Key actions – winter 2022 preparedness: nursing and midwifery safer staffing
Contents
- Planning
- Decision making and escalation
- Staff training and wellbeing
- Indemnity and regulation
- Governance and assurance
- Useful links
- Appendix 1: Decision tool and escalation framework
- Appendix 2: Example quality impact assessment
- Appendix 3: Example staffing SBAR Tool
- Appendix 4: Example risk appetite statement
- Appendix 5: Assurance framework – nursing and midwifery staffing
- Appendix 6: Example safe staffing governance framework
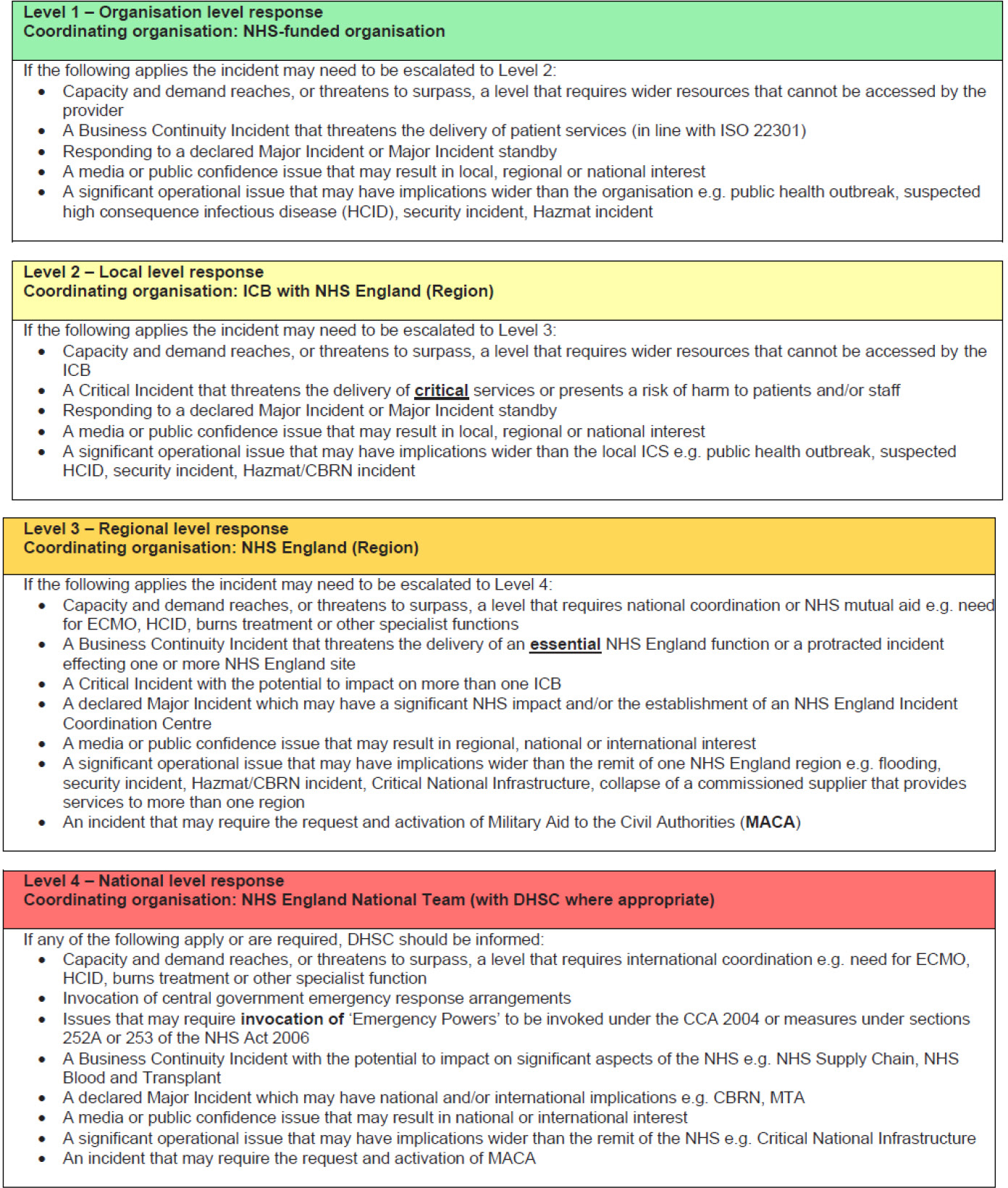
- Appendix 7: EPRR escalation and alerting
Classification: Official
Publication approval reference: PAR2072 / BW2072
November 2022, Version 2, updates to version 1 are highlighted.
Trust board members are collectively responsible for workforce planning, practice and safeguards. The following actions focus on preparedness, decision making and escalation processes to support safer nursing and midwifery staffing as the winter period approaches. They build on the previous guidance issued in relation to staffing in extremis workforce models and the fundamental principles for the nursing and midwifery workforce as set out in the National Quality Board (NQB) Safe Sustainable and Productive staffing guidance. The document summarises and signposts to existing resources, tools, and templates in support of nursing and midwifery workforce planning, preparation, and board assurance.
Planning
- When planning the nursing and midwifery workforce, boards should ensure that system wide and local learning from previous staffing deployments, including from the Covid-19 pandemic continue to be incorporated into staffing escalation plans.
- Work with providers of temporary workforce to be clear about anticipated requirements during activity peaks and consider steps such as block booking for hard to fill areas.
- Executive directors of nursing should ensure that all forecast staffing plans are reviewed weekly or more frequently as required by the operating context and changing circumstances. Executive directors of nursing are expected to work with the Board and with ICBs/ICSs to align system approaches to workforce planning.
- Changes in estate function or staffing configuration should be subject to a quality impact assessment with final sign-off by the executive director of nursing and countersigned by the medical director as joint quality lead.
- Redeployment should be voluntary where possible and individual risk assessments must be undertaken with staff prior to any redeployment.
- Now that ICBs/ICSs are operational, trusts must consider whether system level solutions are appropriate.
Decision making and escalation
- Even during challenging times, executive directors of nursing should be mindful of the fundamental principles set out in the NQB Safe Sustainable and Productive staffing guidance and Developing Workforce Safeguards guidance.
- When implementing escalation plans, decisions regarding skill mix and staffing numbers should be taken in conjunction with an assessment of patient acuity and dependency, professional judgement and the environment of care.
- In preparation for periods of increased demand, organisations should ensure that staffing plans are reviewed and signed off by the executive director of nursing, with staffing decisions including redeployment and daily deployment of staff led by the senior clinical leadership teams.
- Staffing risk assessments should be undertaken on a shift by shift basis and concerns and issues escalated in a timely manner via clearly established routes. Unresolved issues should be escalated in line with provider governance processes. A system wide discussion and focus should be taken to reach solutions wherever appropriate.
- Escalation mechanisms and governance processes should be clear to all staff and the board should seek assurance that effective escalation occurs and that issues are addressed and recorded.
- Staff should be supported to discuss and raise concerns regarding staffing and their ability to safely care for patients. The board must seek assurance that there are clear mechanisms in place for staff to raise concerns and that these are acknowledged and mitigated where possible.
- Clinical leaders should take a multi-professional and skills-based approach to staffing and ensure each clinical area is supervised by a senior clinical leader.
Staff training and wellbeing
- Supporting the workforce is paramount; boards should seek assurance that there are well-publicised and accessible resources in place for staff.
- Staff wellbeing should be embedded at every level. For example, team-based check- ins, wellbeing support hubs and wobble rooms.
- Professional nurse/midwife Advocates (PNA/PMAs) who are trained to provide confidential restorative clinical supervision and support nurses in clinical practice, should be readily available.
- Boards should ensure that local leaders are supporting staff wellbeing, which in turn will support the delivery of high standards of patient care.
Indemnity and regulation
- It is recognised that at times staff might need to act outside their normal role or places of work/scope of practice. A risk-based approach should be used to mitigate emerging risks using available resources effectively and responsibly.
- The UK’s Chief Nursing Officers, the CQC and the NMC have published a joint letter on how staff will be supported over the winter period.
- Working in partnership with people receiving care and their fellow professionals remains of utmost importance; and of using professional judgement to assess risk, informed by the values and principles set out in NMC professional standards. Trust boards must be assured that wherever possible these standards are met.
Governance and assurance
- There must be a clear and effective line of sight from point of care delivery to board, in relation to nursing and midwifery staffing decisions and challenges.
- To help boards understand the quality impact of decisions that have been taken around staffing, boards should be provided with triangulated information linking staffing with wider intelligence, through regular reporting. For example incidents, complaints and NICE red flags.
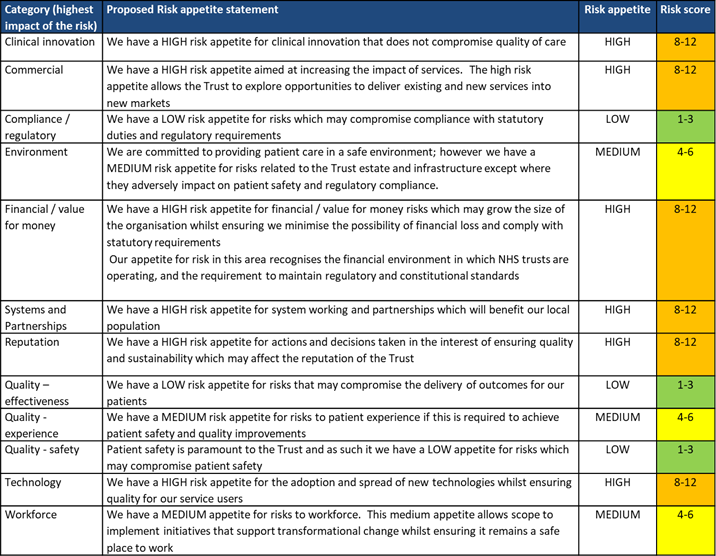
- Boards should have reviewed their risk appetite in relation to quality and workforce risks and be clear on the tolerances the board is willing to accept, understanding that not all risks can be fully mitigated. This should be clearly communicated to the organisation.
- Boards should seek assurance that plans are in place to ensure safe nursing and midwifery staffing over the winter period and that these plans are connected to the wider system staffing planning, resourcing and mutual aid.
- The Care Quality Commission (CQC) recognises that services are facing tremendous challenges as result of the pandemic – and that the nursing and midwifery workforce is experiencing these pressures particularly acutely. This includes decisions around nursing, midwifery and care staffing capacity and capability. CQC expects boards to make staffing decisions with a focus on mitigating emerging risks and trends using available resources effectively and responsibly, in line with national guidance – and that where staffing shortages are identified, use of temporary solutions including a multidisciplinary approach to manage immediate risks should be implemented.
- Where necessary, ICBs/ICSs, CQC and regional NHS England and NHS Improvement teams should be made aware of any fundamental concerns arising from significant and sustained staffing challenges.
- People first is an online resource available on CQC’s website for system leaders and service providers. It presents suggested actions for individual services and the wider system to help manage the challenges in urgent and emergency care and includes a section on staffing and staff training.
Useful links
Alongside the formal guidance that has previously been issued in this area, a collection of additional resources has been collated for use by providers. These resources are attached as appendices and/or via the following links:
Planning
|
Staff training and wellbeing |
Decision making and escalation
|
Governance and assurance
|
Appendix 1: Decision tool and escalation framework
Flow chart for resolution of staff shortages, to support nurse(s) in charge and matrons on a shift-by-shift basis. (Courtesy of Oxford University Hospitals)
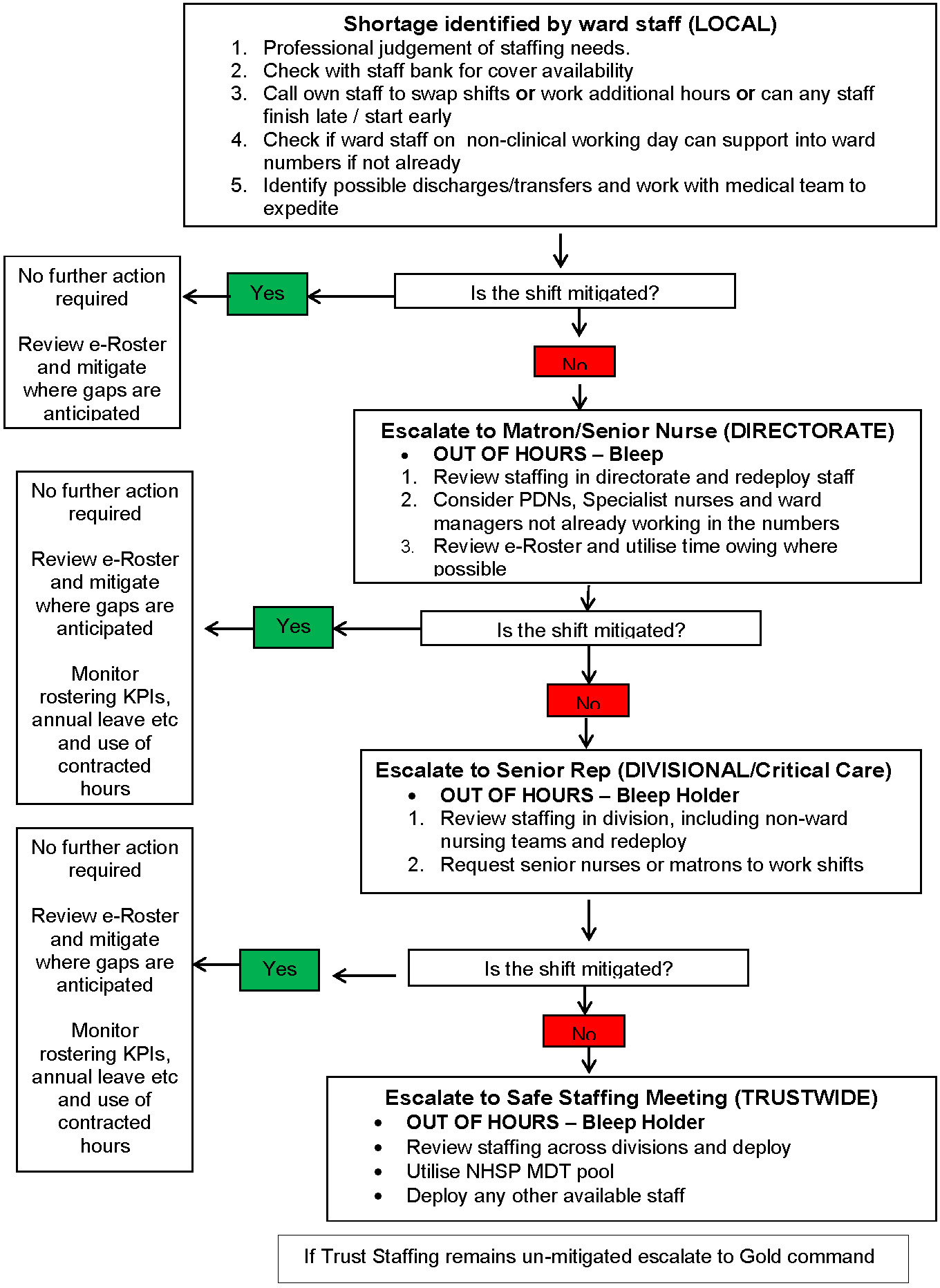
Level 1Required staffing levels achieved across most wards Required CHPPD met Activity can continue as planned |
Local redeployment of staff within and across Divisions has mitigated staffing requirements
Activity unaffected “Business as usual can continue” |
Level 2Staffing levels remain below planned across most wards CHPPD across organisation are not met Monitoring must continue. |
Follow Level 2 protocol
Non – ward based nursing teams across divisions are supporting patient care |
Level 3Staffing levels remain considerably lower than planned despite mitigation nurse to patient ratios 1:8 on adult wards, 1:6 on children’s wards, and nurse 1 and 2 model in critical care and respiratory high care Significant deficiency in required CHPPD across organisation Activity cannot continue as normal |
All other protocol exhausted Step down of all non-urgent meetings Study leave cancellation mandated Urgent meeting of divisional directors of nursing with head nurse for workforce to discuss any further possible mitigation. (If declared at the weekend duty manager to meet with ops and senior representative from each division)Review all planned elective and emergency activity to prioritise care and deployment of staff, consider regional supportTrust wide deployment of indirect patient care staff considered to support delivery of direct care. As with OPEL 4, all effort will be focussed until step down to level 1 or 2 has been achieved. |
Appendix 2: Example quality impact assessment
Follow this link to view (FutureNHS account required): https://future.nhs.uk/BeneficialChangesCOVID19/view?objectId=93995109
Appendix 3: Example staffing SBAR Tool
Staffing communication tool using situation, background, assessment, recommendation (SBAR) principles to ensure critical staffing issues are received and actioned.
Situation:
Ward:
Date, Shift and Band that require covering:
Number of beds:
Acuity and dependency score:
Describe your concern, include Safety/Quality concern:
Background:
Current problem:
Reason for problem on shift:
How long has the shift been out to the Hospital Nurse Bank:
How long has the shift been out to Framework Agency:
Assessment:
My assessment of the situation is:
Current concern:
Describe actions that have been taken to solve the current problem:
Recommendation:
Based on my assessment I request that you approve:
Things to consider:
Explain what you need:
Appendix 4: Example risk appetite statement
For boards and senior leaders outlining the pressures on the service and any potential changes in the level of accepted risk.
Appendix 5: Assurance framework – nursing and midwifery staffing
For quality (or other board level) committees and board members to support discussion and challenge surrounding the active staffing challenges faced and the potential impact this may have on patients.
| Ref | Details | Controls | Assurance (positive and Negative) | Residual Risk Score / Risk register reference | Further action needed | Issues currently escalated to Local Resilience Forum / Regional Cell / National Cell |
Ongoing Monitoring / Review |
| Guidance notes | Outline the current controls (controls are actions that mitigate risk include policies, practice, process and technologies) | Detail both the current positive and negative assurance position to give a balanced view of the current position Assurance is evidence that the control is effective – or conversely is evidence that a control is ineffective / there are still gaps Recurrent forms of assurance are audit results, key performance indicators, written reports, intelligence and insight. Effective Assurance should be a triangulated picture of the evidence (staff shortages, sickness absence, pt outcomes, complaints, harm reviews) |
What is the remaining risk score (using the trusts existing risk systems and matrix) Are these risks recorded on the risk register? |
Where there are identified gaps in either control or assurance, outline the additional action to be undertaken to mitigate the risk. Where the organisation is unable to mitigate fully, this should be escalated to the LRF/region/national teams and outlined in the following column |
Provide oversight to the board what the current significant gaps are
Outline those risks that are currently not fully mitigated /needing external oversight and support |
Due to the likely prevailing nature of these risks, outlines through what operational channels and how are these active risk being monitored (e.g daily silver meetings via safe staffing heatmap) |
|
| 1. Staffing Escalation / Surge and Super Surge Plans | |||||||
| 1.1 | Staffing Escalation plans have been defined to support surge and super surge plans which includes triggers for escalation through the surge levels and the corresponding deployment approaches for staff.
Plans are detailed enough to evidence delivery of additional training and competency assessment, and expectations where staffing levels are contrary to required ratios (i.e intensive care) or as per the NQB safe staffing guidance |
||||||
| 1.2 | Staffing escalation plans have been reviewed and refreshed with learning incorporated into revised version in preparation for winter. | ||||||
| 1.3 | Staffing escalation plans have been widely consulted and agreed with trust’ staff side committee | ||||||
| 1.4 | Quality impact assessments are undertaken where there are changes in estate or ward function or staff roles (including base staffing levels) and this is signed off by the CN/MD | ||||||
| 2.0 Operational delivery | |||||||
| 2.1 | There are clear processes for review and escalation of an immediate shortfall on a shift basis including a documented risk assessment which includes a potential quality impact.Local leadership is engaged and where possible mitigates the risk.Staffing challenges are reported at least twice daily via Bronze. |
||||||
| 2.2 | Daily and weekly forecast position is risk assessed and mitigated where possible via silver / gold discussions.
Activation of staffing deployment plans are clearly documented in the incident logs and assurance is gained that this is successful and that safe care is sustained. |
||||||
| 2.3 | The Nurse in charge who is handing over patients are clear in their responsibilities to check that the member of staff receiving the patient is capable of meeting their individual care needs. | ||||||
| 2.4 | Staff receiving the patient (s) are clear in their responsibilities to raise concerns they do not have the skills to adequately care for the patients being handed over. | ||||||
| 2.5 | There is a clear induction policy for agency staff
There is documented evidence that agency staff have received a suitable and sufficient local induction to the area and patients that they will be supporting. |
||||||
| 2.6 | The trust has clear and effective mechanisms for reporting staffing concerns or where the patient needs are outside of an individuals scope of practice. | ||||||
| 2.7 | The trust can evidence that the mechanisms for raising concerns about staffing levels or scope of practice is used by staff and leaders have taken action to address these risks to minimise the impact on patient care. |
||||||
| 2.8 | The trust can evidence that there are robust mechanisms in place to support staff physical and mental wellbeing.
The trust is assured that these mechanisms meet staff needs and are having a positive impact on the workforce and therefore on patient care. |
||||||
| 2.9 | The trust has robust mechanisms for understanding the current staffing levels and its potential impact on patient care.
These mechanisms take into account both those staff who are absent from clinical duties due to required self Isolation, shielding, and those that are off sick. Leaders and board members therefore have a holistic understanding of those staff not able to work clinically not just pure sickness absence. |
||||||
| 2.10 | Staff are encouraged to report incidents in line with the normal trust processes.
Due to staffing pressures, the trust considers novel mechanisms outside of incident reporting for capturing potential physical or psychological harm caused by staffing pressures (e.g use of arrest or peri arrest debriefs, use of outreach team feedback etc) and learns from this intelligence. |
||||||
| 3.0 Daily Governance via EPRR route (when/if required) | |||||||
| 3.1 | Where necessary the trust has convened a multidisciplinary clinical and or workforce /wellbeing advisory group that informs the tactical and strategic staffing decisions via Silver and Bronze to provider the safest and sustained care to patients and its decision making is clearly documented in incident logs or notes of meetings. | ||||||
| 3.2 | Immediate, and forecast staffing challenges are discussed and documented at least daily via the internal incident structures (bronze, silver, gold). | ||||||
| 3.3 | The trust ensures system workforce leads and executive leads within the system are sighted on workforce issues and risks as necessary.
The trust utilises local/ system reliance forums and regional EPRR escalation routes to raise and resolve staffing challenges to ensure safe care provided to patients. |
||||||
| 3.4 | The trust has sufficiently granular, timely and reliable staffing data to identify and where possibly mitigate staffing risks to prevent harm to patients. | ||||||
| 4.0 Board oversight and Assurance (BAU structures) | |||||||
| 4.1 | The quality committee (or other relevant designated board committee) receives regular staffing report that evidences the current staffing hotspots, the potential impact on patient care and the short and medium term solutions to mitigate the risks. | ||||||
| 4.2 | Information from the staffing report is considered and triangulated alongside the trusts’ SI reports, patient outcomes, patient feedback and clinical harms process. | ||||||
| 4.3 | The trusts integrated Performance dashboard has been updated to include COVID/winter focused metrics.
COVID/winter related staffing challenges are assessed and reported for their impact on the quality of care alongside staff wellbeing and operational challenges. |
||||||
| 4.4 | The Board (via reports to the quality committee) is sighted on the key staffing issues that are being discussed and actively managed via the incident management structures and are assured that high quality care is at the centre of decision making. | ||||||
| 4.5 | The quality committee is assured that the decision making via the Incident management structures (bronze, silver, gold) minimises any potential exposure of patients to harm than may occur delivering care through staffing in extremis. | ||||||
| 4.6 | The quality committee receives regular information on the system wide solutions in place to mitigate risks to patients due to staffing challenges. | ||||||
| 4.7 | The Board is fully sighted on the workforce challenges and any potential impact on patient care via the reports from the quality committee.
The Board is further assured that active operational risks are recorded and managed via the trusts risk |
||||||
| 4.8 | The trust has considered and where necessary, revised its appetite to both workforce and quality risks given the sustained pressures and novel risks caused by the pandemic
The risk appetite is embedded and is lived by local leaders and the Board (i.e risks outside of the desired appetite are not tolerated without clear discussion and rationale and are challenged if longstanding) |
||||||
| 4.9 | The trust considers the impact of any significant and sustained staffing challenges on their ability to deliver on the strategic objectives and these risks are adequately documented on the Board Assurance Framework | ||||||
| 4.10 | Any active significant workforce risks on the Board Assurance Framework inform the board agenda and focus | ||||||
| 4.11 | The Board is assured that where necessary CQC and Regional NHSE/I team are made aware of any fundamental concerns arising from significant and sustained staffing challenges | ||||||
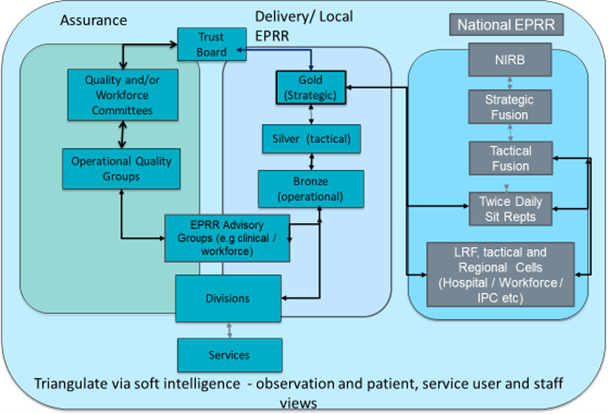
Appendix 6: Example safe staffing governance framework
The flowchart below is a general illustrative example. It outlines the two arms of a provider governance framework (assurance and delivery) and further indicates the relationships with the national emergency preparedness, resilience and response (EPRR) structures.
Providers must ensure that non-executive members of the board have clear sight of the significant or sustained operational issues and challenges that are being discussed in the day-to-day delivery of care during these challenging times.
This should be through their existing board assurance routes (ie quality committee, strategic workforce and organisational development committee to the board), to allow the non- executive directors to adequately fulfil their duties of holding the executive director members to account so that quality care is maintained.
Appendix 7: EPRR escalation and alerting
Extracted from NHS England EPRR Framework