Good HOOF guide for primary care and out of hours teams – November 2020
Contents
- Introduction
- BTS guideline for patient criteria and assessment
- APPENDIX 3: Assessment protocol for palliative oxygen page i35
- Filling in the HOOF Sections
- Filling in the Part A HOOF
- Oxygen removal
Good HOOF (Part A) guide for Primary Care and Out of Hours teams Nov 2020 Update
This guide will support non-specialist teams who need to order home oxygen for palliative and cluster headache patients (normally following a consultant recommendation and not already under the care of a Home Oxygen Assessment and Review [HOS-AR] team). All other oxygen requirement should be referred to a specialist HOS-AR team. To ensure the patient fulfils the criteria for long term or ambulatory oxygen therapy – LTOT/AOT.
Produced on behalf of the National Home Oxygen Safety Group.
4/11/2020
Introduction
This guide will support those who need to order home oxygen for palliative and cluster headache patients (normally following a consultant recommendation and not already under the care of a Home Oxygen Assessment and Review [HOS-AR] team).
NB All other oxygen requirement should be referred to a specialist HOS-AR team to ensure the patient fulfils the criteria for long term or ambulatory oxygen therapy – LTOT/ AOT.
On average, a GP will fill in a HOOF once every 5 years, so this guide is to help ensure it is completed correctly first time.
If your patient is palliative, please review the guidance from the BTS before requesting oxygen or refer to local palliative care guidance where available.
Good HOOF guide for Primary Care and Out of Hours teams – April 2020
BTS Guideline for Home Oxygen Use in Adults
https://www.brit-thoracic.org.uk/quality-improvement/guidelines/home-oxygen/
“The term ‘palliative oxygen therapy’ (POT) refers to the use of oxygen to relieve the sensation of refractory persistent breathlessness in advanced disease or life-limiting illness irrespective of underlying pathology where all reversible causes have been or are being treated optimally.”
Studies show little benefit of oxygen therapy compared with air in either hypoxaemic or non-hypoxaemic palliative patients. This guidance therefore is for patients with:
cancer or end stage cardio-respiratory disease, on maximum treatment for underlying diseases where possible, and reversible causes for breathlessness have been or are being treated optimally, who are still experiencing intractable breathlessness, and who are either
- Hypoxaemic – resting SpO2<92% or
- Normoxaemic – but only for whom ALL other approaches have been exhausted
Before consideration of oxygen therapy:
- Ensure psycho-social factors have been assessed and addressed as distress from breathlessness can be multi-dimensional
- Trial non-pharmacological measures, including breathing relaxation and life modifying strategies, by involving physio and occupational therapists
- Trial a hand-held fan
- Assess response to Opioids (significantly better than POT in reducing the intensity of dyspnoea in non-hypoxaemic or hypoxaemic patients. Evidence level 1)
- Check SpO2 using pulse oximetry at rest and/ or after exertion.
APPENDIX 3: ASSESSMENT PROTOCOL FOR PALLIATIVE OXYGEN page i35
There is no consensus for the correct clinical assessment strategy for the use of oxygen in palliative care, although multiple tools exist for assessing dyspnoea. This assessment applies to:
The subjective severity and intensity of breathlessness should be recorded regularly to evaluate the degree of suffering caused and the effect of treatment. Recurrent assessment is prudent, especially when using an N=1 approach, as it is difficult to predict which patients will benefit (1). The Numerical Rating Scale (NRS) from 0 to 10 (0=no shortness of breath, 10=worst shortness of breath imaginable) is recommended as it was used in evidence cited. Treatment should focus on patients with an NRS ≥4, and especially those with scores ≥7.
PRESCRIPTION
As distress from breathlessness is not correlated to degree of hypoxemia. It is suggested therefore that oxygen flow rates be determined by symptom score on an individual basis rather than SpO2 reading (though caution is advised with this approach as cool air can relieve breathlessness which is why hand-held and other fans are useful and sometimes a lower flow rate plus a fan provide effective relief). Additional consideration needs to be given to potential risks of hypercapnia in those patients susceptible (commonly COPD and those with neuromuscular disease – see BTS guidance for detail) if oxygen is given at higher flow rates.
1. Nonoyama ML, Brooks D, Guyatt GH, et al. Effect of oxygen on health quality of life in patients with chronic obstructive pulmonary disease with transient exertional hypoxemia. Am J Respir Crit Care Med 2007;176(4):343–9
Chronic Obstructive Pulmonary Disease in over 16s in diagnosis and management 23/24 of 65
https://www.nice.org.uk/guidance/ng115
The recommendations in this document relate to patients with COPD. After discussion with part of the committee who wrote the guidelines, the safety considerations and smoking recommendations could stand regardless of disease prognosis.
EQUIPMENT
Concentrator or cylinder as determined by patients’ needs. If the need is intermittent, then static cylinders may be considered. If it is considered, however, that the patients’ needs are going to increase to >4 hrs a day, then a static concentrator should be first choice.
NB Oxygen cannot be stored in the body, so using it pre-exertion to ‘stoke up’ is unhelpful; likewise, replacing lost oxygen post exertion is unnecessary as levels will normalise with rest anyway, so the perceived desire for a ‘few whiffs’ here and there, pre or post exertion, is not an indication. Hypoxaemia on exertion should be managed with AOT.
The NHS pays for every delivery of static cylinders and so, if a patient deteriorates, a new HOOF may be required, or the patient may have to keep ordering urgently, which is both an added stress at a difficult time for the patient and their family, and adds to the £108M (Correct 2018) National home oxygen bill.
FOLLOW UP
Oxygen therapy, like any pharmacological intervention, should be best considered on a trial basis and be reviewed regularly, while balancing benefits and risks. Most benefit is likely to occur in the first 24 hours, and nearly all symptomatic and functional improvements within the first 3 days of use (1). Follow-up and assessment of response should fit with these timescales.
If the patient still requires oxygen, both a consent form and the Initial home oxygen risk mitigation form (IHORM) need to be filled in and signed before oxygen is requested. (There is a guidance document and a FAQ for the new consent form). All the documents for a GP or OOA team are below. Some areas will have these forms already uploaded onto local systems e.g. EMIS
[LINKS REQUIRED AS DOCUMENTS NOT EMBEDDED PROPERLY IN DOCUMENT]
Final IHORM_ IG approved 298 v1 3.pdf
Final IHORM_ IG approved 298 V123.doc
IHORM guidanceVersion 10 N.pdf
IG approved FAQIHORM and Consent fo.pdf
Updated Part A HOOF final March 17 V123.doc
Updated Part A HOOF Final March 17 V.1.pdf
Assuming the patient passes the risk mitigation form then a HOOF needs to be raised.
How to send the HOOF
DO NOT SEND the Consent form or IHORM to the oxygen supplier
- All supplier details are below
- Please check which region you are based in
- Please note this is correct as for Nov 2020.
AIR LIQUIDE HEALTHCARE Regions: South West, London
Air Liquide Part A Portal – https://www.airliquidehomehealth.co.uk/hcp
The portal:
- Allows you to download the IHORM and HOCF for completion prior to ordering oxygen
- Guides you through the ordering process and automatically sends the order to Air Liquide
- Provides a copy of the submitted HOOF to download and add to patient records
- Allows you to request removals when oxygen is no longer required call Prescriber Support Team on 0808 202 2099 for more support.BOC regions: East of England, East Midlands (Milton Keynes see South Central Region)
Telephone: 0845 609 4345 Clinical Line
BOC Home Oxygen Portal Main Page:
https://www.bochealthcare.co.uk/hop/Clinician Registration:
https://www.bochealthcare.co.uk/hop/RegisterAsNHSStaff.aspxVideo Instructions:
Note: If you anticipate needing to prescribe oxygen at any point in the future it is highly recommended you register in advance at your earliest convenience so you can familiarise yourself with the BOC Home Oxygen Portal and its features.
BAYWATER Ltd Regions: There are different Home Oxygen ordering procedures in place for each of the Baywater Regions. Yorkshire & Humber, Wales and the North West use the Baywater Portal. West Midlands use a dedicated NHS Portal: OxyShop. Please see below for further information:
Yorkshire and Humber, Wales, North West
For Yorkshire and Humber, Wales, and North West HOS Regions the Baywater portal is available on https://apps.baywater.co.uk/onlineportal/:
Access to the Baywater portal requires all Healthcare Professionals (HCPs) to register using a secure @nhs.net, @wales.net, or a DCB1596 accreditation secure email @nhs.uk email address; and
- Provides online training, via a video, to support the registration process
- Allows the HCP to download the IHORM and HOCF for completion prior to ordering oxygen
- Guides the HCP through the ordering process and automatically sends the order to Baywater Healthcare
- Provides a copy of the submitted HOOF to download and add to patient records
- Allows the HCP to request equipment removals when oxygen is no longer required
- Provides online training, via a video, relating to completing a HOOF, equipment instructions etc.
- Electronic confirmations generated and sent to the HCP, as the order is received and the processed.
If a Healthcare Professional has problems registering or accessing the Baywater portal please contact Baywater colleagues by ringing 01270 218050.
Healthcare Professionals (HCPs) have the ability the e mail to HOOFs to Baywater via a secure e mail address: bhltd.ehoof@nhs.net
BAYWATER PORTAL (You will need to register on the portal)
https://apps.baywater.co.uk/onlineportal/Account/Register
The portal allows for completion of the IHORM and will guide the user through the ordering process of a HOOF A.
Once completed the HOOF A will send electronically preventing the need for printing.
If you have problems registering please call 01270 218050 for the clinical line.
West Midlands Only
All orders for Home Oxygen Services in the West Midlands must be made via OxyShop.
OxyShop is the dedicated ‘NHS Patient and Finance Management System’ used by all Clinical Commissioning Groups (CCGs) operating in the West Midlands. The OxyShop Portal can be accessed via www.oxyshop.org
You cannot order home oxygen services before registering as a user on the OxyShop Portal. As part of the registration process your professional registration will be checked; this is to ensure that it is appropriate for you to prescribe Home Oxygen Therapy.
The OxyShop Portal allows for end-to end completion of a HOOF A or B and the Initial Home Oxygen Risk Mitigation Form (IHORM). At all stages the user will be guided through the ordering process.
Once completed, the HOOF will be sent electronically to Baywater Healthcare Limited with the prescribing clinician receiving confirmation of HOOF transmission and action.
For video guides and help using OxyShop, please visit
https://www.oxyshop.org/home/support
If you require further information or support, please contact us email the OxyShop Support Team on Oxyshop.Service@nhs.net or call Tel: 0121 612 2806/1675.
DOLBY VIVISOL regions: South Central, South East Coast, North East
As a Part A HOOF prescriber, Part A portal link is below – Your professional number will not be held by Dolby Vivisol
[LINK BROKEN] https://www.dolbyvivisol.com/services/healthcare-professionals/home-oxygen- services/england/ihorm-and-hoof-part-a/
Using your NHS.net or secure professional email and your professional registration number, you will be sent a verification code in order to gain access to the HOOF Part A form. Once the completed form has been submitted, a confirmation of your prescription will be sent to you and the Dolby Vivisol HOOF team for processing.
In the event that the portal is not functioning please email your completed HOOF to hoof.dv@nhs.net
If being sent by NHS.net, contact the supplier if the email is not below, and ensure the clinician signature is replaced by “sent from my nhs.net account”. This acts as the signature as it is sent from a named account. HOOFs cannot be sent from generic nhs.net accounts.
Email HOOF from the signatory of the HOOF from their nhs.net account.
(Please sign by typing “sent from my NHS.net email.”)
Any issues please ring the Clinical line T: 0800 0778020.
Dolby Vivisol Website link/ portal this guides clinicians through the process in a video of how to fill in a part A HOOF
[BROKEN LINK]
https://www.dolbyvivisol.com/services/healthcare-professionals/home-oxygen- services/england/oxygen-therapy/
Filling in the Part A HOOF
This extract for completing HOOF Part A is taken from the Dolby Vivisol and BOC ‘Completing a HOOF’ guides.
In very exceptional circumstances a verbal HOOF may be requested. Please contact the local home oxygen supplier for guidance. N.B. If requested the outstanding HOOF must be sent to the supplier within 24hrs of the request being made.
Some Suppliers encourage you to use their portal see local contact details on 5/6. Other suppliers request that you email the hoof on a named nhs.net address.
Please note from the roll out of the new contract in 2020 across most of England and Wales the use of Faxes is no longer acceptable.
Section 1 and 2: Patient and Carer Details
Please fill in all the boxes, with particular attention to including NHS number and contact details.

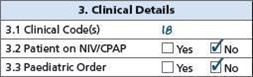
Section3: Clinical Details
Complete the clinical coding to assist in data management and on-going reviews to provide an integrated care plan for the patient where required. Clinical Code definitions can be found in section 14 of the HOOF Part A and are now mandatory from 1st August 2017. On the very rare occasion where the patient is using NIV/CPAP or is a paediatric patient, it is recommended that you refer to their Respiratory Clinician/Paediatrician.
Section 4: Patient’s Registered GP Information
Enter the details of the GP with whom the patient is registered.

Section 5: Assessment Service (Hospital or Clinical Service)
Please complete the details of the Assessment Service that will be used for follow-up purposes. This enables us to communicate effectively and ensure seamless care for the patient. Prompt communication with specialist assessment centres/specialist respiratory teams will ensure that they are informed of the situation and are able to assess the patient at the earliest opportunity.

Section 6: Ward Details (if applicable)
If the patient is in hospital and due for discharge, section 6 should be completed. This will enable us to liaise with the hospital to ensure a smooth and consistent process with minimal delays disruptions.
Sections 7, 8, 9: Ordering
Section 7 relates to the oxygen the patient should use. The flow rate of oxygen needs to be stated, together with the number of hours of therapy required per day. All parts are marked as mandatory; failure to complete in full will result in potential rejection and ensuing delay in the provision of supply.
The flow rate must be given as litres per minute. If a fractional component is required (e.g. 0.5,
1.5 LPM etc.) please ensure the decimal point is clearly marked. There should also be a digit to the left of the decimal point (e.g. 0.5 rather than .5).
The period of use required to meet the patient’s need must be stated in hours per day, although periods of less than one hour can be expressed in minutes (e.g. 15 minutes or 15 min).
Section 8 – The choice of equipment will ideally be based on a) the flow rate b) period of use and c) expected length of treatment.
Ultra-high flow rates (> 12 LPM) are generally provided via cylinder supply, particularly if period of use is short (e.g. 15 – 20 minutes per day) Cluster headache patients are the most common patients to require static cylinders at these ultra-high flow rates.
- Lower flow rates and short periods of use (e.g. 1.5 LPM for 1hour per day) will generally best be provided via cylinder supply
- Longer periods of use (e.g. above 4 hours per day) will generally best be provided via concentrator supply
- Where the supply is likely to be in situ for a short period of time (e.g. a few days), with a consistent modest flowrate and period of use, again cylinder supply may be best, but if there is a concern that usage is going to increase, then a concentrator should be considered, to save the family and patient from extra stress at this difficult time.
The quantity to be ordered will depend on flow rate (concentrators) or flow rate & period of use (cylinders), please consult your home oxygen supplier.
For section 9, a choice of either nasal cannula or mask should be made. Most patients would use a nasal cannula unless there are issues with mouth breathing, the home oxygen supplier should be able to give advice. For Cluster headache patients a 100% non-rebreather mask is the default mask.

Section 10: Delivery details
Please indicate the delivery timescale required. Be aware that there are cost implications if using other than standard delivery times.
![]()
Section 11: Additional Patient Information
If you would like the oxygen assessment centre to review the patient within a timescale, please indicate which month and year the review would be required. For example, write “Review: April 2020”. If no date is specified, we will notify the assessment centre to review the patient in 6 months’ time.
Additionally, this section should be used to advise us of any special information relating to the patient’s oxygen supply and on-going support requirements. This could include, for exa[mple, physical disabilities, language difficulties, non-English speaker.

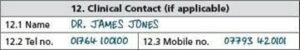
Section 12: Clinical Contact (if applicable)
The details of the clinical contact for the patient need to be incorporated here. It is possible that this may be the same person signing the HOOF Part A and, in this case, those details must be repeated here.
Section 13: Declaration
This declaration is mandatory and must be fully completed before the HOOF Part A is sent to the supplier. Both the Consent form and IHORM must be filled in and ticked.
For all new patients, these forms must be signed off appropriately by the clinician and the patient/ patient’s representative. If it is any existing patient please confirm with the patient that the forms were signed previously and it maybe in their notes.
It is very important that not only is the declaration signed, but also a NHS email address or an approved secure email is provided so that we are able to send confirmation/corrections back.
Section 14: Clinical Code:
This must be added to Section 3 as it is a mandatory requirement
We would strongly advise that ‘Referred for Assessment’ boxes are completed and, if
possible, send both forms to your local home oxygen teams for follow up.
If the patient has passed away then this can be called through to the supplier by family or carers.
Otherwise an email should be sent to the supplier to request removal by an HCP.
If oxygen is removed as it is no longer clinically appropriate, the patient does not want to use it, or following failure of a risk assessment, an email should be sent to the supplier to request removal by an HCP after agreement with the prescriber, the local HOS team or GP.
