Novel coronavirus (COVID-19) standard operating procedure: resource shortage, escalation and National Loan Programme for COVID-19 in England
Contents
- Purpose
- Core principles
- System requirements
- National Loan Equipment allocation action steps (urgent clinical need)
- Definitions
- Decision sequence for bidding for allocation of ventilators or equipment
- Next steps
- Operating process for distributing nationally sourced equipment in England
Classification: Official
Publications approval reference: 001559 / C0709
Novel coronavirus (COVID-19) standard operating procedure: resource shortage, escalation and National Loan Programme for COVID-19 in England
For use when resources are being allocated on the basis of urgent clinical need
1 September 2020, Version 2
This guidance is correct at the time of publishing. However, as it is subject to updates, please use the hyperlinks to confirm the information you are disseminating to the public is accurate. Updates to Version 1, published on 7 April 2020, are highlighted in yellow.
Purpose
Describe the mechanism for hospital trusts in England to escalate capacity-limiting shortages to regional and national incident co-ordination teams. It is applicable during periods of the COVID-19 pandemic response in which resources are being allocated on an urgent clinical need basis.
Core principles
- Trusts will surge across England at different times.
- Trusts will hit a limit of ‘true capacity and capability’ to accept and manage
COVID-19 patients depending on ‘rate limiting factors’. - These rate limiting factors are dynamic and may be overt such as staff, hardware (ventilators, consumables, syringe drivers, NG feed pumps, filters, circuits or medications), or overarching service-critical supplies (oxygen).
- Trusts should have explored the following before submitting request to National Ventilator Application Panel (NVAP):
- local arrangements of re-allocating staff, equipment or transfer of patients
- regionally co-ordinated, flexible mutual aid arrangements within existing local/regional critical care networks.
System requirements
Must be based on the latest NHS regional capacity plans and demand modelling:
- Constant review of accurate real time data captured from all critical care-capable sites to give a local, regional and national overview of ‘true capacity’; including established and surge potential and utilisation.
- Data collated in a central data integration platform rolled out to regional and national decision makers to identify and respond.
- Ventilators and non-invasive ventilation (NIV)/continuous positive airway pressure (CPAP) machines as a top priority, recognising dependence on other equipment.
- Allow regional/national decision makers to allocate scarce resource optimally and dynamically with a clear audit trail and governance structure.
- Ensure receipt of equipment is confirmed by the receiving trust, and that it is tagged and tracked.
National Loan Equipment allocation action steps (urgent clinical need)
| Action | Responsible team | |
| 1 | Complete COVID-19 daily sitrep of baseline established capacity to manage O, O+ and V patients | Hospital trust |
| 2 | Report in COVID-19 sitrep current capacity *surge plan and **super-surge capacity for NIV/CPAP and IPPV considering:
|
Hospital trust |
| 3 | Interrogate justification for additional equipment and check alignment with regional surge plan | Host region |
| 4 | If required, exploit within region mutual aid options:
|
Host region (adjacent region) |
| 5 | If unresolvable or insufficient mitigation at regional level, then escalate to National Ventilator (equipment) Loan Panel for prioritisation and potential allocation of national loan stock. | |
Definitions
Baseline ventilator capacity
Invasive mechanical ventilators (located in critical care units) and non-invasive ventilation (NIV) machines (located in critical care/high dependency settings or designated wards).
*Surge ventilator capacity
Operating theatre, anaesthetic room and recovery area ventilators (including radiology, day surgery, independent sector, etc) not required for emergency or prioritised surgery (eg urgent cancer or obstetric).
**Super-surge ventilator capacity
Additional staffed bed capacity in any location for which additional ventilators and other equipment would be required to enable operation.
Note 1 – CPAP is the primary mode of non-invasive ventilation in COVID-19, unless the patient has (prior) type 2 respiratory failure.
Note 2 – Many critical care ventilators can also do CPAP/NIV: care required to not count these types of machines twice.
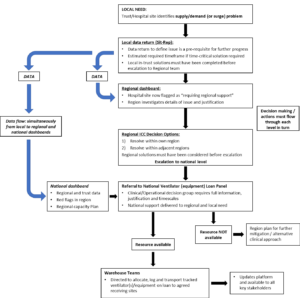
Decision sequence for bidding for allocation of ventilators or equipment
(Actions linked to table above)
Stage 1
[Table actions 1 and 2]
- Baseline data collected as per current data streams (daily situation report and other data requests) which inform capacity status, bids and decision making.
- Collect 12-hourly through critical care network within all V, O+ and O beds and surge beds.
- Return data collection through regional/national data platform as available.
Stage 2
[Table actions 3 and 4]
Information from Stage 1 checked and, in co-ordination with regional team, used to determine operational matching response – including:
-
-
- relocating ventilators, NIV machines and associated equipment from other hospital sites within region
- moving patients between hospitals within region (or to adjacent region)
- ambulance diverts, changing ambulance service catchment area.
-
Stage 3
[Table action 4]
- Meeting of key decision makers informed by Stages 1 to 2 at regional level with trust input as required. Feed into place mitigation and response plans.
Stage 4
[Table action 5]
If unresolved at regional level, referral to National Loan (equipment) Panel with full information and justification (bid to be submitted onto NHS Foundry by regional lead). Plan for further mitigation/alternative clinical approach if no national option available.
Next steps
- Local, regional and national supply leads to adopt this method of decision making as single route of escalation.
- Leads need to be familiar with and trained on planning tools and associated data capture methods to be introduced.
- Assess suitability of decision model for other equipment shortages.
Ventilator/NIV/CPAP-shortage escalation and loan protocol COVID-19
Operating process for distributing nationally sourced equipment in England
NHS trust/region submission process
- Trusts need to provide to the regional lead the name of their trust, contact person at that trust, and address of the trust to which allocations, if made, should be communicated and delivered. Trusts must confirm capability and detail for receipt 24 hours a day at the trust if required. Denial of delivery is not acceptable.
- Regional lead teams submit Resource Loan Request form on the NHS Foundry platform by 14.00hrs. In the event of any issues, send email to: england.covid-oxygen@nhs.net, copying in England.Covid19-oxygen-ventilator-delivery@nhs.net.
Urgent clinical need loan stock allocation process
- NVAP national support team list items available in stock and create forward view of future items to be presented at 15.00hrs NVAP session:
- NVAP decision on allocation recorded on NHS Foundry
- email sent by Oxygen and Ventilator Programme PMO to: NHS regional leads, SPOC and regional director, and copied to the assignment team England.Covid19-oxygen-ventilator-delivery@nhs.net
- assignment team confirm makes and models, collect delivery details and send instructions to warehouse teams.
- Warehouse teams:
- log serial number on dispatch against actual destination</mark
- deliver items to delivery addresses provided; typically the day following the NVAP meeting at which the loan request was approved.
- Notifications go out to trusts of expected contents and arrival time-window (including manufacturer and model details). Ensure out-of-hours reception arrangements if required.
On trust receiving site
Confirmation of delivery and receipt collected via signed proof of delivery. Proof of delivery forms will be validated with receiving trusts on a weekly basis.
- Trust accepts responsibility to track and retain equipment within their organisation and be prepared to release loan stock for redistribution of stockpiling at later date when requested by national or regional team.
- Trust pre-arranges prompt commissioning of device(s) by Medical Engineering.
- Trusts record appropriately on asset registers as loan etc.
Subsequent movements
- Regional teams are responsible for understanding all movements of National Loan Stock equipment between trust sites – so that locations are known if equipment needs to be returned.
- If equipment moves, regional team must notify nhsi.covido2ventproject@nhs.net including clearly identifying which items have moved, including serial numbers.
Retrieval and redistribution of loan stock
- At the point where a regional team or trust identifies that National Loan Stock is no longer required, the equipment should be fully decontaminated and the returning organisation contact england.ventilatorpackqueries@nhs.net.
- On receipt of the email the Returns Team will provide all required forms to enable the nominated collection service to undertake pick up of the equipment and return to the main National Loan Stock.