforce landscape
- 8. Key stakeholders
- 9. Competencies and mapping of potential roles
- 10. Indemnity arrangements – England
- 11. Remuneration considerations
- 12. Induction
- Appendix 1: Transferable competencies
- Appendix 2: Questions and answers for volunteers
- Appendix 3: Self-assessment competency reporting framework
Publications approval reference: 001559 / C0207
12 April 2020, Version 1
1. Background and definitions
The optical workforce in England constitutes around 27,000 optometrists, dispensing opticians, students and businesses that are current registered with the General Optical Council (GOC). With the coronavirus (COVID-19) pandemic and the suspension of routine eye care, this multi-skilled workforce could be called upon for increasing surge capacity. The optical workforce has a wide range of skills and experience that can be utilised to undertake activities that will help clinical colleagues and the wider workforce during COVID-19. This document sets out the principles of safe redeployment and healthcare delivery as critical care units prepare and deliver increased activity during surge and super-surge in the coronavirus pandemic.
It is expected that the clinical optical workforce can be used to free up other roles within the health and social care system and help maintain the delivery of other non-coronavirus related essential services. However, contribution in these other roles would have to be done on a voluntary basis and would be outside of the workforce individual’s scope as an optometrist or dispensing opticians, unless it is in the provision of eye care. By calling on the optical workforce, this will enable the existing healthcare workforce to have the time to focus on tasks at the top end of their competencies.
Some of the optical workforce will still be required to maintain urgent and essential eye care access the system. It is crucial that this is maintained to reduce pressures on GPs and emergency hospital departments.
Other self-employed clinical staff may be available for immediate recruitment.
For non-clinical members of the optical team, there are numerous, valuable local community volunteering efforts which will help vulnerable members of society and which can be offered without undermining furlough arrangements. These optical team members have a wide range of skills that can be utilised during this time of crisis to support the wider workforce. Further information is available here.
While the list in this document is not exhaustive, it provides potential job roles where the clinical optical team may be able to redeploy their skills within their competencies in accordance with GOC standards. Redeployment opportunities will be locally determined. Individual trusts will have their own induction and job specifications and the demand for certain roles will vary depending on locality.
2. Aim
Increase the health and social care workforce by tactically redeploying the clinical optical team, based on meeting locally identified needs.
3. Objectives
- Maximise output from existing workforce.
- Increase capacity where it is needed for response to COVID-19 surge.
- Support medical clinical staff and other health care professionals.
- Ensure effective resilience across the health and social care system.
4. Principles
- Safe for staff and patients.
- Redeployed optical team members should work to the limits of their usual framework of competence and experience even though operating outside their usual teams and hierarchies.
- Competencies have been mapped to specific roles, requiring support during surge. Individuals should undertake a self-assessment to ensure their competence meets the required role. Please see Appendix 3.
- Optical team members should not be removed from roles which would leave urgent and essential optical services understaffed.
- Redeployed optical team members may be at increased personal, physical or mental health risk, because of their lack of experience in their new working environment. Induction and orientation (including in appropriate personal protective equipment (PPE) will be key, as well as the assignment of a designated contact person.
5. Key considerations
- Stakeholders will need to be on board with the deployment process as the profession is likely to engage only if approval by stakeholders is given. Communication and collaboration with stakeholders is key.
- Optical professionals will register their note of interest via the online questionnaire at www.england.nhs.uk/coronavirus
- There will be no obligation for any member of the optical workforce to provide services. This will be on a voluntary basis.
- Expressions of interest will be triaged based on multiple factors including recognised competencies, level of experience and geographical location.
- Consideration to competence and supervision will feature as part of any assessment of mapping across potential roles.
- Once triaged appropriately, the information will be shared with relevant regional teams.
- Regional teams will recruit staff according to demand/operational needs.
- Regional teams will provide necessary and identified training needs, based on local requirements.
- Optical team members will be utilised to meet surge demand, within their scope of practice.
- Optical team members will be expected ensure they have appropriate clinical negligence cover in place – it is important GOC registrants check with their indemnity provider (also see FAQs below). It is anticipated that most redeployment roles for the optical workforce would be on a voluntary basis and outside their normal course of practice. As such, their own indemnity insurance would not cover such activities and they would have to rely upon any cover provided by the Clinical Negligence Scheme for Trusts (CNST).
- Death in Service cover would need to be provided to volunteers from the optical workforce.
- Individuals will need to know what roles they will be expected to do and how they will be deployed. In cases where they are employed, volunteers will need to know how to notify their employer and be made aware of the employment protections they will receive in respect of the leave.
- Finances – compensating individuals for some loss of income and expenses is an important factor in ensuring that enough volunteers come forward. Maximising success will be aided by identifying and agreeing an appropriate rate of compensation and a simple means for individuals to claim.
6. Redeployment pathway
7. Workforce landscape
The optical workforce comprises mainly independent providers and professionals (on the same basis as GPs, community pharmacists and general dentists) and small number within NHS hospitals, universities and research institutions.
The majority of the optical clinical workforce operate under the General Ophthalmic Services Contract (GOS) system and are employed by GOS contractors. A significant number of optometrists work as self-employed locums. Many optometrists work in salaried positions within hospital ophthalmology departments. Hospital optometrists are likely to be assisting urgent and emergency eye care in the hospitals under the supervision of ophthalmologists. The General Optical Council currently registers around 30,000 optometrists, dispensing opticians, student opticians, optometrists, pre-registration optometrists and optical businesses across the UK, we estimate 90% of this capacity is in England.
8. Key stakeholders
- General Optical Council
- The College of Optometrists
- The Optical Confederation
- NHS England and NHS Improvement
- NHS trusts
- Indemnity organisations (Association of Optometrists, Federation of Ophthalmic and Dispensing Opticians, Association of British Dispensing Opticians, Specsavers)
- NHS Business Services Authority
- Department of Health and Social Care
- Public Health England
9. Competencies and mapping of potential roles
Table 1: Key training and supervision
| LOW | A few hours local induction training required |
| MODERATE | Up to three days training required |
| HIGH | Formal course or qualification required |
Table 2: Competencies and mapping of potential roles
| Sector | Job List | Who can do this | Training Need | Supervision Level |
| A&E
(better suited to current hospital employed optometrists) |
Donning of PPE on self and others | Dispensing opticians | Local training induction | None |
| Patient observations (O2 saturations, blood pressure monitoring, respiratory rate, heart rate) | Optometrists / dispensing opticians | High (National Early Warning Scoring System) | Low | |
| Patient History Taking | Optometrist / Dispensing Opticians | Low (but may need to tailored to specific clinical specialty) | None | |
| Ophthalmic triage (with referral to appropriate urgent/essential/emergency eye care) | Optometrists / dispensing opticians | None | None | |
| Ophthalmic drug prescribing (POM classification) | Independent prescribing optometrists | None | None | |
| Ophthalmic drug prescribing (P or GSL classification) | optometrists | Low | None | |
| Wound dressing | Optometrists / dispensing opticians | Wound care training / moderate | Low | |
| Blood glucose measurements | Optometrists / dispensing opticians | Practical demonstration | Low | |
| “Specialising” (prolonged close observation) of patients in certain situations | Optometrists / dispensing opticians | Locally tailored training | High | |
| Keeping medical records (paper and computer) | Optometrists / dispensing opticians | None (but may need to tailored to specific clinical specialty) | None | |
| Talking to patients and relatives | Optometrists / dispensing opticians | None | None | |
| Cannulation | Optometrists / dispensing optician | High | High | |
| Phlebotomy | Optometrists/ dispensing optician | High | High | |
| Reception administrative duties | Optometrists / dispensing opticians / non-registered optical staff | Systems training | Low | |
| Suturing | Optometrists / dispensing optician | High | High | |
| Learning and performing new tasks as required | Any member of the optical team | As required | As required | |
| Critical Care | Patient hygiene | Optometrists / dispensing opticians | None | None |
| Donning of PPE | Dispensing opticians | Local training induction | None | |
| Conversation | Optometrists / dispensing opticians | None | None | |
| Eye care | Optometrists / dispensing opticians | None | None | |
| Record observations | Optometrists / dispensing opticians | Locally tailored training | None | |
| Audit / research data | Optometrists / dispensing opticians | None | None | |
| Dressing care | Optometrists / dispensing opticians | Wound care training | High | |
| Pressure areas observation | Optometrists / dispensing opticians | Locally tailored training | High | |
| Range of movement exercise after assessment by, and under advice of, a physiotherapist | Optometrists / dispensing opticians | Locally tailored training | Moderate | |
| Escalation of concerns | Optometrists / dispensing opticians | None | None | |
| Housekeeping | Any member of optical team | None | None | |
| Note taking | Optometrists / dispensing opticians | None | None | |
| Result chasing | Optometrists / dispensing opticians | System training | Low | |
| Bookings | Optometrists / dispensing opticians | System training | Low | |
| Referrals | Optometrists / dispensing opticians | Locally tailored training | Moderate | |
| Learning and performing new tasks as required | Any member of the optical team | As required | ||
| General Hospital | Porter services | Any member of the optical team | Lifting and handling training | Low |
| Housekeeping | Any member of the optical team | None | None | |
| Donning of PPE | Dispensing opticians | Local training induction | None | |
| Talking to patients and relatives | Any member of the optical team | None | None | |
| Healthcare assistant duties | Optometrists / dispensing opticians | None | None | |
| Learning and performing new tasks as required | Any member of optical team | As required | ||
| General Medical Practice | Immunisations and vaccinations | Optometrists / dispensing opticians | Immunisations Training | High |
| Administrative duties | Any member of the optical team | None | None | |
| Patient triage | Optometrists / dispensing opticians | System training | Moderate / High | |
| Donning of PPE | Dispensing opticians | Local training induction | None | |
| Decontamination/Infection Control of surgeries | Optometrists / dispensing opticians | Low | Low | |
| Phlebotomy | Optometrists/ dispensing opticians | High | High | |
| Patient observations (e.g. blood glucose monitoring) | Optometrists / dispensing opticians | Low | Low | |
| Learning and performing new tasks as required | Any member of optical team | As required | ||
| Ambulance Service | Decontamination of units | Optometrists / dispensing opticians | Low | Low |
| Stocking of Units | Optometrists / dispensing opticians | Local induction / manual handling | Low | |
| Buddy to team | Optometrists / dispensing opticians | None | None | |
| Donning of PPE on others | Dispensing opticians | Local training induction | None | |
| Learning and performing new tasks as required | Any member of optical team | As required | ||
| NHS 111 | Eye care triage | Optometrists / dispensing opticians | Systems training | None |
| Learning and performing new tasks as required | Any member of optical team | As required | ||
| Pharmacies | Current collaboration between the GOC, General Pharmaceutical Council and Royal Pharmaceutical Society | To determine how optometrists/dispensing opticians can assist in community pharmacy tasks | As required | Low |
| COVID-19 Related testing | If a need arises for clinical rooms across the nation for use of potential testing of healthy patients (or COVID-19 suspect patients with appropriate PPE and infection control facilities). Practices are located across the country and in most rural areas | All optical practices have at least one secluded consultation room with basic hand wash facilities. Now most are vacant as routine sight tests are suspended | Appropriate waste disposal facilities and infection control facilities | Could ease the burden on GP practices and pharmacies |
| This is a potential future workforce need. | Optometrists / dispensing opticians | COVID-19 testing training | Moderate | |
| Social Care | Delivery of medicines | Any member of optical team | None | None |
| Delivery of food / necessities | Any member of optical team | None | None | |
| Domiciliary Eye Care | Domiciliary optometrists and dispensing opticians | None | None | |
| Social interaction | Any member of optical team | None | None | |
| Personal care | Any member of optical team | None | None | |
| Cooking | Any member of optical team | None | None | |
| Cleaning | Any member of optical team | None | None | |
| Learning and performing new tasks as required | Any member of optical team | As required | Learning and performing new tasks as required |
10. Indemnity arrangements – England
The Coronavirus Act 2020 enables existing indemnity arrangements to be complemented by covering any gaps. This is only applicable where adequate cover is not otherwise provided for the relevant activities carried out in relation to the COVID-19 response.
The Clinical Negligence Scheme for Trusts (CNST) will provide cover for retired healthcare workers who return to work for NHS trusts and is the vehicle for covering other gaps. The Clinical Negligence Scheme for General Practice (CNSGP) will cover returning healthcare workers who work for general practices undertaking normal NHS contracted work. Cover would need to be provided by the CNST for any volunteers from the optical workforce, especially if they are working outside of their capacity as a GOC.
11. Remuneration considerations
Those members of the optical workforce who are not on a trust payroll will need reassurance that their roles will be remunerated.
12. Induction
Health Education England have developed training and induction modules to help the healthcare workforce respond to COVID-19. These modules are useful to aid the upskilling of the workforce and prepare for redeployment.
Appendix 1: Transferable competencies
The optical workforce should be allocated to tasks according to their competency and skill set, as set out below. All GOC registered optometrists and dispensing opticians should have achieved the following competencies upon registration:
| Optometrists |
| Obtain, interpret and record an accurate history that incorporates appropriate optical, medical (including medication history and allergies), social, demographical, cultural, nutritional, psychological and genetic factors. |
| Have high level of numeracy and scientific skills. |
| Recognise the signs of abuse or neglect in vulnerable groups or Protect risks and the local procedures that should be followed when reporting such circumstances. |
| Generate a differential diagnosis and treatment / management plan based on evidence from an eye care health assessment / urgent care assessment and risk screening, through the correct interpretation of clinical findings. |
| Implement, perform and manage effective decontamination and infection control. |
| Identify medical emergencies. |
| Safely and appropriately administer ophthalmic diagnostic medicines (therapeutic ophthalmic agents for independent prescribing optometrists) |
| Keep clinical records (conventional and or electronic) in line with current national guidance. |
| Dispensing Opticians |
| Obtain, interpret and record an accurate history that incorporates appropriate optical, general health, medication, family history, work, lifestyle and personal requirements. |
| Have high level of numeracy and scientific skills. |
| Some would have training in recognising the signs of abuse or neglect in vulnerable groups or Protect risks and the local procedures that should be followed when reporting such circumstances. |
| Be able to recommend suitable products and devices based on evidence from a sight test, through the correct interpretation of a sight test. |
| The ability to implement and perform effective decontamination and infection control. |
| Safely and appropriately dispense and fit spectacles to patients, competency could prove useful in the safe donning of personal protective equipment on others. Experience of fitting safety eyewear Repairing and replacing spectacles for patients and keyworkersKeep clinical records (conventional and or electronic) in line with current national guidance. |
Appendix 2: Questions and answers for volunteers
General
In what ways can I support the coronavirus (COVID-19) response?
The coronavirus (COVID-19) outbreak is unprecedented and is affecting all aspects of society. You can assist with the response to coronavirus in many ways by:
- Follow guidance outlined on the NHS England and NHS Improvement website.
- Offer assistance to vulnerable members of your local community at: https://www.goodsamapp.org/NHS.
Might my practice environment be utilised during the response to COVID-19?
An optical practice is a clinical environment that potentially may be of benefit in some local areas. There are, however, no current plans in place to utilise optical practices as part of the immediate or surge responses to COVID-19.
Can I help without being directly in a patient facing role?
There are opportunities to work in roles such as NHS 111. These roles will be available firstly to those individuals who are at increased risk of a severe response to coronavirus, such as individuals with comorbidities.
In what geographical location might I be expected to work?
There is likely to be increased demand across the entire NHS in England and therefore you will be offered opportunities as close to your requested area as is reasonably practical. There may be an element of key worker travel involved.
Will I be tested for coronavirus before my deployment?
We expect that as testing capacity increases this may become available to all NHS workers.
Will I be sent to multiple different locations?
To minimise the need for training and induction, it is highly likely that once you have commenced work in a particular team, you will remain as part of that team until demand subsides, and you can return to normal clinical practice.
I am working in an education / research role, can I still help?
Of course. You are a highly skilled and knowledgeable member of the healthcare workforce. You will have the opportunity to work within your own clinical competencies but potentially outside your traditional comfort zone.
Will I be provided with personal protective equipment?
You will be provided with the appropriate personal protective equipment, as recommended by the government, to safely fulfil each role you work in. The safety of NHS Staff and patients is of utmost importance.
Are all members of the optical team able to offer services?
Assistance and support is required in a wide variety of both clinical and administrative roles. All members of the optical team will therefore have a vital role in providing an effective response to coronavirus (COVID-19).
When is this likely to start?
There is no exact or defined date as to when this additional support is needed. This will vary and be dependent on the specific demands of a local area, at a particular time.
If I change my mind about volunteering during my service am I able to withdraw?
Yes, however, we would encourage you to commit to a minimum period in discussion with your local placement.
Training
Will I need to learn new skills?
This is dependent on your current experience and skillset. You will be assigned a role and task that is closely aligned with your current competencies. If there is a need for training or orientation, this will be provided via an induction programme.
Who will I go to if I have any concerns / questions once I am redeployed?
There will be a central point of contact at the location you have been deployed to.
Personal health
What if I am pregnant?
The government has advised that you should be particularly stringent in following social distancing measures. This does not specifically mean you cannot work. You should, however, have a risk assessment undertaken at work and where possible work from home or work more remotely, potentially in a non-clinical facing role. Further information on what measures to follow is available here.
What if I have a chronic disease?
The government has advised individuals with particular conditions to stringently follow social distancing measures. Please see the list of conditions/diagnoses outlined here. This does not specifically mean you cannot work. You should however have a risk assessment undertaken at work and where possible work from home or work more remotely, potentially in a non-clinical facing role. Further information on what measures to follow is available here.
What if I develop symptoms of coronavirus (COVID-19)?
If you develop symptoms of coronavirus current public health advice on testing and management of staff should be followed. If at work at the time of developing symptoms you should immediately inform your line manager and withdraw from work.
What if someone in my family develops symptoms of coronavirus?
If someone in your family / household develops symptoms of coronavirus current public health advice on testing and management should be followed. Further information on how to manage this situation is available here.
What if I become ill while I am working?
If you become unwell, while working, please notify your designated point of contact.
What if a member of my household is a vulnerable individual?
Given the increased risks of coronavirus, in certain groups (see here), we would advise against returning to patient-facing clinical work if you are a carer to someone in an at risk group. However, there are a range of opportunities in non-patient facing roles that we are in urgent need of support with. This includes assistance with clinical triaging via the NHS111 pathway.
Contractual and remuneration
I am self-employed, can I still help?
You are indeed a valuable, highly skilled and trained individual. Your services will be invaluable in providing safe, effective and timely care to patients.
I work part-time, can I still help?
You will be able to help in a part-time capacity and may even have the opportunity to increase your working hours if desired. A workforce rota will be designed to suit the availability of all staff. Please discuss your availability with the designated point of contact.
How will I be paid?
If you work as a salaried hospital optometrist, your salary will be paid for as usual. If not, your voluntary commitment will be incredibly welcome. Furloughed workers would be able to volunteer without effecting their status with their employer.
Will my pension contributions be maintained?
Your NHS pension contributions will continue as normal if you are NHS employee.
Will I have an employment contract?
No, you will not have an employment contract; however, there will be an agreement with your allocated placement.
How long will I be expected to help?
The expected length of this outbreak is estimated to be around 12 weeks. However, this time period is not definitive and is subject to change. Assistance and support, from the wider healthcare community, will be necessary until the surge in COVID-19 has been effectively and safely managed.
Will I have a rota / need to work specific hours?
It is likely you will work specific hours and as part of a wider rota. This will of course be planned and designed in such a way that it meets the surge demand on the system. You will be asked for your availability and, where possible, will be given shifts aligned with your stated availability.
Scope of practice
What roles might I be expected to do?
We recognise that optical staff have many competencies that are transferrable to the medical environment. There are multiple possible roles that you might be expected to take on, depending on where you work. This may be within a hospital, ward environment or within a local GP practice. You will not be asked to fulfil a role that you do not have the training or support to safely perform.
Will I be asked to work in a role I am not familiar with?
As far as possible, we will aim to match optical staff to the most suitable roles in line with their capabilities. In some situations, you may need to be placed in higher, less or unskilled roles. Where this is necessary, you will be supported adequately to take on these roles and should only work within the limits of your competency. Training and supervision will be given.
Can I reject a role, if I am not confident it aligns with my skillset?
As the COVID-19 pandemic progresses, it is likely that doctors will have to work outside their normal field of practice which has been acknowledged by the General Medical Council. A similar arrangement may be required for optical professionals. Defence organisations advise that any professional having concerns about clinical responsibilities outside their clinical competence should clearly outline their concerns to the clinical / medical director managing the service. If further advice is required, please contact your indemnity defence organisation.
I am working in an educational or research role, what are the next steps for me?
If you have an honorary clinical contract, your organisation will contact you to discuss whether you are prepared to postpone your educational / research activities in the short term (unless working on education or research in relation to COVID-19) to provide more clinical support in the workplace. Those with teaching expertise may be able to help provide induction for new staff – for example, environmental orientation, the use of PPE, managing high flow oxygen of ventilated patients (if appropriately trained to do so).
Indemnity
My current indemnity only covers optometry / ophthalmic dispensing practice, what are my options?
It is important to remember, that trust indemnity will exist for all those working for and on behalf of an NHS trust and this would extend to volunteers. As regards to eye care, NHS England will consult with the main optical defence organisations (AOP, FODO and Specsavers, ABDO) to ensure coverage for working within core skills and simple notification systems where necessary.
Will any cost of alteration to my indemnity be paid for by the NHS?
For any optical workforce volunteers providing services outside of their capacity as a GOC Registrant, CNST will provide indemnity cover. Therefore, we do not anticipate any required alteration to your current indemnity cover.
Appendix 3: Self-assessment competency reporting framework
| Competency Assessment | |
| Name | |
| Email address | |
| Telephone number | |
| Job title | |
| GOC Number (if registered) | |
| Skill | Competent Yes (Y), with initial supervision (S), No (N) |
| Oxygen monitoring using a pulse oximeter | |
| Blood pressure monitoring using automated equipment | |
| Blood glucose measurement | |
| INR measurement using a Coagucheck | |
| Peripheral IV access (cannulation) | |
| Phlebotomy (taking blood) | |
| Administration of IV drugs | |
| Up to date BLS training | |
| Up to date ILS training | |
| Skin suturing | |
| Personal protective equipment donning on self and others (such as safety eyewear and others) | |
| Wound dressing | |
| Infection control | |
| Additional qualifications PLEASE STATE: |
For example, medicine/nursing / midwifery/ pharmacy/ paramedic/MECS/low vision/independent prescriber/contact lens optician |
| Please provide any other relevant information or describe any skills you are able to offer in addition to those listed above | |
| Do you have any compromising conditions that would prevent you working in different areas of the hospital? (Y/N) | |
| Do you have any dependants? (Y/N) | |
| Would you be able to work in evenings/ weekends if necessary? (Y/N) | |
