Minimising nosocomial infections in the NHS: Letter from Amanda Pritchard, Ruth May and Professor Stephen Powis
Contents
To:
Chief Executives and Chief Operating Officers of all NHS Trusts and Foundation Trusts
CCG Accountable Officers
Copy to:
GP practices and Primary Care Networks
Community pharmacies
Dental providers
Optometry providers
Providers of community health services
NHS 111 providers
NHS Trust Medical and Nursing Directors
NHS Trust Directors of Human Resources and Organisational Development
Chairs of ICSs and STPs
NHSEI Regional Directors
9 June 2020
Minimising nosocomial infections in the NHS
Dear colleague
Thank you to you and your teams for all the incredible work you have done in our response to COVID-19, while maintaining critical services and now the challenging task of restarting mainstream NHS services. We must take further action to tackle infections acquired in the NHS itself, whether staff, visitors or patients.
You will be aware that the Government launched the NHS Test and Trace service last week to minimise community transmission of COVID-19. It is designed to ensure that anyone who develops symptoms can quickly be tested to find out if they have the virus and, if they do, to trace close recent contacts who will be notified that they should self-isolate at home for 14 days.
If a member of staff develops symptoms of COVID-19 they should follow the stay at home guidance, and get tested as soon as possible. If the result is negative, the advice from Public Health England states that they “can return to work when they are medically fit to do so, following discussion with their line manager and appropriate local risk assessment. Interpret negative results with caution together with clinical assessment.” If they test positive, they can return to work after seven days, unless they still have symptoms other than a cough or loss of sense of smell/taste, in which case they must continue to self-isolate until they feel better.
Where a member of NHS staff tests positive for coronavirus, the starting point is that the Test and Trace self-isolation rules apply as anywhere else, and close contacts must self-isolate if the NHS test and trace service advises them to do so. Close contact excludes circumstances where PPE is being worn in accordance with current guidance on infection, prevention and control.
In other circumstances, i.e. where a member of staff has come into contact outside work with someone who has subsequently tested positive for coronavirus, NHS staff are subject to the same test and trace protocols as all other members of the public. If a healthcare professional or another member of your team is contacted by the Test and Trace service and advised to self-isolate for 14 days, they must do so.
We recognise this may be challenging, but it is an important part of our collective response to the pandemic. It is therefore vital to ensure that NHS organisations have robust processes in place to support the timely reporting and management of COVID-19 outbreaks, hospital acquired infection and associated staff absence.
This letter sets out specific actions that NHS organisations should take in these areas. It builds on the immediate response to support the mitigation of these impacts that has already been circulated through normal incident routes.
A. Test and Trace
All NHS organisations are asked to read and follow the latest guidance on Test and Trace.
All trusts are asked to take the following actions:
- Ensure that all daily COVID-19 sitrep data is accurate information, including the additional sections on length of time in hospital before a positive test result, and reporting staff absent because of COVID-19 (illness or self-isolation) and within that, the subset who are self-isolating for 14 days because they have been notified, by the Test and Trace service, as having been in close contact with someone who has tested positive for COVID-19. They should also report in the sitrep where staff absence has resulted in service disruptions, cancellations, etc.
- Each organisation must identify a point of contact for staff contacted by Test and Trace who have been advised to self-isolate, this point of contact should operate for a minimum of 16 hours each day.
- To prepare for potential staff absence, organisations should review their existing business continuity plans and take actions as required.
- Where as a consequence of reduced staffing organisations are considering temporary service reductions (part or all) they should discuss with the Regional Incident Coordination Centre without delay and implement appropriate business continuity measures or mutual aid. The Regional Team will notify the National Incident Coordination Centre.
All primary care contractors (GPs, pharmacists, dentists and optometrists) are asked to take the following actions:
- To prepare for potential staff absence, providers should review their existing business continuity plans and take actions as required. This includes ensuring that arrangements are in place within a primary care network or between buddies to maintain patient access to services.
- Providers should inform their commissioner as soon as they consider that delivery of the full contracted service may be compromised by staff absence due to Test and Trace. The commissioner will work with the contractor to put business continuity arrangements in place and to maintain access to services for patients. The provider will need to update information on patient accessible websites and the impacted NHS 111 Directory of Services profiles will need to be updated.
- The commissioner will inform the Regional Incident Coordination Centre without delay and work with the provider to implement appropriate business continuity measures. The Regional Team will notify the National Incident Coordination Centre.
In addition, Public Health England has launched SIREN, a new large-scale study to improve understanding of COVID-19 immunity and reinfection. Trusts will be asked to use their PCR and serology capability to monitor a cohort of healthcare workers fortnightly for up to 18 months for the purposes of this study. SIREN is aiming to determine whether a detectable antibody response protects against future infection in the short and medium term, which will help inform the public health response to COVID-19.
B. Management of outbreaks
Ongoing and consistent implementation of national infection prevention and control guidance, including in staff areas, will be paramount in reducing healthcare associated infections. This includes all staff adhering to social distancing (2 metres) wherever possible in non-clinical areas. Close contact between staff over prolonged periods should be minimised; for example, by avoiding congregating at central work stations, restricting the number of staff on ward rounds, conducting handover sessions in a setting where there is space for social distancing, moving to ‘virtual’ multi-disciplinary team meetings, and considering staggering staff breaks to limit the density of healthcare workers in specific areas.
Social distancing measures, where possible, are a critical part of maintaining IPC in clinical and non-clinical areas. However, where it isn’t always possible to maintain social distancing, public health advice is that wearing a face covering is an appropriate precautionary measure. As announced by the Secretary of State for Health and Social Care, from the 15 June, the recommendation will be that all staff in hospital wear a surgical face mask when not in PPE or in a part of the facility that is COVID-secure in line with the workplace definition set by the government. The guidance will also apply to other NHS healthcare settings, including primary care, and will be published this week by Public Health England. We therefore ask that you make the necessary changes to implement that advice and help reduce any further risks of transmission, by 15 June at the latest.
To support this, trusts should continue to use additional available NHS testing capacity to routinely and strategically test asymptomatic frontline staff. Local health systems should work together with their labs and regions to agree the use of available capacity. NHS labs should also be aiming to turnaround all COVID-19 tests within 24 hours, to ensure swift action can be taken to minimise the risk of nosocomial transmission and improve operational efficiency.
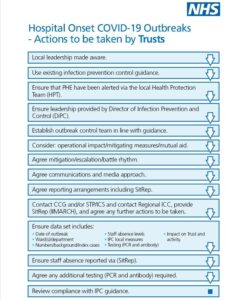
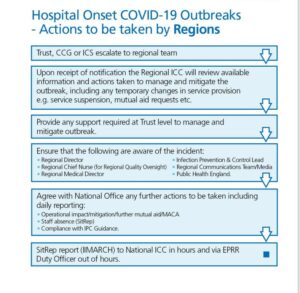
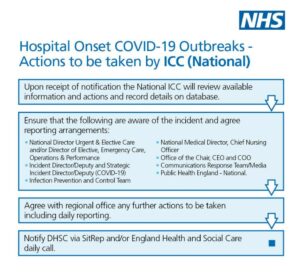
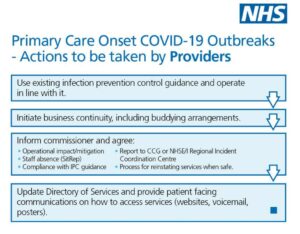
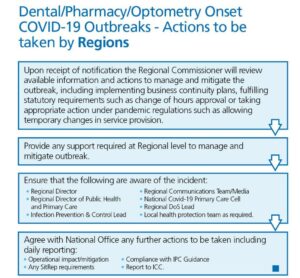
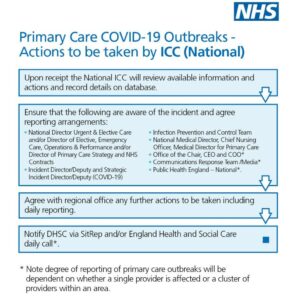
In the event of a COVID-19 outbreak, NHS organisations should continue to follow existing Public Health England guidance on defining and managing communicable disease outbreaks. To support the effective management of COVID-19 outbreaks at local, regional and national level we are making some changes to existing reports to ensure the impact of outbreaks is captured. Our regional teams are already working with local systems to develop standard ways of responding to these outbreaks. Appended are some high-level flowcharts of these processes, which can be adapted for local use where these are not already in place. We have also shared examples of good practice between regions.
To enable the local and national monitoring of outbreaks it is essential that the information you submit is correct. In addition to the COVID-19 sitrep mentioned above, please also ensure the accuracy of other data submitted, crucially including that correct patient postcode information is provided alongside test result data.
We hope that this letter helps to clarify the steps which organisations should be taking to minimise nosocomial infections, protect staff and ensure the timely reporting and management of outbreaks and staff absence in the NHS. We are extremely grateful for your ongoing support during this challenging time.
Yours sincerely
Amanda Pritchard | Chief Operating Officer | NHS England and NHS Improvement
Ruth May | Chief Nursing Officer | NHS England and NHS Improvement
Professor Stephen Powis | National Medical Director | NHS England and NHS Improvement