New national NHS England and NHS Improvement/Independent sector contract for Q4 2021/22
Contents
- New National NHS England and NHS Improvement / Independent sector Contract for Q4 2021/22
- Appendix – activating surge
Classification: Official
Publication approval reference: C1537
To:
- ICS and STP leads
- NHS trust and foundation trust:
- Chief executives
- Medical directors
- Finance directors
- CCG:
- Accountable officers
- Medical directors
- Finance directors
cc.
- NHS regional directors
- NHS regional directors of commissioning
- Regional finance directors
- Regional medical directors
10 January 2022
Dear colleague
New National NHS England and NHS Improvement / Independent sector Contract for Q4 2021/22
Following the letter (ref C1487) to the system on 13 December 2021 declaring a Level 4 National Incident, NHS England and NHS Improvement (NHSEI), under direction from the Secretary of State, has agreed a new national contract for Q4 with multiple independent sector providers (ISP).
The purpose of the arrangement is to ensure that as many people as possible can continue to get the planned care they need. It also importantly provides additional potential surge capacity if Covid threatens the NHS’s ability to provide urgent care. For the term of this contract ISP facilities and staff will be on standby to support the NHS at short notice should the Omicron variant lead to unsustainable levels of hospitalisations or staff absences.
This letter sets out what the new national contract means for systems and ISPs.
This national contract will be in place from Monday 10 January 2022 until 31 March 2022. For this period it replaces local CCG contracts and Trust sub-contracts with those ISPs sites that have been included in the arrangements.
The contract is made up of two parts – pre-surge and surge.
In pre-surge the contract continues to enable systems and Trusts to work with the ISPs to undertake elective work. This includes allowing NHS hospitals to send a wider range of patients to the ISPs for some forms of cancer surgery and other care, not normally delivered under existing arrangements, through priority tariff uplifts.
If ISP surge capacity were to be needed, the contract is designed to enable systems to make flexible use of independent sector facilities and staff. This would be triggered at short notice and as a last resort in the event that a local NHS system faced unsustainable levels of hospitalisations or staff absences.
Surge status will only be invoked for an individual NHS provider or system when:
- there is insufficient bed capacity to support the continued treatment of urgent/P1/P2 elective or cancer procedures
- staffing absence reaches levels that present a significant clinical risk to patient safety
- there is insufficient critical care capacity to support Covid activity
It is recognised that some surge triggers may operate differently within systems or regions reflecting variation in local services. Overarching surge thresholds have been set in the above areas. In the event that any of the thresholds are breached, and as a consequence the system is unable to continue to provide safe and appropriate clinical care, this will trigger a surge conversation between NHSE, the relevant region and system ISPs. However, for staffing it is recognised that patient safety is of paramount importance, so where there is significant clinical risk of patient safety being jeopardised due to staffing absences, surge may require triggering below the threshold.
During surge routine services at an ISP site will be suspended to make facilities and staff available to the NHS system. Entry into surge will be approved by the national NHSEI IS SRO with a clear process set out to trigger and manage use of surge arrangements, including high thresholds and evidence for demonstrating that surge is required. Systems in surge should regularly review the de-escalation criteria to ensure that it is still appropriate for the system to remain in surge. De-escalation from surge will also require approval from the national NHSEI IS SRO.
ISP surge capacity is to be used in extremis. Our priority remains for systems and Trusts to continue working locally with ISPs over the coming weeks and months to maintain non-Covid related NHS services within those green pathway sites. To support this, payments to ISPs will continue to be made by NHS systems and Trusts to facilitate optimal use of ISPs locally. Further detailed financial guidance on the pricing and funding of the arrangements will follow in the next few days.
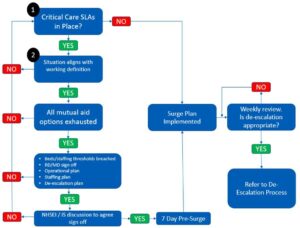
Key principles and criteria for surge activation and de-escalation are provided in the Appendix.
Yours sincerely
Sir David Sloman | Chief Operating Officer | NHS England and NHS Improvement
Julian Kelly | Chief Financial Officer | NHS England and NHS Improvement
Appendix – activating surge
Working definition
Surge status will only be invoked when an individual NHS provider or system faces unsustainable levels of hospitalisations or staff absences as a result of Covid pressures and as a result:
- there is insufficient bed capacity to support the continued treatment of urgent/P1/P2 elective or cancer procedures
- staffing absence reaches levels that present a significant clinical risk to patient safety
- there is insufficient critical care capacity to support Covid activity
Key principles
Surge is automatically invoked if any Critical Care Service Level Agreement between the ISP and an NHS Trust in that STP/ICS is terminated.
While some surge triggers may be different within systems or regions reflecting variation in local services. The thresholds after which a request for surge will be considered are:
- Trust core bed occupancy >=98%
- Trust Covid occupancy >=35%
- Trust ACC Occupancy >=85%
- Trust Clinical Staff absence rate >=20%*
*(lower absence levels may be applicable if areas can demonstrate material impact on single staff groups or disciplines)
Regions activating surge will require sign off from the national NHSEI IS SRO. Requests for surge activation will only be accepted when accompanied by:
- Regional Director approval.
- Confirmation of clinical sign off at regional level (Regional Medical Director).
- Evidence/confirmation agreed system criteria/thresholds have been breached.
- Detailed operational/staffing plans, jointly agreed between the NHS and ISP. Plans must include detail on intention of use (medical bed or green pathway provision), and de-escalation.
- Use of ISP for general medical patients is outside the scope of services specified in the contract, except in peak surge, and then only by prior mutual consent between the ISP Medical Director and the local NHS lead. Before being agreed they will need to make sure that the requested medical services can be provided to a safe standard in the relevant facilities. Even in surge, the ISPs cannot provide care for Covid infected patients requiring high dependency respiratory support.
Activating surge: Checklist for NHSEI sign off
Scenario 1
If the critical care / transfer out SLA between the NHS provider and ISP has been terminated and no alternative NHS provider has been found within 3 days, surge will be signed off by NHSE without further evidence.
Scenario 2
NHS provider or system is facing unsustainable levels of hospitalisations or staff absences. Regions will be asked to evidence the following:
- Breach of the overarching thresholds
- The region is satisfied the situation meets the working definition for surge
- Regional Director signed off system request for surge
- Regional Medical Director sign off
- Other routes for mutual aid within the region have been explored
- Locally agreed thresholds have been met
- There is a clear operational plan describing planned utilisation/intention for ISP capacity
- There is a staffing plan that outlines how NHS staff will be deployed into ISP sites
- There is a clear plan for de-escalation from surge
- Discussion with relevant local IS providers has taken place to ensure that all options for securing additional IS capacity have taken place
De-escalating surge: Overview
Regions and STPs/ICSs in surge should regularly review the de-escalation criteria to ensure that it is still appropriate for the system to remain in surge. This could be either pre planned through the formal surge reviews, or unplanned/urgent when the agreed surge arrangements do not materialise as planned.
All systems are required to develop a transition plan from current surge arrangements. This plan should be developed collaboratively between the NHS and IS, and must include repatriation of all staff, equipment and hosted services.
When a system de-escalates from surge, the national expectation is that the system returns to capacity infrastructure in line with levels prior to surge being activated.
Regions de-escalating surge will require sign off from the national NHSEI IS SRO.
Requests for surge de-escalation will require evidence/confirmation specific criteria/thresholds have returned to pre-surge levels and reversed any breaches of the overarching thresholds.
Once the decision to de-escalate has been made, a surge de-escalation notification will be issued by the PMO on the Friday of that week. This will trigger the notice period for activity to return to the Q4 non surge planned activity. Existing bookings should be honoured unless alternative arrangements are agreed.
De-escalating surge: Checklist for NHSEI sign off
Scenario 1
If the previously terminated Transfer out /critical care SLA between the NHS provider and ISP has been reinstated, de-escalation of surge will be signed off by NHSEI without further evidence.
Scenario 2
Reinstatement of elective care delivery by the NHS system will require regions to evidence the following:
- Regional director signed off system request for de-escalating surge
- Engagement with relevant ISPs has taken place to agree a clear operational plan (including repatriation of all patients, staff, equipment and hosted services) and timescales to de-escalate
- Overarching thresholds have been resolved and are below the surge trigger levels
- Assessment of clinical risk and safety implications have taken place ahead of the de-escalation