Guidance for healthcare teams on the release of adult patients from the secure and detained estate during coronavirus (COVID-19)
Contents
- Process for identification of potential patients for release
- Considerations for healthcare teams
- Appendix
Publication approval reference: C0434
19 May 2020, Version 1
Process for identification of potential patients for release
- List of patients identified by Her Majesty’s Prison and Probation Service (HMPPS) is created for each cohort. This list details prison number, name and site location and will be sent to your site governor/director.
- The governor/director will risk assess the patients and decide if a patient can be released under the early release scheme.
- Healthcare providers will be informed either through NOMIS (National Offender Management Information System) or directly from the governor of potential eligible patients. Sites are advised to follow the patient view instructions (TPP S1) and check all relevant information is in place, such as:
- registered community GP
- referrals to community mental health and substance misuse
- whether a patient is to receive the shielding letter registered community GP
- home address on release
- medication needs
- whether the patient has been displaying symptoms of COVID-19
- whether the patient has been tested for COVID-19 and any results.
- From this information, you will need to advise the governor/director of any pertinent information relating to individual patients, which they may need to consider before potential early release.
- See the patient up to 48 hours prior to release and complete the relevant release planning/release secure environment assessment tool (SEAT) template.
- For patients who do meet the requirements for early release, healthcare providers need to ensure:
- the pharmacy is aware of release and can prepare any take home medication
- referrals to community providers, such as substance misuse and mental health, are in place for release.
Considerations for healthcare teams
Pharmacy
Make sure pharmacy leads receive the patient list of potential releases at the earliest opportunity and prescribers are tasked with issuing urgent prescriptions for these patients. Pharmacies providing dispensing services that are outside the prison must be notified, so they can expect these urgent prescriptions which will require delivery to the prison under contracted urgent delivery arrangements. The health and justice (HJ) chief pharmacist for your organisation will have received guidance on issuing take home medication and FP10MDA to ensure continuity of care following release.
This information can be used to organise 28-day supplies for identified persons or arrange provision of a FP10 prescription, if timings do not allow for a pharmacy supply. This will ensure patients are able to continue to access medicines post-release via GPs. If a person is not released, the medicines can be used for the patient’s next supply while in prison.
As for usual releases, doses of substance misuse medicines should be administered before the person is released. FP10MDA prescriptions can be used to supply ideally up to 14 days supervised consumption, or daily pickup as a bridging supply, until community services can be accessed. When release is happening on a Friday, consideration may need to be given to supplying a labelled supply of opioid substitution therapy from the prison for Saturday and Sunday to avoid omitted doses. Where possible, we advise collaboration with community substance misuse about managing these persons.
Note that the costs for the additional release medicines will be included in financial pressures for HJ COVID-19. Providers are advised to record these additional supplies as this may be needed for any future reimbursement of the costs.
Pregnant patients and women on mother and baby units
The key elements required for discharge planning are:
- Through the Gate service must be trauma informed.
- Housing should be confirmed.
- All women must be offered GP registration.
- All women must be referred to social services to make an assessment regarding the unborn child or the child. This should include details of any children in the home where the mother will be residing.
- Women in their second and third trimester must be allocated a link midwife at the birthing unit of choice. As part of this, additional consideration should be given to those women whose birth is imminent during this stressful time.
- All women must be made known to local named safeguarding midwife.
- Mothers must be asked if there is a protection plan in place for the unborn child and this should be clearly documented. If so, the essence of the plan, available from the social worker, must inform all decisions relating to release planning and location of release. All protection plans must be logged via Child Protection – Information Sharing (CP-IS).
Patients with a registered GP in the community
Make sure the registered GP receives an email containing a health summary for the patient and a short email, which states that the patient has been released and whether they fall into the shielding category. If the patient falls into the shielding category, ensure they are given a printed copy of the shielding letter. (Letter template is listed on your S1 unit.) Also state what medication the patient has left prison with.
Patients without a registered GP
For patients who do not have a registered GP, you must pre-register the patient prior to them leaving the detained estate. If you require assistance in Pre Registering a patient prior to release contact your delegated Primary Care Service at the Clinical Commissioning Group (CCG) for that area or NHS England and NHS Improvement regional team for the area the patient is being discharged to, please email Amanda Hizzett at ahizzett@nhs.net. Email the chosen GP practice with the completed GMS1 form, and a health summary, and notify the receiving practice of the shielding status and any medication the patient has been discharged with.
Patients leaving site and returning to Wales
For patients who are leaving the site and returning to Wales, please contact NHS Wales to inform NHS Wales of patients who are returning at COVID-19Wales@justice.gov.uk. This mailbox is monitored regularly.
Patients seen by clinician on the day of release
If a clinician sees a patient on the day of their release and they are symptomatic, the clinician has a public health duty of care to inform the local health protection team (HPT), as well as the probation provider or responsible community rehabilitation responsible officer, as they may be required to take further action in relation to patient transport or licence conditions. Further information can be found here: www.gov.uk/guidance/notifiable-diseases-and-causative-organisms-how-to-report
Registered medical practitioners (RMPs) have a statutory duty to notify the ‘proper officer’ at their local council or local HPT of suspected cases of certain infectious diseases.
RMPs should complete a notification form immediately on diagnosis of a suspected notifiable disease. They should not wait for laboratory confirmation of a suspected infection or contamination before notification.
Public Health England aims to detect possible outbreaks of disease and epidemics as rapidly as possible. Accuracy of diagnosis is secondary, and since 1968 clinical suspicion of a notifiable infection is all that is required.
‘Notification of infectious diseases’ is the term used to refer to the statutory duties for reporting notifiable diseases in the Public Health (Control of Disease) Act 1984 and the Health Protection (Notification) Regulations 2010.
Information sharing required on release
The released patient’s healthcare summary must be emailed to the registered GP on release. Summaries must be sent via secure email.
Supporting Shielding for vulnerable patients
NEL Commissioning Support Unit have placed the shielding letter template into your S1 unit. Patients who fall into the shielding category must be supplied with this letter on release as it provides advice on how they can protect themselves and access the care and treatment they need.
In support of this, patients who might need support while self-isolating can be referred to NHS Volunteer Responders for help with tasks such as collecting shopping and prescribed medicines or driving patients to medical appointments. Referrals can be made through the NHS Volunteer Responders referrers’ portal or by calling 0808 196 3382. The scheme will soon be open for self-referrals by calling 0808 196 3646 between 8.00am and 8.00pm.
Appendix
NHS volunteer responder scheme: information is available at https://volunteering.royalvoluntaryservice.org.uk/nhs-volunteer-responders
FAQs for referrers (such as NHS staff, including GPs and pharmacists and local authority colleagues) to refer vulnerable people for support from an NHS volunteer responder is available here: https://www.england.nhs.uk/coronavirus/publication/preparedness-letters-for-general-practice/
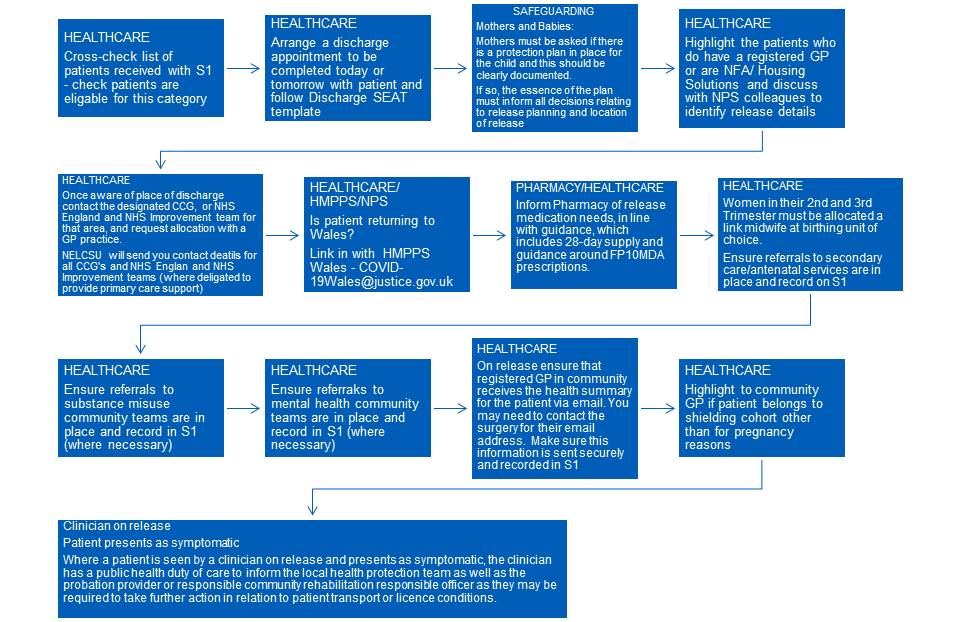
Cohort release – flowchart – 28 April 2020