Long COVID: the NHS plan for 2021/22
Contents
- Summary
- Summary of actions on Long COVID 21/22
- 1. What we know about Long COVID
- 2. Expanding Long COVID treatment and rehabilitation services
- 3. Enhancing general practice services to support patients with Long COVID
- 4. Long COVID in children and young people
- 5. Rehabilitation to manage the most common Long COVID symptoms
- 6. Extending the use of the Long COVID self-management digital tool
- 7. Improving data quality and transparency
- 8. Focus on equity of access, outcomes and experience
- 9. Supporting NHS staff with Long COVID
- Useful information
Classification: Official
Publications approval reference: C1312
Version 1, June 2021
Summary
- Highly debilitating for many sufferers, Long COVID is an increasingly widespread, multi-system condition. Regardless of the severity of their initial illness, it appears that anyone of any age – including children – can experience Long COVID.
- The term ‘Long COVID’ includes both ongoing symptomatic COVID-19 (5-12 weeks after onset) and Post-COVID-19 Syndrome (12 weeks or more). It is associated with a wide range of different symptoms impacting physical, psychological and cognitive health. It can also have an effect on quality of life and ability to work or attend education.
- As an initial response to the challenge of Long COVID, last October the NHS set out a 5-point plan:
- advice for clinicians and information for patients: NICE published the case definition in November and clinical guidance on managing the long-term effects of COVID-19 in December 2020
- providing Post-COVID Assessment Clinics. 89 clinics have now been established in England to offer specialist physical, cognitive or psychological assessment. While the second COVID-19 wave impacted them, early data showed increases to over 1500 referrals a week
- over 1.5 million visits have been made to the patient information section of the Your COVID Recovery website and over 100 rehabilitation services have been trained to support patients to use the specialist online rehabilitation support element
- on research, the NHS worked with the National Institute of Health Research to support studies to advance understanding of Long COVID with £50 million having now been committed to research
- finally, we have been much aided by the work of the NHS Long COVID Taskforce, which includes people with lived experience of Long COVID, NHS staff and researchers.
These foundations provide the basis for a further 10 key next steps, underpinned by an additional £100 million, to which the NHS now commits in 2021/22:
- £70 million to expand Long COVID services to add to the £24 million already spent on Post-COVID Assessment Clinics. By mid-July 2021, all local NHS systems will have submitted to regions, fully staffed Long COVID service plans covering the whole pathway from primary and community to specialist care. These should cover diagnostics, treatment, rehabilitation, children’s services and mental health services. To support this NHS England and NHS Improvement have developed a more detailed Long COVID clinical pathway, with help from an expert clinician group and people with lived experience, which was published as part of updated national commissioning guidance for Post-COVID Assessment Clinics in April 2021. (NICE. COVID-19 rapid guideline: managing the long-term effects of COVID-19, December 2020.)
- £30 million for the rollout of an enhanced service for general practice to support patients to be managed in primary care, where appropriate, and enable more consistent referrals to clinics for specialist assessment and treatment. Funding for the enhanced service will be made available to general practice to support professional education; support training and pathway development that will enable clinical management in primary care, where appropriate; and enable more consistent referrals to clinics for specialist assessment in line with the recently updated Commissioning Guidance; and planning to ensure equity of access.
- Care coordination. Care coordinators will support the running of Post-COVID Assessment Clinics. Long COVID can be a complex, multi-system disease. They will ensure care is joined up and prioritised based on clinical need. We will publish information about waiting times to ensure transparency.
- Establish 15 Post-COVID assessment children and young people’s hubs across England in order to coordinate care across a range of services. Building on the services already in place, these specialist hubs around England will provide assessment services or remote support to other clinicians and ensure ongoing holistic support.
- Develop standard rehabilitation pathway packages to treat the commonest symptoms of Long COVID. Local NHS systems will include a rehabilitation pathway programme in their Long COVID service plans due by mid-July 2021. It should be based on the principles included in the RightCare: Community Rehabilitation Toolkit.
- Extend the use of the Your COVID Recovery online rehabilitation platform. Local NHS systems will include planning to ramp up Your COVID Recovery supported patient-self management in their Long COVID service plans due by mid July 2021. The aim is to support those with Long COVID remotely to manage and monitor their symptoms where appropriate. Improved functionality will enable Your COVID Recovery online content to be translated into more than 100 languages. Work will also be undertaken to ensure improved accessibility through inclusion of easy read options and a printed manual which replicates online content.
- Collect and publish data to support operational performance, and clinical and research activities. From September 2021 onwards, NHS Long COVID activity data on referral, assessments and waiting times for post-COVID assessment clinics and the onward patient journey, including use of Your COVID Recovery, will be published monthly. A Long COVID registry for patients attending the Post-COVID Assessment Clinics will be established by July 2021. This registry will facilitate understanding of the longitudinal patient journey and support operational, clinical and research activities, through data linkage across national data collections. Importantly, it will also allow a more granular understanding of healthcare access for groups who experience health inequalities.
- Focus on equity of access, outcomes and experience. The NHS will use data tools to track take up by gender, ethnicity and deprivation, against expected prevalence. We will partner with National Voices, Asthma UK/British Lung Foundation and other Voluntary, Community and Social Enterprise Sector (VCSE) organisations to engage with communities more likely to be impacted by health inequalities. NHS England and NHS Improvement will appoint six Patient and Public Voice Partners to provide advice on Lived Experience to the programme. We will carry out a Health Equity Audit to assess the degree to which we achieve our vision of equitable access, excellent experience and optimal outcomes for all communities.
- Promote good clinical practice through the national learning network on Long COVID for healthcare professionals including a network for nurses working in community and acute care and for the wider NHS. We have developed a site on the FutureNHS platform to provide educational materials and enable information sharing across healthcare organisations and staff.
- Support our NHS staff suffering from Long COVID by offering a package of comprehensive support for health and wellbeing including mental health hubs, rapid referral to services, local occupational health and online wellbeing resources.
Summary of actions on Long COVID 21/22
| Actions | Delivery date | Owner |
|---|---|---|
| 1. Invest a further £70 million to expand Long COVID treatment and rehabilitation | 21/22 | NHS England and NHS Improvement |
| 2. Invest £30 million in the rollout of an enhanced service for general practice to support patients in primary care | 21/22 | |
| 3. Publish information about waiting times of post-COVID assessment services to ensure transparency | September 2021 | |
| 4. Evaluate post-COVID Assessment Clinics to obtain the lessons learned from set up | Ongoing | |
| 5. Ongoing review of the Long COVID clinical pathway to reflect the latest research evidence and operational experience | Ongoing | |
| 6. Extend the use of the Your COVID Recovery online rehabilitation platform | August 2021 | |
| 7. Use data tools showing take up by gender, ethnicity and deprivation, against expected prevalence. | July 2021 | |
| 8. Partner with National Voices, Asthma UK/British Lung Foundation and other Voluntary, Community and Social Enterprise Sector organisations to engage with communities more likely to be impacted by health inequalities. | Summer 2021 | |
| 9. Appoint six Patient and Public Voice Partners to provide advice on lived experience to the programme | May 2021 | |
| 10. Carry out a Health Equity Audit to assess the degree to which we achieve our vision of equitable access, excellent experience and optimal outcomes for all communities. | Summer 2021 | |
| 11. To improve accessibility of information we will ensure ‘easy read’ and printed versions of Your COVID Recovery materials are accessible, and that translations in over 100 languages will be available. | August 2021 | |
| 12. Promote good clinical practice through the national learning network on Long COVID for healthcare professionals | Ongoing | |
| 13. Further develop resources on FutureNHS platform to provide educational materials and enable information sharing across healthcare organisations and staff | Ongoing | |
| 14. For NHS staff, comprehensive support for health and wellbeing including mental health hubs, rapid referral to services, local occupational health and online wellbeing resources will be available. | June 2021 | |
| 15. All local NHS systems will have submitted to NHS Regions, fully staffed Long COVID service plans covering the whole pathway from primary to specialist care | 12 July 2021 | Integrated Care Systems |
| 16. Local NHS systems will include planning to ramp up Your COVID Recovery supported patient-self management in their Long COVID service plans | July 2021 | |
| 17. Long COVID services will nominate care coordinators to manage complex cases | July 2021 | |
| 18. Develop standard rehabilitation pathway packages to treat the commonest symptoms of Long COVID | July 2021 | |
| 19. Establish 15 Post COVID assessment paediatric hubs across England | July 2021 | |
| 20. NHS Long COVID activity data on referral, assessments and waiting times for post-COVID assessment clinics and the onward patient journey including use of Your COVID Recovery will be published monthly | September 2021 | NHS England and NHS Improvement and NHS Digital |
| 21. A Long COVID digital code will be added to the psychological therapies Minimum Data Set. | Summer 2021 | |
| 22. A Long COVID registry for patients attending the Post COVID Assessment Clinic will be established | July 2021 |
1. What we know about Long COVID
Clinical case definition
Some people can experience ongoing symptoms following COVID-19 well after their initial infection. People of all ages and backgrounds, irrespective of the severity of initial infection, can experience Ongoing Symptomatic COVID-19 and Post COVID-19 Syndrome, also known as ‘Long COVID’.
Long COVID is a multi-system condition with a wide range of debilitating symptoms spanning fatigue, breathlessness, cough, chest pain, heart palpitations, fever, headache, muscle pain, gastrointestinal problems and loss of taste and smell. Many people with Long COVID may experience a range of psychological and cognitive symptoms such as depression, anxiety, post-traumatic stress disorder (PTSD) and ‘brain fog’ or other cognitive impairments, in addition to physical symptoms. This can also have a social impact. Symptoms can fluctuate and change over time. They are well recognised by people who are living with Long COVID and can have significant impacts on a person’s ability to carry out day-to-day activities and work.
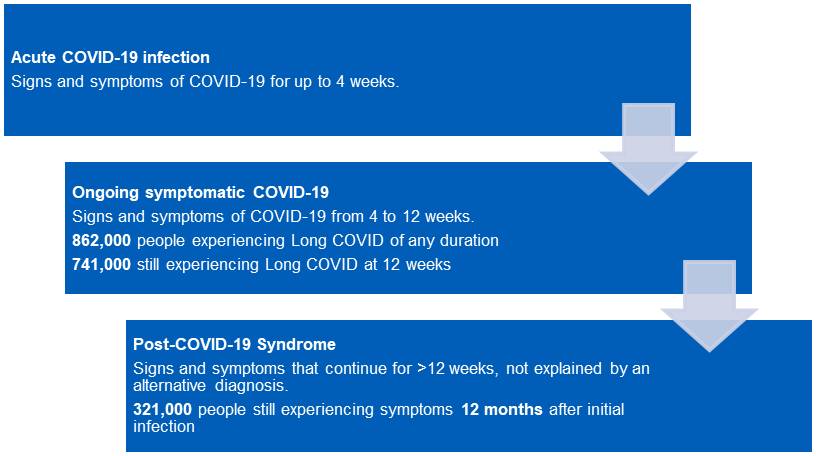
Recognising the importance of defining this emerging condition to enable diagnosis, NHS England commissioned the National Institute for Health and Care Excellence (NICE), which worked with the Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP), to produce a rapid guideline on managing the long-term effects of COVID-19. (NICE. COVID-19 rapid guideline: managing the long-term effects of COVID-19, December 2020.) This was first published in December 2020 and set out the following clinical definitions:
- Acute COVID-19: signs and symptoms of COVID-19 for up to 4 weeks.
- Ongoing symptomatic COVID-19: signs and symptoms of COVID-19 from 4 to 12 weeks.
- Post-COVID-19 syndrome: signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis.
“I’ve had an ongoing fever since the start of developing COVID and I have been left with extreme fatigue, difficulty concentrating (‘brain fog’), which worsens as fatigue sets in and poor short-term memory. I used to exercise regularly, but I have felt unable to since the infection, due to muscle pains mainly in my legs.”
SP – suffering from Long COVID
Emerging evidence
While we are still learning about this relatively new condition, there is growing evidence of the long-term effects of COVID-19 in those who were admitted to hospital with COVID-19. Results from the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) study (based on self-reporting from 325 people), found that half of participants reported feeling not fully recovered from COVID-19 (median follow-up 7 months). Fatigue was the most common symptom (77% of respondents), followed by shortness of breath (54% of respondents). Around a quarter reported a new disability in sight, walking, memory, self-care and/or communication, and overall, patients experienced a drop in quality of life. Studies also suggest that mental health problems may be common.
“There is a huge variety in the symptoms patients’ experience. The effects of this virus are variable and affect numerous different body systems. The two most striking symptoms we have seen are fatigue and breathlessness or breathing discomfort. The fatigue is extreme, relapsing and debilitating. The breathlessness is inconsistent, worrying for the patients and limiting. We regularly see people who were running marathons before they became unwell, now too fatigued and breathless to do their food shopping…. the psychological impact of such significant activity limitation is huge. We recognise the importance of treating patients’ mental health alongside their physical symptoms. Having investigations and a diagnosis is important for patients to accept, self-manage and begin to recover from their illness. Given the number of people struggling with these symptoms, our approach to management has had to be innovative and collaborative.”
Rebecca Livingstone, Senior Physiotherapist, University College London Hospitals NHS Trust
A study of 1,077 previously hospitalised patients, conducted by the PHOSP-COVID Collaborative Group, made similar findings, and identified four disease phenotypes with varying severities of physical, mental and cognitive health impairment.
Another study of over 47,000 individuals discharged from English hospitals following COVID-19, found they had elevated rates of multi-organ dysfunction compared with a matched control group. Post discharge adverse events included diabetes, major cardiovascular events and respiratory disease as well as increased risk of readmissions. Risk was greater for those who were less than 70 years old and from ethnic minority groups.
International research has similarly found evidence of long-term organ impairment following COVID-19 infection, with patients seen to have impaired lung function at six months post-infection, and persistent inflammation in the heart in some studies. (The Lancet, January 2021 and JAMA Network, July 2020.)
Long COVID can also occur in people who were never admitted to hospital and, in some cases, where initial symptoms were relatively mild. 862,000 people experiencing Long COVID of any duration in England, 741,000 are experiencing symptoms at 12 weeks after initial infection. The prevalence of Long COVID was higher in people aged 35-69, women, those from more deprived groups and amongst people with pre-existing health conditions. Health and social care workers had a higher prevalence of Long COVID.
Figure 1: Number of people with self-reported long COVID by duration, UK: 6 March 2021 and 2 May 2021
| Period | Duration | Estimate |
|---|---|---|
| Data to 6 March 2021 | Less than 12 weeks | 309 |
| At least 12 weeks | 697 | |
| At least 12 months | 70 | |
| Data to 2 May 2021 | Less than 12 weeks | 66 |
| At least 12 weeks | 869 | |
| At least 12 months | 376 |
Source: Office for National Statistics
Analysis of data from the COVID Symptom Study app (of over 4000 individuals) indicates Long COVID symptoms may fall into distinct groups and identified risk factors that may be associated with increased likelihood of developing Long COVID.
Some children and young people also appear to be affected by Long COVID. A study which followed up over 500 children (≤18 years old) previously hospitalised with COVID-19 found that a quarter had persistent symptoms >5 months after discharge, with fatigue (10.7%) and sleep disturbance (6.9%) being the most common. In another study, children reported prolonged symptoms such as insomnia, respiratory problems, fatigue, muscle pain, and concentration difficulties, and symptoms were also seen in those with asymptomatic acute infection.
“My symptoms varied a great deal at first and were very frightening. I was unable to walk more than fifteen metres, unable to empty a dishwasher or shower without intense chest pains, breathlessness and dizziness. The slightest effort wore me out. Improvement was painfully slow.”
Mike – experiencing symptoms after a year
A National Institute for Health Research (NIHR) review suggests that Long COVID may consist of a number of different syndromes, which could include post intensive care syndrome, post viral fatigue syndrome, long-term COVID syndrome and permanent organ damage. The report recommends that care should be stratified, and management should be joined-up across specialties and across primary, community and secondary care requiring a multi-professional workforce.
2. Expanding Long COVID treatment and rehabilitation services
NHS England and NHS Improvement will provide a further £70 million to expand Long COVID services beyond Post-COVID Assessment Clinics to strengthen diagnostics, treatment and rehabilitation for Long COVID. This is in addition to the £24 million already provided to 89 specialist Post-COVID Assessment Clinics around England, bringing the total investment in 2021/22 to £94 million. Additional funding will be allocated to Integrated Care Systems (ICSs) to ensure it goes to support the right services for diagnostics, treatment and rehabilitation, whether that be in a community, acute, mental health or tertiary care setting.
In April 2021 we published national commissioning guidance which can be found here. The guidance builds on feedback from service users, experiences of newly established clinics, NICE guidance and latest evidence, to map out a Long COVID clinical pathway, which can be found at the end of this section. It should act as a guide for commissioners, managers and clinicians in establishing services for Long COVID.
All ICSs are asked to provide fully staffed Long COVID service plans to regional teams covering the whole pathway from primary to specialist care by mid-July 20201, including for children. Plans should show how they meet the commissioning guidance, providing treatment and rehabilitation for people with Long COVID, and how they plan to maximise use of the Your COVID Recovery online rehabilitation platform for supported patient self-management.
Services must meet this core criteria:
- offer multidisciplinary, physical, cognitive, psychological and psychiatric assessments with the aim of providing consistent services and face-to-face appointments available where appropriate
- make provision for all those affected including those who were never admitted to hospital or tested for COVID-19
- services must ensure equity of access. Consideration must be given to groups most likely to be impacted by health inequalities and how they access and utilise healthcare services to ensure that no one is discouraged or unable to benefit.
Modelling demand
Some of those experiencing long term symptoms following COVID-19 will not need to seek NHS help, and others can be supported by their primary care team or in a community care setting. Others, however, will need specialist assessment and treatment. Working with an expert clinical reference group, a modelling assumption has been developed to estimate how many of these patients may require follow up in a Long COVID service. Figure 2 shows how this has been calculated.
Figure 2: NICE definitions with figures from ONS infection study and NHS England’s consensus model, numbers are approximate and high-level indications
There was clinical consensus that provisionally around 2.9% of people who had COVID-19 will go on to need NHS support: this is estimated to be around 342,000 people.
Early estimates of resources for follow up treatment and assessment at around 12 weeks after onset, include workforce and diagnostic costs for screening and triage into Post-COVID Assessment clinics for assessment and treatment, and further follow up with three broad levels of treatment intensity. Clinical feedback suggests that following initial clinic appointments:
- approximately 30-50% of patients could be appropriate for supported self-management (Tier 1)
- 18-30% could be treated in primary and community care (Tier 2)
- 20-50% could be followed up in specialist services and rehabilitation pathways (Tier 3).
Figure 3 provides an indicative visualisation of patient flow from triage to follow up treatment pathways, based on one potential clinical operating model, and for illustrative modelling purposes, assuming 160,000 patients require treatment in a specialist Long COVID service. It is based on information from three clinical reference sites in England and provides a guide for the flow of patients into and out of Post-COVID Assessment Clinics.
Figure 3 Indicative flow of patients with Long COVID symptoms
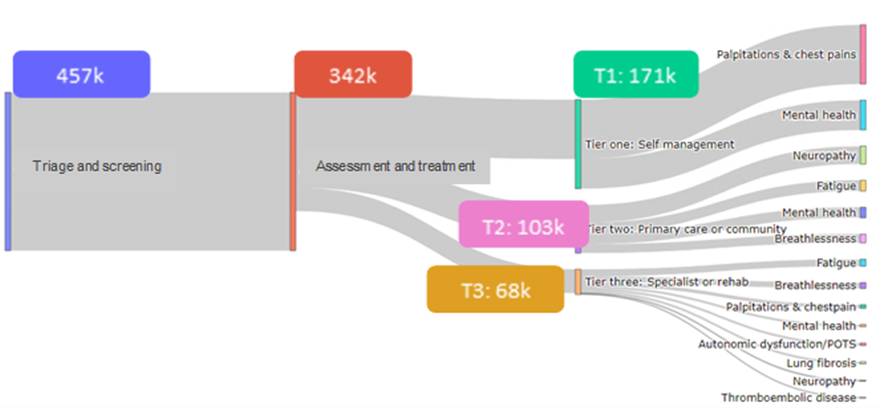
The above modelling relates to Post-COVID Assessment Clinics and follow up treatment and does not include patient pathways prior to 12 weeks after onset. Clinical feedback suggests much of the care provided prior to 12 weeks will happen in primary care although we know that a few may need to be referred from 4 weeks.
This, combined with the updated Post-COVID commissioning guidance and care pathway, will help ICSs to develop comprehensive Long COVID service plans, including provision for children and young people, by mid-July 2021.
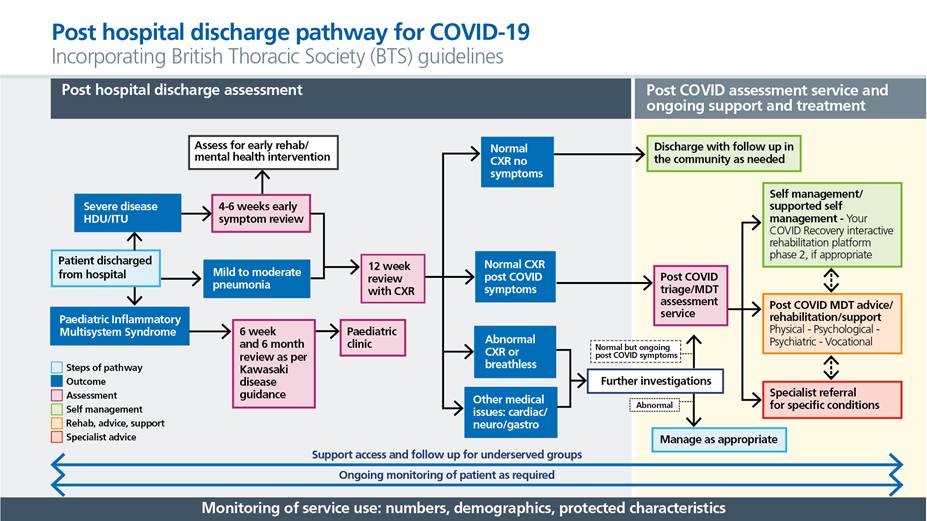
The care pathway
The two care pathways explained in Figures 4 and 5 have been developed in collaboration with commissioners, doctors, nurses, allied health professionals (AHPs) and people with lived experience of Long COVID. They are designed to help commissioners and providers plan and deliver joined up services spanning the whole care pathway. They include general practice, the wider primary care team, mental health services, rehabilitation services and acute hospitals as well as opportunities to signpost to the voluntary sector and local authorities.
Three principles of care for Long COVID
The care pathway for Long COVID has been designed around three core principles.
- Personalised care: By listening to people and asking, ‘what matters to you?’ a personalised care and support planning process based on what matters most to individuals is a crucial initial step in providing personalised care.
- Multidisciplinary and rehabilitation: A multidisciplinary team should tailor support and rehabilitation for the person to enable the development of individual care plans for physical, mental and social needs.
- Supporting and enabling self-care: Some people with milder symptoms may be able to help themselves through self-management.
The role of allied health professionals
Allied health professionals have a key role in the assessment, treatment and rehabilitation of people with Long COVID. These professionals, including physiotherapists, occupational therapists, clinical psychologists, dietitians and speech therapists, are a core component of the multidisciplinary team and are essential to support people with Long COVID to regain function. Utilising the workforce in an innovative way will be essential to optimise scope of practice and will include use of support staff, links to the voluntary sector and private providers, including those in the sports and leisure industry. The use of advanced practitioners in long term conditions rehabilitation pathways would provide leadership of such workforce models.
The role of pharmacists
Pharmacists can play an important role in the support of Long COVID patients in the community, general practice and in care homes.
Community pharmacists may be involved in public engagement and education, signposting people to support, providing any potential treatments and reaching underserved communities. Clinical pharmacists in primary care may also play a role in diagnosis and ongoing support.
Mental health pathway guidance
A significant proportion of people with Long-COVID are likely to experience problems in both physical and mental health, with the two interacting. When persistent mental health problems involve depression, anxiety or PTSD, a referral to IAPT should be considered, as Post-COVID MDT advice/rehabilitation/support element of the pathway. Referrals into other specialist mental health services must be considered with presentation of Serious Mental Illness in adults or for children and young people. Psychologists should be part of the multidisciplinary rehabilitation team, providing some individual input, group input and consultation to other staff.
To ensure integrated care for people experiencing depression, anxiety or PTSD as part of the Post-COVID MDT advice/rehabilitation/support element of the pathway, each system should create a pathway whereby IAPT works closely with other professionals involved in physical healthcare and rehabilitation. In many of the areas that already have an IAPT Long Term Condition (IAPT-LTC) service, the pathway for integrated working can build on the foundations and principles established through IAPT-LTC. However, in areas where IAPT-LTC does not yet exist, or is too small, existing resources in core IAPT, local clinical health psychology and physical specialist and rehabilitation pathways need to work together to create a pathway that provides the necessary integrated care and outcome monitoring for people with Long COVID.
Systems should also ensure links are in place between physical healthcare and other local specialist mental health services, which will be involved in supporting people with Serious Mental Illness or will form part of children and young people’s pathways.
In addition, to support with the cognitive impairment and difficulties in concentration or attention that are common with Long COVID, it will be important that multidisciplinary rehabilitation and treatment pathways include services to support with cognitive rehabilitation and stimulation, eg Memory Assessment Services.
Fatigue is one of the most common and disabling symptoms experienced by people with Long COVID and the pathway should provide access to a biopsychosocial approach to assessment and management of fatigue through primary, community and specialist rehabilitation services.
A Long COVID online training package has already been developed and rolled out for IAPT therapists and is available to others.
The role of nursing
Given the multi-faceted nature of Long COVID and the fact it may need to be managed as a long term condition, the nursing workforce will be key to supporting and coordinating the long term holistic clinical care of this group of patients.
Nursing teams should build education and knowledge to help assess, support and manage complex patients with Long COVID. Nursing also plays a critical role in the education of patients and families about Long COVID.
Development of specialist Long COVID nursing roles is an option for systems, to support Long COVID patients in primary and community settings. They will provide clinical capability, education and support into differing settings linking to primary and community care healthcare professionals.
We are committed to establishing networks to support nursing engagement and collaboration in this work – and for all healthcare professionals – as well as to support learning and sharing of good practice across the country.
Care coordination
To ensure timely and joined up care, which is prioritised based on clinical need, Long COVID services should identify care coordinators to help manage waiting lists and help patients navigate healthcare for, what are often, complex needs.
Figure 4: Primary and community care pathway for all ages
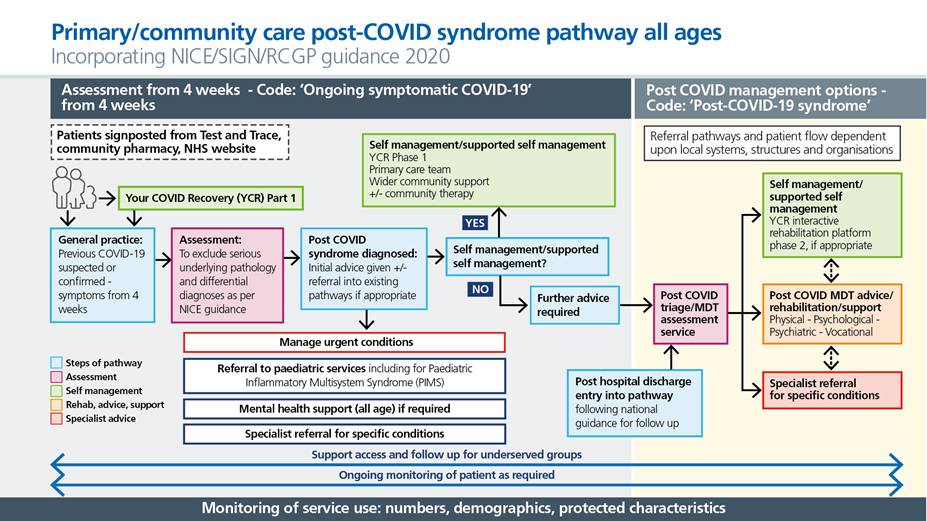
Figure 5: Post hospital discharge pathway (for patients who were admitted for or acquired acute COVID-19 infection)
Learning network
We have created a national learning network made up of 700 people involved in setting up and delivering Long COVID services around England. We will build on this to collate educational materials and spread good practice on diagnostics, treatment and rehab. The community includes a network for nurses working in community and for the wider NHS. A site on the FutureNHS platform has been developed to enable information sharing across healthcare organisations and staff and to make educational materials available. Supportive education and learning about the condition for healthcare professionals can be found on the Health Education England e-learning platform.
Actions
- NHS England and NHS Improvement will provide a further £70 million to expand Long COVID services beyond Post-COVID Assessment Clinics to strengthen treatment and rehabilitation for Long COVID. Additional funding will be provided to ICSs adding to the £24 million already provided to 89 specialist Post-COVID Assessment Clinics around England, bringing the total investment in 2021/22 to £94 million.
- Alongside this Long COVID Plan we have published the updated list of Post-COVID Assessment Clinics around England.
- By mid-July 2021 healthcare systems should provide fully staffed Long COVID service plans covering the whole pathway from primary care through to specialist care using multidisciplinary teams.
- Long COVID services should identify care coordinators by July 2021 to help manage waiting lists and help patients navigate healthcare for, what are often, complex needs.
- We will promote good clinical practice through the national learning network on Long COVID for healthcare professionals.
- We have developed a site on the FutureNHS platform to provide educational materials and enable information sharing across healthcare organisations and staff.
3. Enhancing general practice services to support patients with Long COVID
General practice plays a key role in supporting patients, both adults and children, with long term symptoms of COVID-19. This includes assessing, diagnosing, referring where necessary and longer-term holistic support of patients. If further complex investigations or support are required, the patient may be referred into a Post-COVID Assessment Clinic or other rehabilitation or support services.
This is a new and complex condition and will require professional education, consistent clinical coding of patients, planning of practice clinical pathways that will enable clinical management in primary care, where appropriate, and consideration of measures to reduce the risk of inequity of access to support. Therefore, we will offer an Enhanced Service to all GP practices.
Additional funding of £30 million will be available for practices that take up the Enhanced Service to plan their workforce set up, training needs and infrastructure to support patients with this new condition. This will be in addition to the funding already available to practices through global sum which reflects their core contractual responsibility for the provision of essential services to this cohort of patients.
This Enhanced Service will be for general practice to achieve the following objectives:
1) To increase knowledge on identifying, assessing, referring and supporting patients with Long COVID:
Education about the condition
- this is a new condition and ongoing education is required as learning evolves
- this may involve learning at different levels of expertise within the team
- different professionals in the team are likely to have different learning needs (for example, the role of the GP is likely to differ from the role of the social prescriber or the health and wellbeing coach)
- participation in educational sessions and sharing of learning with system partners (such as between specialist clinics and primary and community care) may be of benefit
- sharing of learning on national platforms may be of benefit.
Educational materials available to all healthcare workers can be found in the ‘Useful information’ section.
Knowledge of local pathways
- understanding local clinical pathways will be required to enable signposting or referring into appropriate pathways
2) To code and obtain data consistently and accurately to:
- enable learning about this new illness such as symptoms and the natural history
- obtain data, that can be cut by demographic, to understand which groups or communities are most affected and to identify potential inequities
- obtain activity data that can help to guide future service planning
Coding includes the following elements:- SNOMED codes as specified in national commissioning guidance, which include:
- Diagnosis code:
- Ongoing symptomatic COVID-19 (4-12 weeks after infection)
- Post-COVID-19 syndrome (12 weeks plus)
- Signposting and referral code:
- Signposting to Your COVID Recovery: when signposting patients to the publicly available Your COVID Recovery website (phase 1)
- Referral to post-COVID assessment clinic
- Resolution code:
- Post-COVID-19 syndrome resolved (available from May 2021): to be used at the patient and clinician discretion when all symptoms are fully resolved and there is no evidence of persisting organ impairment or if an alternative diagnosis has been made to account for all symptoms
- Diagnosis code:
- SNOMED codes as specified in national commissioning guidance, which include:
- coding of key clinical information in clinic letters from post-COVID assessment services or other specialist services
- continuing to code demographic information including ethnicity
3) To reduce inequity of access:
- By working with the practice Patient Participation Group (PPG) to help raise awareness of support (such as Your COVID Recovery website)
- By working with system partners to help raise awareness of support and understand any potential barriers to support
Participating general practices will submit a self-assessment confirming the above plans are in place.
Actions
- NHS England and NHS Improvement to invest £30 million in rollout of enhanced service for general practice
4. Long COVID in children and young people
The majority of children and young people (CYP) experience only mild symptoms following COVID-19 infection or are asymptomatic. However, there is evidence that some will experience Long COVID, and a minority of children may develop a delayed onset systemic inflammatory response known as Paediatric Inflammatory Multisystem Syndrome (PIMS-TS or PIMS) following COVID-19 infection. Symptoms of Long COVID are believed to be similar to those experienced by adults, although this needs to be understood more clearly. According to April 2021’s ONS estimates, around 7.4% of children 2-11 years and 8.2% of those aged 12-16 years report continued symptoms at 12 weeks after infection.
Clinical pathway for children and young people
Those with suspected Long COVID should be holistically assessed as early as possible to identify the need for specialist referral or ongoing therapeutic input, rehabilitation, psychological support, specialist investigation or treatment. They should be referred to existing services as needed and reviewed when appropriate.
The NHS will establish 15 Long COVID paediatric hubs across England in order to coordinate care for children and young people across a range of services. These specialist hubs will consist of multidisciplinary teams that can provide assessment services and remote support to other clinicians to ensure ongoing holistic support. Data collection from post-COVID assessment clinics has specific component for paediatric patients This will include advice to other clinicians on appropriate referrals. Considerations for assessment and treatment as follows:
- The impact of the illness on the child and family as a whole unit should be assessed.
- Be aware of wide-ranging, fluctuating symptoms that may change over time.
- Be aware of possible symptoms and signs suggestive of possible specific organ impairment such as chest pain, palpitations, breathlessness and symptoms or signs suggestive of possible ongoing inflammatory or autoimmune response, eg recurrent fever, rashes, joint symptoms, weight loss. These children may need specific investigations and timely discussion/referral to tertiary paediatric specialists.
- Consider alternate diagnoses for their symptoms.
- Consider transition services for young people aged over 16.
- Listen to concerns with empathy and acknowledge the impact of the illness.
- Discuss the child or young person’s experience of their symptoms and ask about any feelings of worry.
- As we provide care for children and young people with Long COVID we will gather evidence and work with NICE to potentially develop a case definition for children and young people.
Actions
- ICSs to establish 15 paediatric hubs to coordinate and advise on care for children with Long COVID across a range of appropriate services by July 2021.
5. Rehabilitation to manage the most common Long COVID symptoms
Long COVID has highlighted the importance of rehabilitation services in the treatment of chronic conditions. Feedback from clinicians indicates that the commonest symptoms of Long COVID are those that are most amenable to rehabilitation therapies. Prevalence of Long COVID is highest in working age adults (25-69), 29% of all those reporting symptoms report that their ability to undertake their day-day activities is significantly impacted.
Appropriate and personalised rehabilitation will have a beneficial impact on people’s lives and their recovery. Existing rehabilitation services in well integrated systems are best placed to provide this, especially integrated, multidisciplinary rehabilitation services, which include access to vocational rehabilitation to support return to occupation/work, with liaison where appropriate with the person’s employer.
People with Long COVID can often experience a multitude of complex conditions, once assessed in a Long COVID assessment service, those identified as being in this category should be assigned a care coordinator to help manage their progression through the pathway.
The recently published commissioning guidance includes a rehabilitation pathway for people with Long COVID. The purpose of rehabilitation pathways for people with Long COVID is to improve physical, psychological and cognitive outcomes. Pathways should be developed based on the principles in the RightCare: Community Rehabilitation Toolkit.
“Long COVID rehabilitation consists of a twice weekly, six-week programme of exercise and education which includes both strength and aerobic exercises. Topics discussed as part of the education are based on the information provided on the Your COVID Recovery website. The programme is delivered by the multidisciplinary team and tailored to individuals as community and hospital cases often present differently.”
Leicester Long COVID Service
Actions
- Local NHS systems should include a rehabilitation pathway programme in their Long COVID service plans due mid-July 2021. It should be based on the principles in the RightCare: Community Rehabilitation Toolkit.
6. Extending the use of the Long COVID self-management digital tool
Due to the range of Long COVID symptoms and their chronic nature, supported self-care is an important part of managing the condition, where this is clinically appropriate. We are working with experts to collate information, advice, support and referral to ensure people with Long COVID have reliable information, access to support and referral when it is required. People with Long COVID should not be excluded from the same level of support offered by these tools if they don’t have access to or literacy with digital technology.
Your COVID Recovery
Your COVID Recovery, a website containing support, advice, and information was launched in summer 2020 and has now had over 1.5 million visits. It is designed to help individuals recover from COVID-19 and manage the effects both on their body and mind effectively, reducing the impact it has on their day-to-day life.
Your COVID Recovery also provides a personalised and tailored package of modules covering topics such as fatigue and breathlessness management and nutritional advice for use by patients following a clinical consultation, under the supervision of a clinician. Individuals are encouraged to set goals and choose the resources that may help them to achieve their targets.
The website is being expanded to allow anyone with symptoms to access a range of symptom management advice without needing a referral from a clinician. There are also other digital tools being used by the NHS to support people with Long COVID.
Many patients are benefiting from the Your COVID Recovery online rehabilitation platform which enables self-management with the support of a clinician. Approximately 20% of Long COVID patients seen in clinics will have follow up treatment via digital rehabilitation platforms: 10% supervised treatment via Your COVID Recovery, and 10% self-managing with digital app support.
Actions
- From August 2021 further symptom management advice will be available on the Your COVID Recovery website.
- Local NHS systems should include planning to ramp up Your COVID Recovery supported patient-self management in their Long COVID service plans due by mid-July 2021.
- To improve accessibility of information, we will ensure ‘easy read’ and printed versions of Your COVID Recovery materials are accessible and translations in over 100 languages will be available from August 2021.
7. Improving data quality and transparency
Long COVID is a new condition about which little is known, so collecting data is critical to advance understanding of the prevalence, nature and course of the disease, and which treatments and pathways work. Data is required to understand demand for services, equity of access to services, and potential areas of unmet need, to support service planning, delivery and evaluation.
Since the 5-point plan…
Activity data is being regularly collected from the 89 Post-COVID Assessment Clinics, on the numbers of patients being referred, assessed and onward referral patterns. This data collection provides insight into health access and inequalities and performance of the Post-COVID Assessment Clinics.
NHS England and NHS Improvement has worked with NHSX, NHS Digital, and the Professional Records Standards Body (PRSB) to develop clinical coding to record Long COVID care in clinical information systems in primary and secondary care. This includes new SNOMED CT codes and a Treatment Function Code for post-COVID-19 syndrome services. Guidance on clinical coding in primary care and post-COVID assessment clinics has also been developed and shared. Establishment of clinical coding will enable improved and automated collection of data about Long COVID. In addition, a Long COVID code has been added to the IAPT Minimum Data Set, so NHS England, in collaboration with NHS Digital, will be able to report the mental health outcomes of everyone with Long COVID who is treated in IAPT. This will help ensure consistent quality across regions and maximise learning. As data quality from the Post-COVID Assessment Clinics improves we will begin to make it available publicly.
Long COVID Registry
To understand the longitudinal journey of people with Long COVID and needs for services, NHS England and NHS Improvement will develop a patient registry based on data linkage across national data collections. This will support operational, clinical and research activities, and, importantly, enable a more granular understanding of healthcare access for those groups who experience health inequalities.
Actions
- From September 2021 NHS England and NHS Improvement will publish data from the Post-COVID Assessment Clinics on referral, number of assessments, waiting times and the onward patient journey, including use of Your COVID Recovery, monthly. This will include take up by age, sex, ethnicity and deprivation.
- NHS England and NHS Improvement will develop a Long COVID registry for patients attending the Post-COVID Assessment Clinic by July 2021.
- NHS England and NHS Improvement will continue to promote and facilitate uptake of appropriate clinical coding for Long COVID care in primary care and post-COVID assessment clinics.
- A Long COVID digital code will be added to the psychological therapies Minimum Data Set in Summer 2021.
- Over the next year NHS England and NHS Improvement will evaluate Post-COVID Assessment Clinics to capture the lessons learned from set up.
8. Focus on equity of access, outcomes and experience
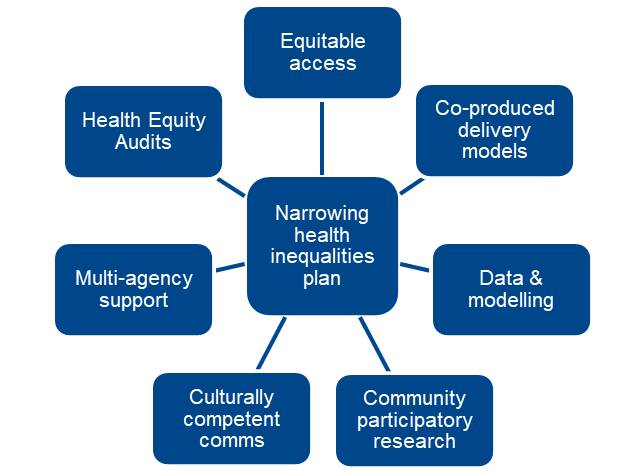
COVID-19 disproportionately affects those groups already experiencing health inequalities in terms of rates of infection and severity of acute infection, for example ethnic minorities.* We are still learning more about the impact of Long COVID on health inequalities, however the condition has the potential to further exacerbate existing inequality through chronic illness and the implications of this for people’s lives and livelihoods as well as health outcomes. We have an opportunity to create a joined-up approach to addressing health inequalities in access, experience and outcomes to Long COVID services, from the beginning – learning from the experiences of the COVID vaccination programme. We will focus on:
- Understanding the need: Driving the consistent recording of ethnicity, deprivation, disability and existing multimorbidity. Five of the 12 questions are core fields in assessment clinics data collection. Bringing data together from various sources, working with partners to ensure we are serving the needs of all groups. The ONS has made available data which will help us understand how Long COVID impacts different groups of people, including by gender, age, ethnicity and deprivation. We will match our data with ONS data.
- Better access: Improving equitable access to information on Long COVID, initial clinical assessment, specialist treatment, ongoing support. This will be addressed through educational materials for healthcare workers (particularly in general practice) and the public. We will further develop support materials like the Your COVID Recovery website into paper-based manuals, for those who do not access information online, and into other languages, for those whose first language is not English along with providing information in an accessible format such as easy read.
- Co-design and co-production with people with lived experience: We will broaden our engagement with people with lived experience to include diverse voices and perspectives at national, system and local level. This should inform design and delivery of services.
- Participatory research: Working with NIHR, we commit to ensuring a focus on engagement in relation to the Long COVID research, crucially that the participant group is diverse and reflective of population served.
- Culturally competent communications: Long COVID communications need to be aware of healthcare disparities and the impact of socio-cultural factors on health. Codesign and coproduction will enable more culturally competent communications.
- Multiagency support: A critical component of the clinical pathway, at local and system level the voluntary sector and local authorities must be involved in taking a holistic approach to physical, mental and cognitive health alongside employment, care needs and housing. Community pharmacy is a point of access, and social prescribing is a vital tool to achieve this. We will work with National Voices and Asthma UK/British Lung Foundation to join up with non-NHS services.
*Disparities in the risks and outcomes of COVID-19, Public Health England, August 2020
Figure 6 Matrix for narrowing health inequalities for Long COVID
Actions
- Building on the invaluable input to date of patient advocacy groups, six Patient and Public Voice Partners have been appointed to work with the Long COVID programme from May 2021.
- Your COVID Recovery information will be available in over 100 languages and printed manuals that replicate online content will be made available
- Over the next year we will partner with National Voices, Asthma UK/British Lung Foundation and other VCSE organisations to meaningfully engage with communities most likely to be impacted by health inequalities and align with VCSE work.
- We will carry out a Health Equity Audit to assess the degree to which we achieve our vision of equitable access, excellent experience and optimal outcomes for all communities.
9. Supporting NHS staff with Long COVID
Feedback from the Post-COVID Assessment Clinics suggests that a significant proportion of those accessing them are healthcare staff and ONS data shows high prevalence rates of Long COVID among health and social care workers compared to those working in other sectors. Healthcare staff may have been disproportionately affected by Long COVID and it is important that the NHS role models its approach as a responsible and supportive employer and takes care of staff who have worked so hard throughout the COVID-19 pandemic.
A comprehensive package for health and wellbeing has been put in place to support NHS staff as part of NHS recovery planning:
- 40 mental health hubs have been established to give staff rapid access to the care pathway.
- Enhanced occupational health and wellbeing pilots are in place in systems covering 700,000 staff.
- Staff can access occupational health teams, either on site or remotely, with onward rapid referral to other services where needed
- Direct access to a suite of national services to support wellbeing such as apps, a helpline, e-learning resources. These will augment local health and wellbeing support services
- As part of the national health and well-being offer, training for line managers and teams will be provided to enable individual health and wellbeing conversations and plans for staff
As part of the establishment of the Post-COVID Assessment Clinics, rapid access to these services for NHS staff via occupational health or GP referral is being explored. In addition, information will be made available to NHS employers about Long COVID and how to support staff experiencing it. The Faculty of Occupational Medicine has produced Guidance for healthcare professionals on return to work for patients with long-COVID and Guidance for managers and employers on return to work for employees with long-COVID.
“I am now on day 285 of Long COVID and whilst I consider myself lucky to have survived, I have been left with many ongoing health issues for which there seems to be no ‘cure’. My life is unrecognisable from before and I struggle to navigate the every day.”
Orli, a nurse who cared for COVID-19 patients
Actions
- A comprehensive package of health and wellbeing support has been extended from June 2021, for staff as part of the COVID-19 pandemic response and NHS recovery.
Useful information
NHS.uk website information on Long COVID
https://www.nhs.uk/conditions/coronavirus-COVID-19/long-term-effects-of-coronavirus-long-COVID/Nhs.uk
NHS England and NHS Improvement website information on Long COVID
https://www.england.nhs.uk/coronavirus/post-COVID-syndrome-long-COVID/
NICE COVID-19 rapid guideline: managing the long-term effects of COVID-19
https://www.nice.org.uk/guidance/ng188
Your COVID Recovery
https://www.yourCOVIDrecovery.nhs.uk/
National Institute of Health Research – Funded research into COVID-19
https://www.nihr.ac.uk/researchers/manage-your-funding/funded-research-into-COVID-19.htm
Royal College of General Practitioners – Resources for GPs
https://elearning.rcgp.org.uk/mod/page/view.php?id=11512&_ga=2.14873968.711735455.1615980427-643992121.1603279467
Health Education England – Knowledge and library Long COVID page
https://library.nhs.uk/long-COVID/
Patient safety learning resource
Post COVID-19 syndrome: What support can patients expect from their GP?
The Faculty of Occupational Medicine has produced guidance for return to work for patients with long-COVID
https://www.fom.ac.uk/media-events/publications/fom-guidance
