Fire Risk Assessment: Guidance on completing specific FRA for temporary wards provided for Covid-19 treatment or care
Contents
Classification: Official
Publication approval reference: 001559 / C0131
Novel coronavirus (COVID-19) standard operating procedure
Fire Risk Assessment: Guidance on completing specific FRA for temporary wards provided for Covid-19 treatment or care
To be used in conjunction with HTM 05-03: Part K
This guidance is correct at the time of publishing (06 April 2020). However, as it is subject to updates, please use the hyperlinks to confirm the information you are disseminating to the public is accurate.
Risk Assessment guidance
Fire Risk Assessment: Guidance on completing specific FRA for temporary wards provided for Covid-19 treatment or care
To be used in conjunction with HTM 05-03: Part K
| Responsible person | ||
| Address | ||
| Specific area | ||
| Assessor | ||
| Date | ||
| Person consulted | ||
| Suggested review period | Daily/weekly depending on risk |
Temporary wards may have the following risk factors:
- Patients who have very high dependency.
- Areas not specifically designed for patients, which may not meet guidance on fire compartmentation and progressive horizontal evacuation.
- Large numbers of patients supplied with oxygen up to 10 litres per minute.
- Possibility of oxygen concentrations exceeding those generally found in the atmosphere- less risk if effective ventilation or large volume i.e. high ceilings.
- Staff who may not normally work together
- Staff who may not be familiar with the area
- Staff not trained in fire safety, progressive horizontal evacuation or oxygen isolation for the specific area.
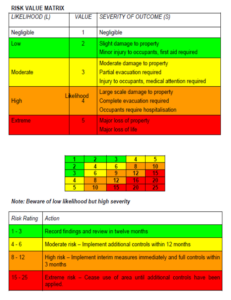
Fire risk assessment – significant findings & action plan (see matrix at Appendix 1 risk rating)
Area/location:
| Findings | Action required | Interim control measures | Risk rating | Person responsible for completing | Date completed |
The following items should be considered and each given a risk rating (RR= see matrix at end):
Step 1: Identifying hazards
| RR | Ignition sources | Yes | No |
| Are reasonable measures taken to prevent sources of ignition? | |||
| Electrical equipment kept to a minimum in appropriate areas? | |||
| Is the use of products which on coming into contact with Oxygen may ignite such as petroleum jelly, sprays, hair and body oils controlled? | |||
| The use of portable electrical equipment such as mobile phones, laptops electronic weighing scales not permitted close to patients? | |||
| Reasonable steps taken to reduce the risk from static electricity in oxygen rich areas such as using cotton fabrics where possible? |
Comments and hazards observed:
| RR | Fuel | Yes | No |
| Are there reasonable steps to prevent the accumulation of waste materials? | |||
| Is the use of oil, grease, paper or other combustible materials kept to a minimum? | |||
| Is the use of textiles and furniture kept to a minimum and where used has a suitable level of fire performance? | |||
Comments and hazards observed:
| RR | Oxygen | Yes | No |
| Is the area well ventilated either naturally or mechanically so as to prevent an accumulation of oxygen? | |||
| Are there suitable controls over the storage and use of oxygen cylinders? | |||
| Are there suitable controls for medical gas pipeline system such that it can be easily isolated in an emergency? | |||
| Are staff trained in isolating oxygen, including procedures for ensuring continuing supplies for patients? |
Comments and hazards observed:
Step 2: Identifying persons at risk
| RR | Type of person | Y/N | number |
| Dependent patients? | |||
| Very high dependency? | |||
| Medical staff | |||
| Cleaning staff | |||
| Other staff | |||
| Others- define in comments below |
Comments and hazards observed:
Step 3: Evaluate, Remove or Reduce and protect from risk
| RR | Cause and ignition source | Y | N |
| Are risks from patients contaminated by oil or grease (emollient) coming into contact with high oxygen concentration and spontaneously igniting avoided? | |||
| Alcohol hand sanitiser, is alcohol permitted to evaporate before treating patient? | |||
| Is the risk from electrical equipment causing ignition in oxygen rich environment minimised? | |||
| Are all staff advised to avoid personal electrical equipment in potentially oxygen enriched atmosphere? | |||
| Are there suitable fire extinguishers and fire blankets easily available? | |||
| Means of escape | |||
| Can patients be easily moved away from a fire? | |||
| Are escape routes free from obstruction? | |||
| Are escape routes available to use at all times- e.g. emergency lighting adequate? | |||
| Are there suitable systems in place for the safe storage and use of oxygen cylinders? |
Comments and hazards observed:
Step 4: Record, plan, inform, instruct and train
| RR | Y | N | |
| Is there an emergency plan which has been tried and tested by talking through with relevant staff? | |||
| Does the emergency plan identify how and by whom the oxygen supply can be isolated? | |||
| Does the emergency plan identify alternative supplies of oxygen for patients? | |||
| Does the emergency plan identify locations to move patients to? | |||
| Is there a staff information sheet covering the risk from fire which all new staff must read? (see appendix) | |||
| Are staff provided with induction training which includes fire safety? | |||
| Are staff (including ancillary) trained in the dangers from oxygen rich atmosphere and oxygen safety? | |||
| Are medical staff trained in the safe use of oxygen including cylinders? | |||
| Are staff trained in the use of fire extinguishers? | |||
| Are suitable fire extinguishers and blankets easily accessible? | |||
| Does the plan identify who will call the fire brigade and access routes? |
Comments and hazards observed:
Step 5: Review
| Date | Any changes? | Previous actions completed? | New actions? | Name |
Appendix 1: Risk value matrix
Appendix 2: Example staff information sheet
Fire Safety Information: Guidance to staff in temporary wards provided for Covid-19 treatment or care
You will be working in an area which may not specifically be designed for the care of very high dependency patients who are on oxygen enhanced ventilators. In an oxygen rich environment (a 2% increase over normal levels) fires start very easily and burn fiercely
- Avoid bringing ignition sources such as mobile phones, computers and pagers close to patients on oxygen.
- Do not use oil-based emollients or alcohol-based sanitiser on patients on oxygen or on yourself if you are close to them. Allow alcohol to evaporate a safe distance away first.
- Keep areas clear of accumulated items that can burn such as bedding or paper, control waste.
- Know your fire procedures, how to raise the alarm, including shouting “fire,fire,fire”, how to evacuate patients and where to take them. Who will call the fire brigade?
- Where are your fire extinguishers? Read the instructions on them and pick them up so you know what they feel like and how to use them.
- Ensure that there is a good level of ventilation, mechanical or natural, don’t let oxygen levels build up.
- Where are your oxygen isolation points? How do you operate them? Who will operate them? What oxygen supplies do they isolate and to whom?
- Once oxygen is isolated, how are patients provided with oxygen? Are there sufficient O2 cylinders?
- Oxygen cylinders explode in fires. Are there effective procedures in place for their storage and deployment? Are staff trained in their safe use?