Frontline social care workers standard operating procedure – updated to reflect phase 3 of the COVID-19 vaccination programme
Contents
Supplementary guidance for Phase 3
Annex 1 – Standard Operating Procedure for Phase 1
- Purpose
- Scope
- Roles & Responsibilities
- Appendix 1 – Framework for Eligibility
- Appendix 2a– National Offer Letter
- Appendix 2b: Consent Form
- Appendix 3: Local Authority Notice of Eligibility
- Appendix 4: Example of Local Authority Template with minimum data requirement
- Appendix 5: Process for those booking via National Booking Service
Classification: Official
Publication approval reference: C1430
Version 2, 13 October 2021
Updates made to this document to reflect phase 3 of the COVID-19 vaccination programme are highlighted in yellow
Glossary
| CCG | Clinical Commissioning Group |
| CHIP | Care & Health Improvement Programme, which is part of the LGA |
| CQC | Care Quality Commission |
| DWP | Department for Work and Pensions |
| ‘Evergreen’ offer | This is an open invitation to anyone who is eligible to receive their vaccination, 1st and/or 2nd dose, if they haven’t yet had them. |
| HH | Hospital Hub |
| ICS | Integrated Care System |
| JCVI | Joint Committee on Vaccination and Immunisation |
| LVS | Local Vaccination Service |
| LA | Local Authority |
| NBS | National Booking Service |
| NHS | National Health Service |
| NIMS | National Immunisation Management System |
| NIVS | National Immunisation Vaccination System |
| Phase 1 | JCVI cohorts 1 to 9 |
| Phase 2 | JCVI cohorts 10 to 12 |
| Phase 3 | Phase 3 is when booster doses should be given to Cohorts 1-9 as set out in the JCVI statement of 14 September 2021.
In this Phase, unpaid carers including adults aged 50 years and over, and adults aged 16-49 who are in an influenza or COVID-19 at risk group will be offered a ‘booster’ vaccine no earlier than 6 months after their second dose, to enhance vaccine protection against COVID-19. JCVI advises that the booster programme should be deployed in the same order as during Phase 1 (priority groups 1-9), with operational flexibility exercised where appropriate to maximise delivery. |
| PHE | Public Health England – PHE has now been replaced by UK Health Security Agency and Office for Health Improvement and Disparities |
| PCN | Primary Care Network |
| RVOC | Regional Vaccination Operations Centre |
| SOP | Standard Operating Procedure |
| SRO | Senior Responsible Officer |
| SVOC | System Vaccination Operations Centre |
| S4C | Skills for Care |
| STP | Sustainability and Transformation Partnership |
| VC | Vaccination Centre |
Supplementary guidance for Phase 3
1. Overview
This updated Standard Operating Procedure (SOP) supports the deployment of the COVID-19 booster vaccinations to frontline social care workers in line with JCVI guidance issued 14 September 2021. That guidance advises that those who are more at risk from serious disease and who were vaccinated during Phase 1 (priority groups 1 to 9) should be included in the booster programme.
All social care workers previously prioritised in cohorts 1 and 2 are covered by this supplementary Phase 3 guidance. The guidance on pages 5 to 18 sets out how eligible frontline social care workers can access COVID-19 booster vaccinations and how those social care workers yet to access the full course of the COVID-19 vaccine can access the ‘Evergreen’ offer. Annex 1 is the original Phase 1 SOP.
This guidance builds on lessons learnt since social care workers were first called for COVID-19 vaccinations and includes several key changes:
- The delivery model has been simplified. In line with national guidance on consent for vaccinations, the national letter for consent, the social care worker consent form and the Local Authority letter of eligibility from Phase 1 are no longer required for the primary or booster vaccinations.
- Amendments have been made to the eligibility criteria set out for Phase 1 to reflect legislation on vaccination as a condition for deployment* (see section 2).
- Updating the Local Vaccination Service Community SOP and the Roving and Mobile Models SOP so the workforce in all CQC registered care homes can access workplace based vaccinations through this delivery model.
- Introducing pop-up, walk-in and mobile delivery sites and updating the Local Vaccination Service Roving and Mobile Models SOP so eligible frontline social care workers from all social care settings (i.e. care homes, home care, community care such as supported living extra care and those who work as personal assistants) can all access the above sites without a pre booked appointment, no earlier than 6 months after completion of their primary vaccine course. Individuals who use the pop-up and walk-in clinics must provide proof of employment in the priority occupational cohort of health and social care workers (HSCWs) at the vaccination site.
- The National Booking Service (NBS) is open to all adults to book first and second doses. A new self-referral pathway in the NBS will allow eligible health and social care workers to make priority bookings for booster vaccinations, no earlier than 6 months after completion of their primary vaccine course. Individuals who book using this pathway must also provide proof of current employment as a social care worker at the vaccination site.
*Regulation 5 amendment: This provides that for the purposes of preventing, detecting and controlling the spread of infection, registered persons (“A”) in respect of the regulated activity of providing residential accommodation together with nursing or personal care in a care home, must secure that a person (“B”) does not enter the premises used by A unless B meets specific requirements.
These changes to delivery models and ways to access them impact on actions needed to support the delivery, uptake and reporting of vaccinations to social care workers. These have been updated for Phase 3 and are set out in section 3.
2. Scope
As all adults are eligible for the ‘Evergreen’ offer, priority access to COVID-19 vaccinations is no longer a requirement for social care workers. Advice in The Green Book that young people aged 16 -18 who are employed in, studying or in training for health and social care work should be offered the vaccination alongside their colleagues also remains unchanged. However, in the light of new guidance on vaccinating all 16 and 17 year olds in the general population, the sector should be aware of the specific guidance for these social care workers, and that they should receive two doses of the Pfizer vaccine (see page 19).
Operational guidance governing the clinical delivery of the vaccine is covered in the LVS SOP. This supports clinical guidance issued by both the JCVI and Public Health England (PHE). Key links are provided in this guidance.
Changes to Social Care Workers in scope for Phase 3
In line with legislation on vaccination as a condition for deployment, eligibility for priority booster vaccination is now extended to include all social care staff working in settings where COVID-19 vaccinations are a statutory requirement.
As in Phase 1 the Local Authority Director of Adult Social Services will continue to have ultimate responsibility for determining social care workers eligible for priority booster vaccinations. This should continue to be based upon the principles established in Phase 1; that social care workers providing close and regular care to those clinically vulnerable to COVID-19 are eligible. Taking into account statutory changes affecting staff working in settings where vaccination is a condition for deployment, all social care workers in care homes are now eligible for priority vaccination, irrespective of whether they provide face to face care or not.
As in Phase 1 some groups are not eligible within this priority group as defined by the JCVI:
- Administrative staff who do not have any direct contact with clients and who work in settings other than care homes are not eligible for priority booster vaccinations.
- Social care workers working with children who are not considered a priority within the context of the JCVI priority cohorts 1-9 (children under 16 who do not have underlying health conditions leading to greater risk of disease or mortality and children who have no underlying health conditions) are not eligible for priority booster vaccinations.
Unpaid carers are eligible for priority boosters as set out in this operational guidance.
Appendix 1 provides more detail on eligibility and offers a framework for use locally.
3. Roles and responsibilities
3.1 Overview of process
The JCVI has stated the objective of the COVID-19 booster programme is to maintain high levels of protection during winter among individuals who are more at risk of serious disease. This includes the social care workforce, which is vulnerable due to occupational exposure. The social care workforce is highly diverse and therefore includes individuals who are at greater risk of serious disease due to certain protected characteristics, such as ethnicity, and social deprivation.
Strong partnership working between providers and employers, Local Authorities, the Department of Health and Social Care and the NHS should continue to focus on actions to enhance uptake of the ‘Evergreen’ offer. Promoting both the ‘Evergreen’ offer and booster vaccinations will enhance and prolong the protection given to social care workers, by maximising protection against occupational exposure and improving health inequalities.
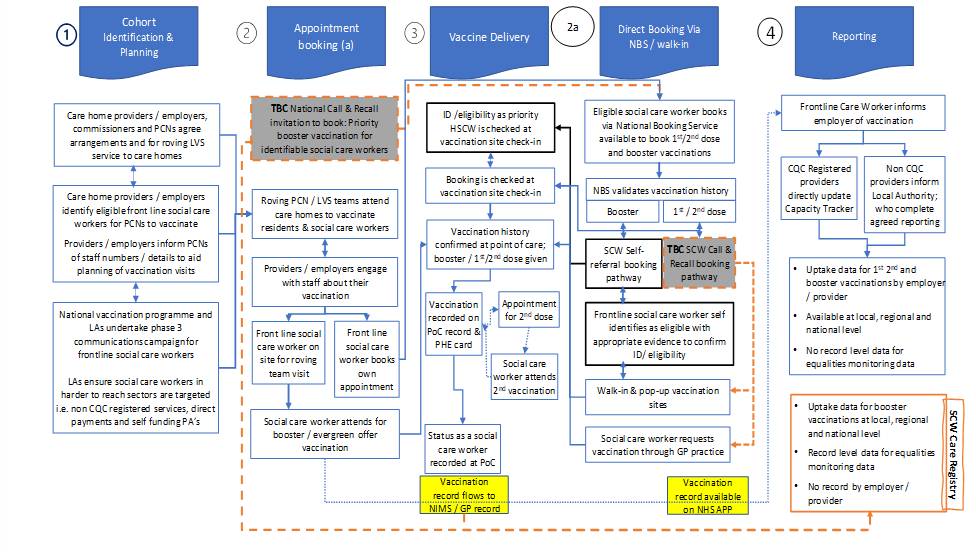
A high level summary of the process for priority booster vaccinations in Phase 3 is shown in figure 1 and includes:
- PCN teams which will vaccinate residents and staff in all adult care homes.
- Access to the NBS for first and second doses or priority booster vaccinations, subject to the course of COVID-19 vaccinations being due and the individual providing proof of employment for a priority occupation cohort.
- Community pharmacies, vaccination centres, some hospital hubs and PCN sites can also be accessed through the NBS.
- LVS sites can vaccinate eligible SCWs at pop-up, walk-in and mobile sites, subject to the course of COVID-19 vaccinations being completed more than 6 months earlier and the individual providing proof of employment within a priority occupation cohort.
Work to implement call and recall for as many SCWs as feasible during Phase 3 will align with business as usual processes for other cohorts, starting with those who made NBS bookings in Phase 1 and moving on to use other management information (subject to Information Governance). This will provide data to improve monitoring and reporting.
Specific actions are set out in section 3.3.
Figure 1: Rollout to social care workers in Phase 3
3.2 Local arrangements to maximise access and uptake
During Phase 1, health and social care workers initially accessed priority vaccinations through hospital hubs. PCN networks supported care homes and some vaccination centres provided block bookings for social care workers in cohort 2.
In February 2021 a self-referral booking route was opened within the NBS to improve local access. This provided flexibility for social care workers to self-refer and book online or over the telephone.
It continues to provide flexibility for social care workers to book as part of the ‘Evergreen’ offer to all adults.
A self-referral pathway will support priority access to booster vaccinations in Phase 3. The booking process will verify vaccination history to ensure a booster vaccine is due and it will prompt individuals to book any outstanding dose of the COVID-19 vaccine. The vaccination programme now offers access at hundreds of walk-in centres across the country without the need to book in advance using www.nhs.uk/grab-a-jab walk-in, mobile and pop-up sites. It will also verify vaccination history as above.
The uptake for both first and second dose vaccinations among social care workers is above or comparable to that of the general population in older people’s and younger adult care homes. It is however below that of the general population in other social care settings.
As in Phase 1, all organisations and employers within the local health and social care system should ensure the local approach to reach eligible social care workers considers: a) equality of access and health inequalities by following JCVI advice and b) the adult social care risk reduction framework to prioritising those staff at high risk.
All organisations and employers within the local health and social care system should continue to take steps to reach frontline social care workers eligible for the ‘Evergreen’ offer, COVID-19 booster and Flu vaccine. They should work collaboratively to build on national measures such as the infection control fund, multilingual resources and evidence based practices using the extensive resources which were developed during Phases 1 and 2 to build vaccine confidence which include:
- bespoke communications materials (posters, videos, leaflets, and shareable social media assets) shared across a variety of channels
- a paid advertising campaign targeting social care workers with digital advertising to build vaccine confidence and encourage use of the National Booking Service
- a stakeholder toolkit (Q&As, guidance and communications materials)
- positive messages using influencers, leaders and care home workers who have already been vaccinated to boost confidence and tackle misinformation
- content in different languages and briefings with different faith groups who have expressed interest in co-creating vaccine content
- webinars for social care workers, including those where clinical experts answered social care workers’ questions and concerns about the vaccine
- good practice for increasing vaccine confidence and uptake among ethnic minority groups, such as the Bridging the Uptake Gap BABAC toolkit.
Many local systems have also developed resources and measures to support those with low vaccine confidence and in hard to reach groups. These should continue to be developed and good practice shared to cover concerns such as vaccination linked to family planning and pregnancy, needle phobia and understanding exemptions linked to vaccination as a condition for deployment. Further resources to support winter vaccinations for social care workers can also be found here.
3.3 Actions required
3.3.1 Local Authorities
The Department of Health and Social care will work with Local Authorities to find ways to achieve a reasonable level of data collection without creating unrealistic expectations or placing an undue burden on Local Authorities – with the aim of replacing the existing process with improved vaccination programme data capture and reporting for social care as soon as this is feasible.
Local Authorities are responsible for:
- Providing consolidated information on vaccination uptake via the national Capacity Tracker for their own directly employed frontline social care workers working in non-CQC regulated services.
- Working with the Department of Health and Social Care to seek and gather information on vaccination uptake for non-Local Authority employed frontline social care workers in non-regulated settings.
- Continuing to encourage providers to regularly update their vaccination data on Capacity Tracker.
- Working with CHIP/LGA to maintain the local point of contact list for support with any issues relating to frontline SCW vaccination and ensure the list the LGA hosts on its website is up to date.
- Working with the CQC, local resilience forum partners and ICSs to co-promote COVID-19 boosters and flu vaccines for all eligible frontline social care workers in their area, in line with JCVI and PHE guidance (with groups who are eligible for the influenza immunisation programme detailed in appendix A).
- In partnership with the local NHS and public health vaccination leads, ensuring there are evidence-based resources and approaches in place within social care settings to support uptake of the ‘Evergreen’ offer among social care workers with protected characteristics, who are known to have low vaccine confidence. They should also continue practical support for employers of care workers, or individuals facing difficulties in arranging vaccination and ensure this is extended to cover booster vaccination.
- Local Authorities should ensure a branded template letter of authority is made available to employers of PAs to ensure that where requested during the vaccination appointment, the necessary evidence of employment can be provided. (In this context branded means that the template should be based on official letter headed paper for the upper tier Local Authority (i.e., with responsibility for Adult Social Care).
3.3.2 Local NHS Vaccination Programme Leads
The Senior Responsible Officer for the local Vaccination Programme is responsible for:
- Working with LVS Roving teams to ensure coverage for all care homes to provide access to the ‘Evergreen’ offer for staff and residents; including plans for co-promotion and co-administration of COVID-19 boosters and Flu vaccinations where operationally practical and in line with JCVI clinical advice for the COVID-19 booster programme.<mark/
- Ensuring that Hospital Hubs, Vaccination Centres and Local Vaccination Services have included preparations to vaccinate this cohort as part of their capacity and operating plans.
- Ensuring that arrangements to validate the identity of eligible frontline care staff for priority booster vaccinations are clearly communicated within the local system and followed during the site check-in process to safeguard against unauthorised use.
- Continuing to ensure the use of robust administrative and data collection systems using NIMs/NIVs or Pinnacle to support the effective delivery of the programme and any local, regional, or national monitoring requirements. This includes the point of care data collection for the clinical event of vaccination and recording individuals’ status as a social care worker or as care home. This will support regional and national oversight in monitoring vaccine uptake by this cohort.
- Ensuring vaccination delivery sites are responsive to changes in data collection systems.
3.3.3 Providers/employers of social care workers
- Providers/employers (which may include the Local Authority and NHS organisations) employing eligible frontline social care workers are responsible for:
- Ensuring all relevant employees are aware of the national offer for priority booster vaccinations and how they can access these and the ‘Evergreen” offer through the NBS and using www.nhs.uk/grab-a-jab.
- Continuing to support all eligible frontline staff to obtain the necessary documentation to enable vaccination sites to validate their identity at the point of delivery. This could be a workplace photographic identity badge, a letter from the employer or a payslip dated within the last three months.
- Continuing to encourage care staff to locate their NHS number if they do not know it or do not have one.
- Continuing to work with employees to manage the logistics of any support required to access or travel to vaccination sites. This includes releasing staff to receive their vaccinations, while maintaining safety and continuity of care. Where the employer is a care home provider, it should work with staff to maximise the opportunities for workplace based vaccinations administered by roving PCN teams. In the event of COVID-19 or other infections being present, care providers should seek advice on whether any vaccination should be delayed and, if so, for how long, from the Local Authority coordinator or the hub. They in turn can take advice from the UK Health Security Agency, Office for Health Improvement and Disparities or from the local Director of Public Health.
- Maintaining a record of vaccinated staff, with staff members’ agreement, to include date/location of each vaccination. CQC registered providers should report uptake directly through the Capacity Tracker. Non CQC registered providers/employers should provide information on staff uptake to their Local Authority for input into the Capacity Tracker.
- Being responsive to changes in data collection systems.
- Ensuring co-promotion of COVID-19 boosters and flu vaccines to all frontline social care employees.
- Working in partnership with the NHS and public health leads to implement the use of evidence based resources and approaches to support the uptake of the ‘Evergreen’ offer among social care workers with protected characteristics, who are known to have low vaccine confidence. They should also continue practical support for employees, or individuals facing difficulties with vaccine confidence or in arranging vaccination, ensuring this is extended to cover booster vaccination.
3.3.4 NHS Vaccination Providers and the NBS
The NBS will continue to provide access for unvaccinated adults, including unvaccinated social care workers to directly book their COVID-19 vaccination appointments in line with the ‘Evergreen’ offer (See Appendix 5).
Each Hospital Hub, Vaccination Centre, PCN and community pharmacy within the Local Vaccination Service will be responsible for:
- Operating effective booking systems for vaccination clinics which confirm disabled access arrangements on site and the ‘on the day arrangements’ for the vaccination appointment.
- Providing details of pop-up, walk-in and mobile sites for recipients to locate using the www.nhs.uk/grab-a-jab link.
- Ensuring appropriate ID and employment checks are undertaken when individuals check in at vaccination sites (see Appendix 5). Where vaccination sites are unable to confirm suitable ID and evidence of employment during the check in process:
- at a vaccination site following a booking made through the self-referral pathway on NBS, or
- at a mobile, walk-in, or pop-up vaccination site, for a priority booster vaccination
staff at the vaccination site should inform the social care worker that proof of employment is required prior to accessing a priority booster vaccination. PAs who attend without evidence of employment should be advised that Local Authorities should provide a branded template letter of authority* for their employers to complete. A list of the local points of contact in Local Authorities which should help with this is provided by the LGA.
- Inputting data from the point of care episode into NIMS or NIVS (HHs and VCs only) and into Pinnacle (LVS only) with automated transfer into NIMS. (Pinnacle is the system for recording Point of Care records in LVS.)
- Administering the vaccination (following the required clinical process).
- Providing the recipient with a PHE record card, completed with name of vaccine, batch number and date of their first dose of vaccination. Completing date and time for second vaccination.
- Updating information on NIMS/NIVS/Pinnacle for first vaccination as appropriate.
- Recalling individuals who have received their first dose to attend for a second dose at the same location, at an appropriate time. Issuing reminders for the second vaccination appointment. In the event of a DNA to the first or second appointments, ensuring there are reminders and follow up.
- At the point of delivery for second vaccination, confirming records of first vaccination and completing the PHE record card with name of vaccine, batch number and date of second vaccination.
- At the point of delivery for a booster vaccination confirming the vaccination history to ensure the booster dose is due and that the booster being administered complies with JCVI guidance on the vaccine product for booster vaccination: subsequently completing the PHE record card with name of vaccine, batch number and date of second vaccination.
- Updating information on NIMS, NIMS via NIVS or Pinnacle for the vaccination episode.
- Where it is operationally practical, vaccination delivery sites may promote and co-administer COVID-19 boosters and flu vaccines to frontline social care workers in line with JCVI and PHE guidance. Flu vaccines are provided to social care workers as part of the NHS complementary offer, where the social care worker is unable to access an employer’s occupational flu vaccination scheme.
- PCNs and roving vaccination teams which provided vaccinations to staff in older adult care homes should extend the offer of workplace vaccinations to include all care home staff, including the ‘Evergreen’ offer and booster vaccinations.
- Work towards implementing a call and recall capability for social care workers, and subject to satisfactory technical and data developments. They should work to align this with business as usual process for other cohorts starting with those who made NBS bookings in Phase 1 and moving on to use other management information (subject to Information Governance approval). This will provide record level data to improve monitoring and reporting for booster vaccinations.
* The LGA and ADASS have produced additional guidance for Local Authorities and Personal Assistants.
3.3.5 Community-based frontline social care workers
Individual frontline social care workers are responsible for:
- Working in co-operation with their employer and Local Authority, being proactive in seeking their national offer of a booster vaccination. Where social care workers have low vaccine confidence, they should access workplace support to address concerns about the vaccine in the first instance. Accessing support and information will help them consider personal and professional responsibilities for keeping themselves, clients and colleagues safe.
- Taking action at the earliest opportunity, following receipt of the national offer for the initial course and COVID-19 booster vaccinations. They should access the initial course and booster vaccination through the following routes:
- as workplace based vaccinations if working in care homes
- through the NBS, including use of the self-referral route for booking priority booster vaccinations
- through sites which are available using the link www.nhs.uk/grab-a-jab.
- Ensuring they take action to comply with any policy changes linked to vaccination as a condition for deployment.
- Taking action to locate their NHS number if they do not know it.
- Social care staff should be aware that in line with PHE guidance, consent is obtained verbally at the point of care.
- Providing the necessary information, as requested, during the vaccination appointment, including evidence of employment with one of the following:
- a workplace photographic identity badge
- a letter from the employer dated within the last three months
- a payslip dated within the last three months.
- Where there is any change in employment between the first and second vaccination this should be discussed with the individual’s employer. This is necessary to ensure records are accurate and noted by the vaccination provider at the time of second vaccination.
3.3.6 GP practices
GP practices are responsible for:
- Supporting the roll out of COVID-19 booster vaccinations by continuing to work in conjunction with local vaccination services at GP practices in line with JCVI advice and the LVS SOP. This includes plans for co-promotion and opportunistic co-administration or concomitant administration of COVID-19 boosters and flu vaccinations in line with JCVI clinical advice.
- Ensuring that arrangements to validate the identity of eligible frontline care staff are based on proof of invitation for vaccination by the NHS call and recall service, or proof of employment as a health or social care worker to include one of the following:
- a workplace photographic identity badge
- a letter from the employer dated within the last three months
- a payslip dated within the last three months.
Annex 1- Standard Operating Procedure for Phase 1
1. Purpose
This standard operating procedure (SOP) supports deployment of vaccinations to frontline health and social care workers in priority cohort 2, as identified by the Joint Committee for Vaccination and Immunisation (JCVI).
Operational guidance to commence immediate vaccination of this cohort, ensuring maximum uptake of vaccination and timely, equitable access across staff groups, was issued on 7 December 2020 and can be found here.
This standard operating procedure (SOP) provides additional guidance on the how this will be achieved for the frontline social care workforce. It describes the process to support the identification and vaccination of frontline social care workers as part of the COVID-19 Vaccination Programme.
This SOP does not apply to frontline social care workers within the JCVI priority cohort 1 (that is those who work within CQC registered residential settings for older adults) for which a separate SOP exists here (Hospital Hubs) and as was outlined in the Phase 1 LVS Community SOP in appendix D but has now been replaced by the LVS roving and mobile SOP.
This SOP is intended to support Local Authorities, the NHS Vaccination Programme, employers* of frontline social care workers and care workers to develop an integrated approach, ensuring equitable access to and uptake of vaccination.
*The term employer includes Local Authorities in their capacity as the employer of social care workers across adult and children’s services. Within Local Authorities the DASS and ADCS provide the executive lead for these respective services and therefore it is likely that they will discharge the roles responsibilities and actions assigned to employers for their respective staff in adult and children services.
It recognises that strong local leadership and partnerships between Local Authorities, the NHS, social care providers and their representative bodies working with social care staff, will be essential to define the optimal local arrangements to maximise the take up of this national offer for vaccination. The SOP therefore sets out the framework for local delivery focusing on the definition, identification and necessary actions and data capture needed to enable eligible individuals in this priority cohort to receive the vaccine and to monitor uptake. It is a guide to the process, designed to clarify roles and responsibilities, recognising the rapid scale of deployment of vaccination arrangements across Hospital Hubs, local vaccination services and vaccination centres over the coming weeks. It is not intended to disrupt any existing local arrangements that are in place where these are working effectively and is complimentary to the clinical guidance to support the safe and effective delivery of the vaccination.
It will be updated as we learn of potential improvements from operational delivery.
2. Scope
This SOP outlines the process for facilitating COVID-19 vaccination for frontline social care workers (excluding those working in care homes for older adults) as defined by the JCVI. This includes the identification of eligible care workers and the roles and responsibilities within local systems for enabling and supporting care workers to be vaccinated.
The SOP also outlines how Hospital Hubs, Vaccination Centres and Local Vaccination Services should work to deliver COVID-19 vaccination to frontline social care workers at pace. It covers how they should work in partnership to match vaccination capacity to meet demand, support booking, on the day arrangements and data capture to monitor uptake. It does not cover the clinical delivery of the vaccine, which is covered in separate guidance.
2.1 Frontline social care workers within the scope of this SOP
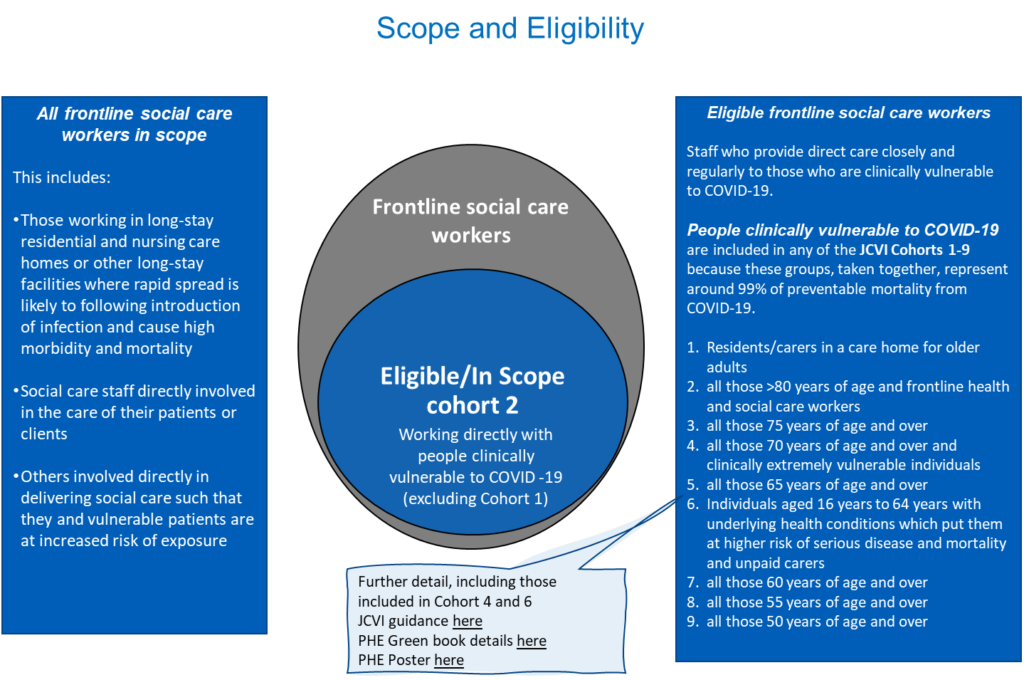
The priority 2 cohort includes:
All frontline social care workers directly working with people clinically vulnerable to COVID-19 who need care and support irrespective of where they work (for example in people’s own homes, day centres, care homes for working age adults or supported housing); whether they care for clinically vulnerable adults or children*; or who they are employed by (for example local government, NHS, private sector, Personal Assistants or third sector employees).
*The JCVI has identified children most at risk of COVID-19 as those of any age who are clinically extremely vulnerable or who are aged 16 and over who are at greater risk of disease or mortality because of underlying health conditions. The committee also advised that only those children at very high risk of exposure and serious outcomes, such as older children with severe neuro-disabilities that require residential care, should be offered vaccination with either the Pfizer-BioNTech or the AstraZeneca vaccine.
The government Green Book for immunisation against infectious disease provides further detail in support of the JCVI priority groups to support vaccination programmes and defines frontline social workers to include:
- Those working in long-stay residential and nursing care homes or other long-stay facilities where rapid spread is likely to following introduction of infection and cause high morbidity and mortality
- Social care staff directly involved in the care of their patients or clients
- Others involved directly in delivering social care such that they and vulnerable patients are at increased risk of exposure
The Green Book goes on to stipulate that young people aged 16-18, who are employed in, studying or in training for health and social care work should be offered the vaccination alongside their colleagues if a suitable vaccination is available.
Figure 1 below recognises that those in scope will be a subset of frontline social care work roles as defined by Skills for Care*, specifically those who are directly working with people clinically vulnerable to COVID-19. (It is recognised that local employers may further define job roles and titles with which the social care workforce will more readily identify, and therefore local processes to identify the frontline social care workforce should take this into account.)
* Skills for Care is part of the Skills for Care and Development (SfC&D). This is the sector skills council for people working in social work and social care for adults in the UK.
Figure 1:
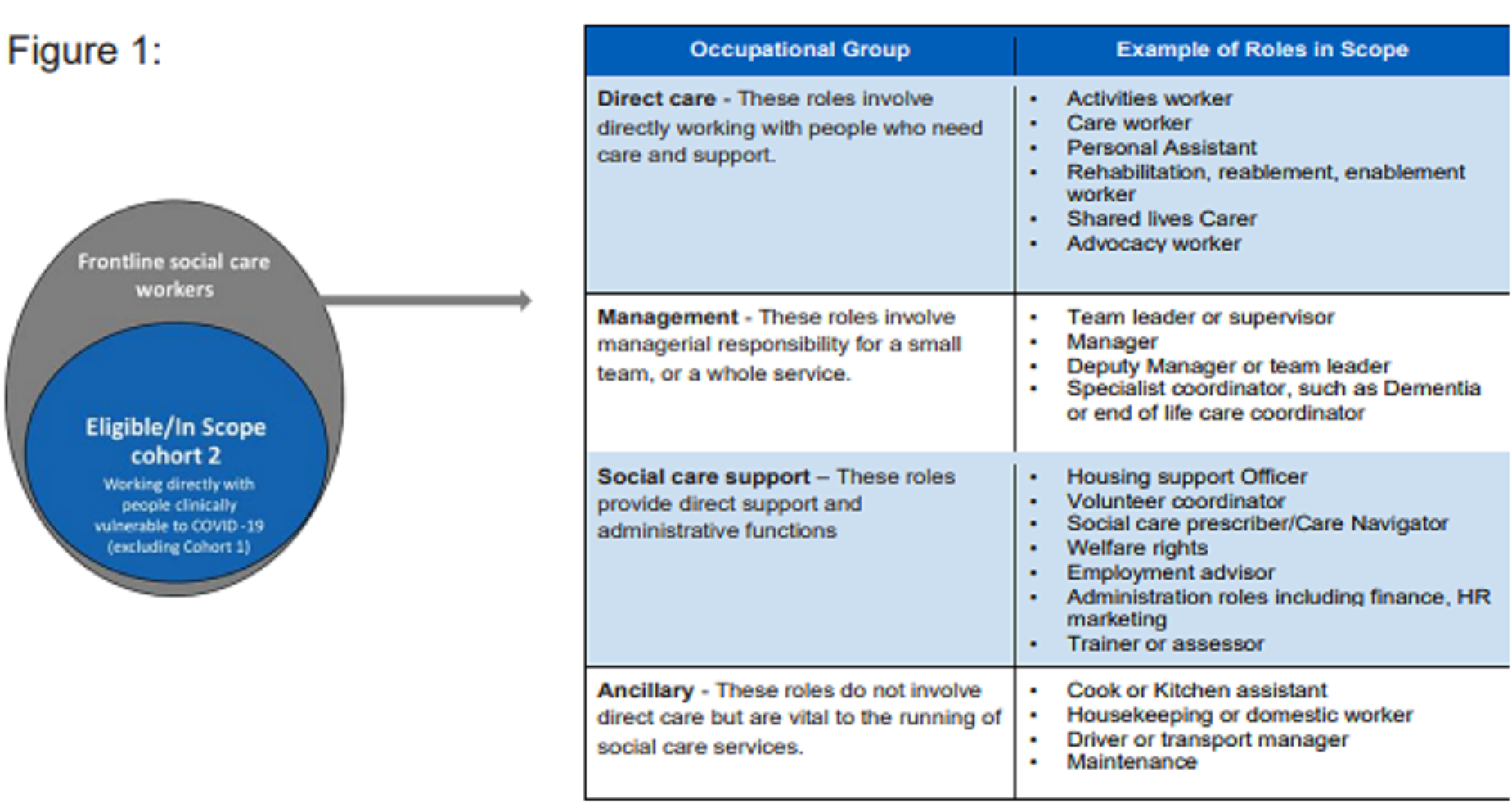
The Local Authority Director of Adult Social Services will have ultimate responsibility for identifying eligible SCW where needed, underlined by the principle aim of achieving high rates of vaccination amongst frontline social care workers who provide care closely and regularly with those who are clinically vulnerable to COVID-19. This will require a consistent interpretation of which social care workers provide care closely and regularly to those who are clinically vulnerable to COVID-19. Those clinical vulnerable to COVID-19 are defined by the JCVI priority groups: a) the Clinically extremely vulnerable (CEV), b) those who have underlying health conditions leading to greater risk of disease or mortality as defined in the Green book, c) those of advanced age. They should ensure that identification of eligibility is consistently applied across the system. Appendix 1 provides more detail on eligibility and offers a framework for use locally.
The Local Authority and NHS vaccination services will work in partnership to reach all eligible frontline social care workers irrespective of the sector in which they work. For example, the approach should include directly employed Personal Assistants, who support people within any of the JCVI priority groups (the clinically vulnerable to COVID-19 children and adults) as they are considered to be eligible within the priority 2 cohort, as are those supporting people in receipt of continuing health care in their own homes.*
*The LGA and ADASS have produced additional guidance for Local Authorities and Personal Assistants.
Other roles and services where individuals are providing frontline social care support may be considered eligible within this cohort. These roles may include services provided by organisations commissioned by local government and/or the NHS, for example, Homeless services and support; Response services to Technology Enabled Care (Telecare); and Housing with support.
The following are, however, not eligible within this priority group as defined by the JCVI:
- Administrative staff who do not have any direct contact with clients.
- Social care workers working with children who are not considered priority within the context of the JCVI priority cohorts 1-9 (children under 16 who do not have underlying health conditions leading to greater risk of disease or mortality and children who have no underlying health conditions).
- Unpaid carers
Separate work is ongoing to identify all unpaid carers so that they can be vaccinated at the appropriate time according to JCVI priorities. We recognise however that a high proportion of unpaid carers are aged 50+ and already fall within one of the nine JCVI cohort groups. Those aged below 50 and caring for vulnerable people fall into cohort 6. Further guidance will be published on this cohort in due course.
3. Roles & Responsibilities
3.1 Overview of Process
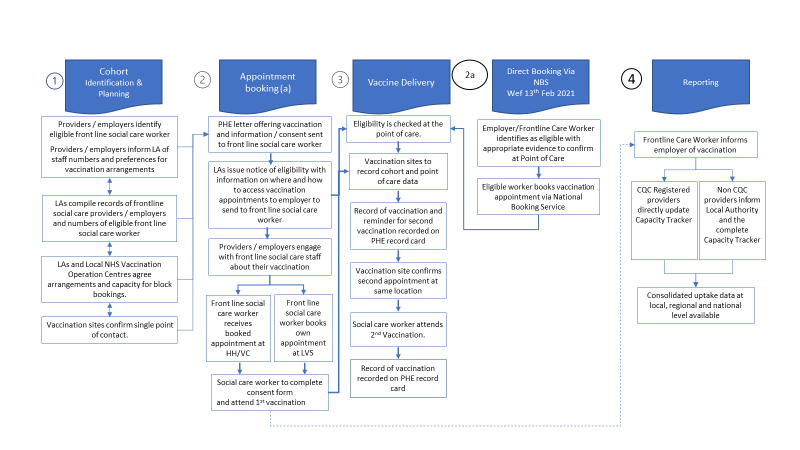
To maximise the effective delivery of the vaccination programme for frontline social care workers, strong partnership working between providers and employers, Local Authorities and the NHS will be required.
Effective engagement between social care provider organisations, not all of which will have a direct relationship with the Care Quality Commission, Local Authority, NHS or Local Resilience Forums, will also be necessary. This includes organisations which supply social care services to individuals who pay for their own care.
A high-level summary of the end-to-end process is illustrated below in figure 2 and specific roles, responsibilities and actions required are described in sections 3.2 and 3.4.
Figure 2 Phase 1 rollout to Social Care Workers
3.2 Roles and Responsibilities
The following table sets out the key roles and responsibilities of partners, within local systems, to maximise uptake of vaccinations for this priority group. It is supported by section 3.4 which details the actions required.
| Body | Key Roles and Responsibilities |
|---|---|
| Local Authorities* |
Local authorities have a key role working with the local NHS Vaccination Programme to support local planning to maximise access to and uptake of vaccination. Local Authorities should, ensure strong input from provider representatives so that processes put in place for eligible staff to be identified, invited and vaccinated use the most appropriate approach for the SCW cohort, their clients and employers.Local authorities, working with the CQC and local resilience forum partners, are responsible for ensuring that all employers of frontline social care workers in their area are identified and provided with the necessary information and support to make arrangements for the vaccination of staff. This may require discussion with providers/employers who employ frontline social care workers in different Local Authority /STP areas to agree arrangements for local access. This should enable an overview of the number of eligible frontline staff in each Local Authority area to be determined (not at individual level).
Local Authorities will also ensure, in partnership with the NHS local vaccination leads, that practical support is available to all employers of care workers, or individuals facing difficulties in arranging vaccination. This could include assistance with logistics, transport, or costs. Local Authority leads will also be responsible for providing consolidated information on uptake via the national capacity tracker for all non CQC registered providers (including their own directly employed care workers) using best endeavours and based on information provided by employers. |
| Local NHS Vaccination Programme** | The local NHS vaccination programme lead should establish arrangements to engage actively with Local Authority leads and provider organisations to ensure equitable access to vaccination for frontline care staff across the Local Authority area. They should work with the national delivery model leads and local vaccination delivery sites to ensure optimum coverage and capacity for delivery based on the total number of eligible social care workers identified. They should ensure that there are clear plans in place to maximise access for this priority group at pace. Local NHS vaccination programme leads should ensure local options to access vaccinations are made available to the relevant Local Authority (or authorities) for distribution to eligible frontline care workers, so they are clear about how they access vaccination appointments. |
| Employers of eligible frontline social care workers (including Local Authorities and NHS) |
CQC-registered providers, and other non-registered organisations who employ frontline care workers providing care to clinically vulnerable to COVID-19 individuals (as defined by JCVI) should proactively approach Local Authorities to ensure that eligible staff are identified and able to be included.
All employers of front-line social care workers should put in place internal arrangements to facilitate eligible employees to access vaccinations at pace taking into consideration equality of access and health inequalities. All employers should provide relevant information to the Local Authority and system partners to enable logistical and operational planning for the vaccination of eligible staff as necessary and in line with this SOP. Employers should facilitate and actively support access to vaccination, recognising the benefits to the safety of staff and clients. This should include consideration of logistics of releasing staff while maintaining safe delivery of services. CQC registered providers should report uptake directly through the Capacity Tracker. Non CQC registered providers/employers should provide information on staff uptake to their Local Authority for input into the Capacity Tracker. |
| NHS Vaccination Service Providers (Hospital Hubs, Vaccination Centres, Local Vaccination Services) | Hospital Hubs, Local Vaccination Services Vaccination Centres will work with the local vaccination operations centre (VOC), and national delivery model leads where necessary to agree optimal arrangements to maximise access and uptake of vaccinations for frontline social care workers.
Vaccination operation centres will ensure that arrangements to validate the identity of eligible frontline staff are agreed across the local system and ensure they are clearly communicated to eligible individuals as part of the information about how to access vaccinations. Vaccination delivery sites will ensure they utilise systems and processes set out in this SOP and other relevant operational frameworks including any operational frameworks which may be developed i.e., covering the data capture. For this cohort, for example, the delivery sites should use the approved PHE publications to support the consent process for social care workers. Vaccination delivery sites are clinically responsible for the administration of vaccinations in accordance with relevant guidance and operational frameworks. |
| Frontline Care Workers | Frontline care workers should be aware of their right to access vaccination as a priority group. They should receive the national offer for vaccination, consent form, relevant vaccination leaflets and local information about how to access vaccinations. They should have access to the Public Health England clinical information leaflets about COVID-19 including the information for women of childbearing age. They should consider their personal and professional responsibility to maximise their own, their client’s, and any co-worker or family members health and safety.
They should actively participate in the arrangements to access a vaccination as agreed with their employer where appropriate. They should act in a way to safeguard resources by ensuring they attend booked appointments and ensure they have the necessary documentation to enable vaccination sites to validate their identity at the point of delivery. Additionally, workers should make efforts to access a Flu vaccination, being sure to follow the correct guidance and timelines between Flu and COVID-19 vaccination. |
*All Local Authorities have been required to identify a lead officer to work with the NHS to support the delivery of the COVID-19 Vaccination Programme.
**There is an NHS Vaccination Programme Lead for each NHS Strategic Transformation Partnership (STP) or Integrated Care System (STM), with an identified Senior Responsible Officer.
3.3 Local Arrangements to maximise access and uptake
In line with the Equality Act 2010 all organisations and employers within the local health and social care system should ensure the local approach to reach eligible individuals in cohort 2 considers equality of access and health inequalities. They should take steps to ensure equitable access to vaccinations for the eligible social care workforce employed within the Local Authority area including reasonable adjustments to allow for equitable access by individuals with protected characteristics.
All employers should ensure that internal arrangements to identify eligible frontline workers take into account the JCVI recommendations that within this cohort, employers should prioritise frontline staff:
- At high risk of acquiring infection
- At high individual risk of developing serious disease, or
- At risk of transmitting infection to multiple vulnerable persons or other staff.
The guidance on the individual risk management process within the COVID-19: adult social care risk reduction framework can support employers identify priority staff within cohort 2.
During January there will be a rapid expansion of Hospital Hubs and Vaccination Centres. Hospital Hubs are well placed to provide block bookings for health and social care workers in cohort 2 and the network across the county will provide the primary route for frontline social care workers to access vaccinations at pace through block bookings. Acute, Mental Health and Community NHS Trusts will be able to provide Hospital Hubs increasingly in multiple locations. Local access is likely to be an important issue for many social care staff, in particular, those working in more rural areas. Employers should identify where accessibility to block bookings at Hospital Hubs and/or Vaccination Centres is a barrier to rapid access or achieving high uptake. Local Authorities should work in partnership with the local vaccination SRO and the national delivery models to understand changes in coverage as more vaccination sites become operational
Eligible social care staff can self-book with local vaccination services. Where local vaccination services are the preferred route for vaccination, the frontline care worker should be signposted by their GP practice to the PCN site working with their registered GP.
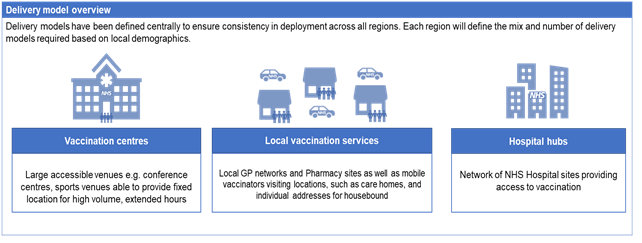
Delivery model overview
3.4 Actions Required
3.4.1 Actions for Local Authorities
Local Authorities are responsible for:
- Identifying who will co-ordinate the local system response on behalf of the Local Authority Director of Adult Social Services.
- Working with the CQC and local NHS partners to identify providers of social care services and subsequently the eligible frontline care workers they employ. This will include both CQC and non-CQC registered providers of commissioned services as well as providers which may be supporting self-funders and individuals in receipt of personal budgets and direct payments.
- Developing and actively maintaining an overview of the total numbers of eligible frontline social care workers within their area, by employer (see Appendix 3 for example template). This overview should include the number of social care workers who, in line with JCVI guidance, are being prioritised within cohort 2.
- Having mechanisms in place to make this overview available to their local NHS Vaccination Operations Centre and system partners to support planning and delivery arrangements.
- Working with the Vaccination Operations Centre and local system vaccination SRO to understand the capacity for block bookings available to social care to meet demand from the local social care system and achieve the national aim for all eligible health and social care staff to be offered vaccinations by mid February 2021.
- Working with employers and the Vaccination Operations Centre to agree how employers can confirm arrangements for employees to attend block bookings with delivery sites.
- Ensuring that all eligible frontline staff employed within the Local Authority area receive the:
- national offer for vaccination (see Appendix 1a Covering letter for consent form: Frontline Social Care Staff)
- PHE consent form (see Appendix 1b COVID-19 vaccination consent form for frontline social care workers)
- Local Authority notice of eligibility and information on where and how to access vaccination services within the local system (see Appendix 2).
- Ensuring that communications and information are issued directly to internal employees, or via local providers and employers to eligible frontline social care workers within the scope of this SOP.
- Working with the NHS Local Vaccination SRO and providers / employers from across the Local Authority area to ensure that robust processes are in place to identify, invite and vaccinate all eligible frontline social care workers in a way which is appropriate for this cohort, their clients, employers and addresses equality of access and health inequalities.
- Completing the Capacity Tracker for all non CQC registered providers in line with agreed national reporting requirements.
- Ensuring local employers are responsive to changes in data collection systems.
3.4.2 Actions for Local NHS Vaccination Programme Leads
The Senior Responsible Officer for the local Vaccination Programme is responsible for:
- Working with Local Authority vaccination lead and national delivery model leads to optimise plans for coverage and to develop a local capacity and delivery plan to maximise access to and uptake of vaccinations by frontline social care workers.
- Ensuring that Hospital Hubs, Vaccination Centres and Local Vaccination Services are prepared to vaccinate this cohort. This includes agreeing arrangements for employers and employees to access to block bookings taking into account capacity to meet the required demand and the working patterns of front-line social care workers.
- Working with the Local Authority and employers to agree how employers can confirm arrangements for employees to attend block bookings with delivery sites.
- Ensuring that arrangements to validate the identity of eligible frontline care staff at vaccination sites is agreed and clearly communicated within the local system and followed at the point of care delivery to safeguard against unauthorised use.
- Ensuring all eligible frontline staff obtain physical copies of the social care worker consent form and that they complete all the fields requested on the form.
- Ensuring that robust administrative and data collection systems are in place using NIMs/NIVs or Pinnacle as appropriate to support the effective delivery of the programme and any local, regional or national monitoring requirements. This includes as a minimum, point of care data collection for the clinical event of vaccination and recording information from the consent form to support regional and national oversight in monitoring vaccine uptake by this cohort.
- Ensuring vaccination delivery sites are responsive to changes in data collection systems.
3.4.3 Actions for providers/employers of community-based social care workers
Providers / employers (which may include the Local Authority and NHS organisations) employing eligible frontline social care workers are responsible for:
- Ensuring all relevant employees receive the national offer for vaccination, consent form, vaccine information leaflets and local notice of eligibility with information about how to access vaccinations.
- Providing relevant information to the named Local Authority lead and the national vaccination service as necessary, to support delivery and monitoring in line with this SOP.
- Identifying the total number of eligible frontline social care workers employed and confirming key factors relevant to support their access to vaccination to their Local Authority lead, For example:
- the number of care staff who are at high risk of acquiring infection and developing serious disease or transmitting infection to multiple vulnerable persons or other staff; and or
- the number of care staff who can attend block bookings.
- Understanding where providers/employers have staff working in different Local Authority areas and confirming preferred planning and delivery assumptions to the relevant Local Authority leads to support the planning and delivery of vaccination for local staff.
- Issuing and ensuring all relevant employees receive the national offer for vaccination, which includes the Public Health England clinical information leaflets about COVID-19, including the information for women of childbearing age, the consent form and the Local Authority notice of eligibility with information on how to access vaccinations. Employers should issue these via channels and in formats to enable staff to be aware of and be vaccinated as quickly as possible, whilst safeguarding against unintended use. Employers should support those staff who may need this information in alternative formats. Employers should support all eligible frontline staff to obtain physical copies of the consent form and notice of eligibility so that they can ensure they have the necessary documentation to enable vaccination sites to validate their identity at the point of delivery and complete the consent process efficiently. Employers should encourage care staff to provide the information requested on the consent form prior to attending for their vaccination. They should encourage care staff to locate their NHS number and utilise the link on the covering letter for consent if they do not know or have an NHS number. They should make staff aware that the consent form can only be signed at the point of care.
- Working with vaccination operations centres, delivery sites and employees to make arrangements for block booked vaccination appointments and where appropriate, adjusting working patterns as necessary to support.
- Considering and managing the logistics of releasing staff to receive their vaccine, while maintaining safety and continuity of care.
- Considering how to maximise the uptake of vaccinations through conversations with care staff, using nationally available staff and public communications materials. Conversations should also consider any employer support to access the vaccination site and include confirmation that travel will be socially distanced as necessary.
- Maintaining a record of vaccinated staff, with staff members’ agreement, to include date/location of each vaccination, and for those providers required to update the national Capacity Tracker to include any relevant information as required. They should review records of vaccinated staff at regular intervals and work in partnership with the Local Authority to report on progress and provide reminders and local encouragement to support the national aim for all eligible health and social care staff to be offered vaccinations by mid February 2021.
- Ensuring they are responsive to changes in data collection systems.
- In the event of COVID-19 or other infections being present, care providers should seek advice about whether any vaccination should be delayed, and if so for how long, from the Local Authority coordinator or the hub. They in turn can take advice from Public Health England or the local Director of Public Health
3.4.4 Actions for NHS Vaccination Providers including the National Booking Service
From 11 February 2021, the National Booking Service provides access for eligible frontline social care workers to directly book their vaccination appointment (see Appendix 5).
Each Hospital Hub, Vaccination Centre and each PCN and community pharmacy within the Local Vaccination Service will be responsible for:
- Confirming the point of contact for frontline social care worker vaccinations and working with the Local Authority and NHS Local Vaccination SRO.
- Operating effective booking system for vaccination clinics.
- Providing details of how to book appointments; ensuring that this is set out in relevant information provided to employers and frontline care workers.
- Inputting data from booking system into NIMS or NIVS (HHs and VCs only) and into Pinnacle14 (LVS only) with automated transfer into MIMS.
- Confirming ‘on the day arrangements’ for the vaccination appointment such as:
- First appointment date, time and location
- Requirements to validate the identity of eligible frontline staff.
- Ensuring appropriate ID checks at point of care, with particular reference to those individuals who have booked their appointment via the National Booking System (See Appendix 5).
- Administering the vaccination (following the required clinical process).
- Providing the recipient with a PHE record card, completed with name of vaccine, batch number and date of their first dose of vaccination. Completing date and time for second vaccination.
- Updating information on NIMS/NIVS/Pinnacle for first vaccination as appropriate.
- Recalling individuals who have received their 1st dose of vaccine to attend for their second dose at the same location. At an appropriate time, issuing reminders for the second vaccination appointment. In the event of a DNA to the first or second appointments, ensuring there are reminders and follow up.
- At the point of delivery for second vaccination, confirming records of first vaccination and completing the PHE record card with name of vaccine, batch number and date of second vaccination.
- Updating information on NIMS or NIMS via NIVS or Pinnacle for second vaccination.
3.4.5 Actions for community-based frontline social care workers
Individual frontline social care workers are responsible for:
- Working in cooperation with their employer and Local Authority and being proactive in seeking their national offer for vaccination, consent form, clinical information leaflets and notice of eligibility with information about how to access vaccinations locally.
- Taking action at the earliest opportunity, following receipt of national offer for vaccination and consent form, to access the patient information leaflets and consider personal and professional responsibilities for keeping themselves, clients and colleagues safe.
- Taking action on receipt of notice of eligibility and information about how to access vaccinations locally to access vaccination services at the earliest opportunity. If necessary, in discussion with their employer, to consider the preferred location for receipt of the vaccination.
- Working with the employer to book vaccination appointments in line with block booking arrangements.
- Taking action to book their own vaccination appointment with local vaccination services at a community pharmacy as these become available locally or at the PCN site working with their GP.
- Taking action to identify their NHS number or register for an NHS number prior to vaccination. They should utilise the link on the covering letter for consent if they cannot locate or do not have an NHS number.
- Employers should encourage care staff to provide the information requested on the consent form prior to attending for their vaccination. They should encourage care staff to take steps to confirm their NHS number by looking at the advice on the NHS website or by following the link on the covering letter for consent.
- Social care staff should be aware that the consent form can only be signed at the point of care.
- Providing the necessary information, as requested during the vaccination appointment. This includes providing necessary photographic ID and evidence of employment, the information as requested on the consent form (see Appendix 1b) to assist in the safe delivery and overall monitoring of the National Vaccination Programme. Your NHS number should be recorded in any COVID-19 tests undertaken. Where an individual is unable to provide their NHS number, their name, date of birth, home address and the name and address of the GP and practice where they are registered must be completed on the consent form enable their NHS number to be confirmed.
Where there is any change in employment between the first and second vaccination this should be discussed with the individual’s employer as necessary to ensure records are accurate and noted by the vaccination provider at the time of second vaccination.
Appendix 1 – Framework for Eligibility
The following seeks to provide a simple framework to consider eligibility with some examples offered. Local Authority Directors of Adult Social Care have ultimate responsibility for confirming eligibility across staff groups within the local authority area. The LA DASS should work with Directors of Children’s Services to confirm eligibility within the children’s workforce.
The table below offers advice to support the Local Authority Directors of Adult Social Care for making decisions on eligibility, noting that any decision should be based on there being clear evidence that the frontline social care workers are providing direct care closely and regularly to those who are clinically vulnerable to COVID-19
| Frontline care worker | Works with which person/s clinically vulnerable to COVID-19 | Default Cohort 2 | Comment | |
|---|---|---|---|---|
| Supported housing, extra care and supporting living workers, including on site ancillary* | Yes | Yes: People of senior age; underlying health conditions; learning disabilities | Yes | Review services to other groups on individual basis |
| Homeless services including rough sleepers / shelter and street support teams and active volunteers | Yes | Possible: People with CEV; underlying health conditions | No | Review services to other groups on individual basis |
| Office workers with no face to face client contact | No | No | No | |
| Children and Family Social Workers | Yes | Possible: Children <16 with CEV; underlying health conditions | No | LA may review on individual service basis |
| Personal Assistants/Live in Carers | Yes | Yes: People of senior age; underlying health conditions (learning disabilities) | Yes | LA may review PAs for <16s on an individual basis |
| Women’s Refuge workers, including volunteers on site ancillary staff* | Yes | Possible: People with CEV; underlying health conditions | No | LA may review on individual service basis |
| Telecare response services/ reablement / discharge support services | Yes | Yes: People of senior age; CEV; underlying health conditions; | Yes | |
| Hospices, including on site ancillary staff | Yes | Yes: People of senior age; people with CEV; underlying health conditions | Yes | Likely to be within health cohort |
On site ancillary includes staff who may have social contact with patients but are not directly involved in patient care. This group includes receptionists, ward clerks, porters and cleaners
Appendix 2a– National Offer Letter
14th January 2021
Covering letter for consent form for social care staff
Dear Frontline care worker
COVID-19 Vaccination Frontline Social Care workers all sectors: Social Care, Health, Third and Voluntary Sectors
I would like to inform you that we will soon be making COVID-19 vaccinations available to all front-line social care workers and would like to ask if you wish to give your consent to be vaccinated.
This vaccination will be free of charge and our highest priority is delivering the vaccines to all eligible staff as quickly as possible.
Through vaccination of our front-line social care workforce, we aim to help protect individuals from becoming unwell with, or dying from, COVID-19 disease. It will also help reduce the risk of staff spreading infection to vulnerable clients, patients and family members.
Please read the guide for social care staff which we have sent with this letter or read it online here:
https://www.gov.uk/government/publications/covid-19-vaccination-a-guide-for-social-care-staff
More information about COVID-19 vaccines is available from:
www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine
https://www.gov.uk/government/collections/covid-19-vaccination-programme
For women of childbearing age, please read the detailed guidance at: https://www.gov.uk/government/publications/covid-19-vaccination-women-of-childbearing-age-currently-pregnant-planning-a-pregnancy-or-breastfeeding
Indications are that some vaccine recipients may experience a painful heavy arm where they had the injection and may feel tired or have a mild fever for a couple of days. These are common side effects following vaccination. If required paracetamol may help to reduce these effects and keep you as comfortable as possible following vaccination. Please read the product information for more details on the vaccine and possible side effects by searching Coronavirus Yellow Card. You can also report suspected side effects on the same website or by downloading the Yellow Card app.
During the vaccination delivery we will maintain the range of measures we have in place to keep our staff safe from COVID-19. Staff giving the vaccine will be wearing personal protective equipment and will abide by all our cleaning and disinfection requirements. Please note two doses of the vaccine are required 3-12 weeks apart.
To progress vaccinations as quickly as possible, your employer and/or the local authority will work to determine the right location for you to receive your vaccination.
The NHS is rapidly expanding the number of sites across the country where vaccinations can be given. This includes hospital hubs where block bookings can allow large numbers of frontline social care workers to rapidly access vaccinations. It also includes local vaccinations services at GP practices and community pharmacies; with more service due to open as the rollout of the programme progresses.
What happens next?
Your employer is providing a notice of eligibility from the Local Authority and local NHS Vaccination Programme, which is proof of your eligibility for vaccination, in line with the Joint Committee on Vaccination and Immunisations (JCVI) priorities for frontline social care workers.
You need your notice of eligibility for vaccination from the Local Authority which your employer will provide. You must take a physical copy of your notice of eligibility to show at the vaccination appointment.
When you attend for your vaccination, you will need your work identity badge or another form of photo ID.
When you attend for your vaccination, you may be able to give verbal consent. Some vaccination service providers are requiring written consent before you attend the vaccination session.
If your employer or the vaccination service provider has issued you a consent form please take it to your appointment, you may be asked to complete it there.
Where your employer is arranging block bookings for vaccinations you can be part of this process. Alternatively, you can take steps to book your own appointment with local vaccination services through the GP/ practice where you are registered or soon at community pharmacies. The local authority and your employer are providing information on local vaccination sites and how you can access them.
If you need help or have concerns about accessing a vaccination appointment you should speak to your employer in the first instance. There are no walk-in vaccination appointments being offered. You must have a booked appointment for vaccination arranged by your employer, or directly by yourself. Please confirm your intention to attend for vaccination with your employer immediately.
By consenting you will be playing your part by protecting yourself and helping to protect patients, clients and staff from catching and spreading COVID-19.
Best wishes
Mary Ramsay | Consultant Epidemiologist and Head of Immunisation, Public Health England
Dr Jonathan Leach OBE | NHS England Medical Director for COVID-19 Immunisation | NHS England Associate Medical Director for Armed Forces and Veterans Health | Joint Honorary Secretary Royal College of General Practitioners | General Practitioner Davenal House Surgery Bromsgrove
Appendix 2b: Consent Form
Appendix 3: Local Authority Notice of Eligibility
This template notice of eligibility requires the letter head for the relevant LA and
should be signed by the Director of Adult social services.
Dear Sir/Madam,
The Joint Committee on Vaccinations and Immunisation (JCVI) identified frontline social care workers as a priority for vaccination due to the critically important work you are doing within your community. You are in receipt of this letter as you have been identified as a frontline social care worker.
Your employer should have sent you a national letter informing you that the vaccination programme is making COVID-19 vaccinations available to all eligible front-line social care workers and asking you to give your consent to be vaccinated. The letter was accompanied by a consent form and had important links to information about the vaccination, such as advice for women of childbearing age. If you have not received this information you should speak to your employer immediately.
The Local Authority and local NHS vaccination programme have been working to identify where you can access vaccination services in your area. The number of sites across the county are continuingly growing and we are working to determine the right location for you to access your vaccination as quickly as possible given the national aim to complete vaccinations for health and social care workers by mid February 2021.
It is now important that you confirm your intention to attend for vaccination with your employer if you have not already done so. You employer will confirm where they will access block booked appointments at the local hospital hub or a suitable alternative site offering block booked appointments. As an appointment is reserved / booked for you, your employer will confirm the time and date along with information relating to any ‘on the day’ arrangements at the vaccination site. You should make arrangements to ensure you can attend. All appointments must be pre booked.
You should take this notice of eligibility letter and your work identification badge to the appointment. Staff at the vaccination centre must see physical copies of these to confirm your priority eligibility. You must also be able to provide your NHS number on the consent form. Advice on how to find your NHS number is available here.
NHS England » How can I find out my NHS Number?
If you have not had a vaccination appointment reserved or booked for you, or you wish to book your own appointment using the National Booking Service. You will be given a booked appointment so please ensure you can attend. You must take this notice of eligibility letter, or letter from your employer, and your work identification badge to the appointment. Staff at the vaccination centre must see physical copies of these to confirm your priority eligibility. You must also be able to provide your NHS number. A link to advice on how to find your NHS number is included above.
Community pharmacies and vaccination centres are also being set up to provide vaccination services. These services will need to check your priority eligibility using the same process described above. You can access these by following the process attached.
Thank you for consenting to have the vaccination. By consenting you will be playing your part by protecting yourself and helping to protect patients, clients and staff from catching and spreading COVID-19.
Thank you for playing this vital role.
Yours sincerely,
Director for Adult Social Services
Local Authority/Local NHS Vaccination Programme to add local details for booking appointments via the National Booking Service
Appendix 4: Example of Local Authority Template with minimum data requirement
Example of Local Authority/NHS Vaccination Programme planning template.
| Provider/Employer | CQC Registered (Y/N) | Named contact | Overall number of eligible staff | Number of staff who are high risk* | Vaccination offer, consent & information leaflets distributed | Local notice of eligibility and access to services agreed and distributed | Preferred location/s | Booking arrangements/Support Agreed |
| Xxx Local Authority | J Smith j.smith@xxx.gov.uk |
450 | 1/1/2021 | XXX Hospital Hub
XXX Local Vaccination Service |
Making block booking for groups of 25 staff | |||
| XX Home Care Ltd
|
Jo Smith jo.smith@xxhomecare.com |
26 | 3/1/2021 | XXX Hospital hub | Making block booking for groups of 4 staff. | |||
| Xx day centre | John Smith John.smith@xxs.co.uk |
12 | Local Vaccination Service (x PCN) | Supporting staff to make appointments |
*Based on JCVI advice high risk means i) high risk of acquiring infection ii) high individual risk of developing serious disease or iii) risk of transmitting infection to multiple vulnerable persons or other staff.
Appendix 5: Process for those booking via National Booking Service
Eligibility checklist for health and social care workers that have self-declared for vaccination through the national booking system
Healthcare workers and community based social care workers in priority group 2 can book their vaccination appointments through the NHS COVID-19 Vaccination Booking Service (online at www.nhs.uk or by ringing 119). To book, they need to self-declare they are a health or social care worker.
When the individual arrives for their appointment
They should verbally declare to the person at the vaccination site that is booking them in that:
- they are a health or social care worker
- the type of role/work they do
- the name of their employer.<m/ark>
They should also show further proof of employment as a health or social care worker to include workplace photo ID (or alternative photo ID) and one of the following:
- A recent letter from their employer (within the last three months)
- A notice of eligibility from a Local Authority
- A recent (last 3 months) payslip which shows their employer.
The individual should be informed, by the person recoding their vaccination, that it will be recorded that they are a health or social care worker.
Who are eligible frontline social care or health care workers?
People that have direct contact with patients, clients or service users at higher risk from coronavirus (COVID-19).
Eligible health workers, for example:
- you work in a clinical role (such as a doctor or nurse)
- you have contact in a non-clinical role (such as a receptionist or porter)
- you work in a hospital laboratory, mortuary or a funeral home
Eligible social care workers
Those providing face-to-face care or support to children or adults at higher risk from COVID-19 (clinically vulnerable or clinically extremely vulnerable).
For example:
- you are employed to provide personal care or work in any support roles (cook, housekeeping, cleaning, maintenance) including as a volunteer, in a residential care home
- you are a registered professional in social care (such as a social worker, therapist or nurse)
- you work providing care for people in their homes or in community services such as home care, supported living, shared lives, extra care and day care services, or you are employed as a personal assistant.
Please speak to your employer, if you’re not sure. If you are a Personal Assistant and you need help or a proof of employment letter you can speak to your Local Authority point of contact who can help you.
Those not currently eligible include those:
- Social care workers working with children who are not at high risk from COVID-19, for example in early years education as a childminder or nursery nurse or with vulnerable children (SEND or Looked After Children) who are not clinically vulnerable to COVID-19.
- Administrative staff who do not have any direct contact with clients and who work in settings other than care homes.
If anyone books an appointment and does not bring official proof that they are eligible they will not be vaccinated when they attend their appointment.