Second Phase Of NHS Response to COVID-19
Contents
To:
Chief executives of all NHS trusts and foundation trusts
CCG Accountable Officers
GP practices and Primary Care Networks
Providers of community health services
NHS 111 providers
Copy to:
NHS Regional Directors
Chairs of ICSs and STPs
Chairs of NHS trusts, foundation trusts and CCG governing bodies
Local authority chief executives and directors of adult social care
Chairs of Local Resilience Forums
29 April 2020
Dear Colleague,
IMPORTANT – FOR ACTION – SECOND PHASE OF NHS RESPONSE TO COVID19
We are writing to thank you and your teams for everything you have achieved and are doing in securing the remarkable NHS response to the greatest global health emergency in our history.
On 30th January the first phase of the NHS’s preparation and response to Covid19 was triggered with the declaration of a Level 4 National Incident. Then in the light of the latest SAGE advice and Government decisions, on 17th March we wrote to initiate what has been the fastest and most far reaching repurposing of NHS services, staffing and capacity in our 72-year history.
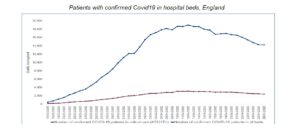
This has enabled us in the space of the past six weeks to go from looking after zero such patients to caring for 19,000 confirmed Covid19-positive inpatients per day, many of whom have needed rapidly expanded critical care support. Alongside this, the majority of patients the Health Service has continued to look after have been receiving care for other important health conditions. Despite real concern going in to the pandemic – following difficult international experience – every coronavirus patient needing hospital care, including ventilation, has been able to receive it.
This has largely been possible as a result of the unparalleled commitment and flexibility of NHS staff, combined with the public’s ‘social distancing’ which remains in place to cut the spread of the virus. We have also been greatly strengthened by over 10,000 returning health professionals; 27,000 student nurses, doctors and other health professionals starting their NHS careers early; 607,000 NHS volunteers; and the work of our partners in local government, social care, the military, the voluntary sector, hospices, and the private sector.
Sadly coronavirus looks set to be with the us for some time to come, so we will need continuing vigilance. We are, however, now coming through this peak of hospitalisations, as seen by the drop of nearly 5,000 in the daily number of confirmed Covid19-positive patients in hospitals across England over the past fortnight.
As the Prime Minister set out on Monday, we are therefore now entering the second phase in the NHS’s response. We continue to be in a Level 4 National Incident with all the altered operating disciplines that requires. NHS organisations therefore need to fully retain their EPRR incident coordination functions given the uncertainty and ongoing need. The purpose of this letter is to set out the broad operating environment and approach that we will all be working within over the coming weeks.
Based on advice from SAGE, we still expect to be looking after several thousand Covid19-positive patients, though hopefully with continuing weekly decreases. This means:
- Ongoing and consistent application of PHE/NHS Infection Prevention and Control guidance in all NHS organisations, with appropriate cohorting of Covid/non-Covid patients (https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control).
- In response to the global shortage, DHSC and the Cabinet Office together with BEIS (for UK manufacture) and DIT (for international suppliers) continue to expand the sourcing and procurement of HSE/PHE-recommended PPE for the NHS, social care and other affected sectors of the UK economy, but it is likely that current Covid-specific logistics and distribution arrangements will need to continue for the time being.
- Increased lab capacity now enables testing of all non-elective inpatients at point of admission, the introduction of pre-admission testing of all elective patients, testing prior to discharge to a care home, as well as expanded testing for staff. The corollary is the operational importance of fast turnaround times for test result reporting.
The pressure on many of our staff will remain unprecedented, and they will need enhanced and active support from their NHS employers to ensure their wellbeing and safety.
- Increased testing capacity means that we will now be able to extend the offer of regular testing to asymptomatic staff, guided by PHE and clinical advice. This approach is being piloted in a number of acute, community and mental health providers this week, which will inform further roll out from next week.
- As set out in our letter of 17th March, NHS organisations should continue to assess staff who may be at increased risk – including older colleagues, pregnant women, returnees, and those with underlying health conditions – and make adjustments including working remotely or in a lower risk area. Educational material, training and appropriate protection should be inclusive and accessible for our whole workforce, including our non-clinical colleagues such as cleaners and porters.
- Emerging UK and international data suggest that people from Black, Asian and Minority Ethnic (BAME) backgrounds are also being disproportionately affected by Covid19. Public Health England have been asked by DHSC to investigate this. In advance of their report and guidance, on a precautionary basis we recommend employers should risk-assess staff at potentially greater risk and make appropriate arrangements accordingly.
- Now more than ever a safety and learning culture is vital. All our staff should feel able to raise concerns safely. Local Freedom to Speak Up Guardians are able to provide guidance and support with this for any concerned member of staff. As we know, diverse and inclusive teams make better decisions, including in the Covid19 response.
- Employers are also asked to complete the process of employment offers, induction and any necessary top-up training within the next fortnight for all prospective ‘returners’ who have been notified to them.
We are going to see increased demand for Covid19 aftercare and support in community health services, primary care, and mental health. Community health services will need to support the increase in patients who have recovered from Covid and who having been discharged from hospital need ongoing health support. High priority actions for mental health providers in this next phase are set out in the Annex. General practice will need to continue to stratify and proactively contact their high-risk patients with ongoing care needs, including those in the ‘shielding’ cohort to ensure they are accessing needed care and are receiving their medications.
Given the scale of the challenges they face, we must also continue to partner with local authorities and Local Resilience Forums (LRFs) in providing mutual aid with our colleagues in social care, including care homes. This includes:
- Continuing to ensure that all patients safely and appropriately being discharged from hospital to a care home are first tested for Covid19; care homes can also check that these tests have been carried out.
- Under the direction of the LRF, local authority public health departments and CCG infection control nurses can help ‘train the trainers’ in care homes about PHE’s recommended approach to infection prevention and control – particularly focusing on those care homes that lack the infrastructure of the bigger regional and national chains.
- To further support care homes, the NHS will bring forward from October to May 2020 the national roll out of key elements of the primary and community health service-led Enhanced Health in Care Homes service. Further detail will be set out shortly.
- Opportunities to support care homes should also be provided to younger health professional ‘returnees’ and public volunteers who have offered to help (subject to appropriate personal risk assessment, as described above).
As also seen in a number of other countries, emergency activity has sharply reduced in recent weeks. Last week emergency hospital admissions were at 63% of their level in the same week last year. This is likely due to a combination of: a) changed healthcare seeking behaviour by patients, b) reductions in the incidence of some health problems such as major trauma and road traffic accidents, c) clinical judgements about the balance of risk between care in different settings, and d) some NHS care being provided through alternative access routes (eg ambulance ‘see and treat’, online appointments).
There is therefore considerable uncertainty as to the timing and extent of the likely rebound in emergency demand. To the extent it happens, non-elective patients will potentially reoccupy tens of thousands of hospital beds which have not had to be used for that purpose over the past month or so.
This means we need to retain our demonstrated ability to quickly repurpose and ‘surge’ capacity locally and regionally, should it be needed again. It will also be prudent, at least for the time being, to consider retaining extra capacity that has been brought on line – including access to independent hospitals and Nightingale hospitals. The national Nightingale team will work with Regions and host trusts to develop and assure regional proposals for the potential ongoing availability and function of the Nightingale Hospitals. Independent hospitals and diagnostics should be used for the remainder of the current contract which runs to the end of June. Please also start now to build a plan for each STP/ICS for the service type and activity volumes that you think could be needed beyond the end of June, which can inform discussions during May about possible contract extensions with the independent sector.
Over the next six weeks and beyond we have the opportunity to begin to release and redeploy some of the treatment capacity that could have been needed while the number of Covid19 patients was rising so sharply.
This means we are now asking all NHS local systems and organisations working with regional colleagues fully to step up non-Covid19 urgent services as soon as possible over the next six weeks, including those set out in the Annex. This needs to be a safe restart with full attention to infection prevention and control as the guiding principle.
In addition, you should now work across local systems and with your regional teams over the next 10 days to make judgements on whether you have further capacity for at least some routine non-urgent elective care. Provisional plans will need to factor-in the availability of associated medicines, PPE, blood, consumables, equipment and other needed supplies. We will continue to provide new ventilators to trusts over the coming weeks so as to sustain critical care ‘surge’ capacity should it again be needed in future, while progressively returning operating theatres and recovery suites to their normal use.
We should also take this opportunity to ‘lock in’ beneficial changes that we’ve collectively brought about in recent weeks. This includes backing local initiative and flexibility; enhanced local system working; strong clinical leadership; flexible and remote working where appropriate; and rapid scaling of new technology-enabled service delivery options such as digital consultations.
In terms of wider action that will also be underway, DHSC will be designing and establishing its new ‘Test, Track & Trace’ service. The leadership and resourcing of local authority public health departments will be vital. Trusts and primary care networks should continue to support clinicians to enrol patients in the three major phase III clinical trials now underway across the NHS, initially testing ten potential Covid19 treatments. In addition, at least 112 Covid19 vaccines are currently in development globally. We also expect an expanded winter flu vaccination campaign alongside a school immunisation ‘catch up programme’.
Looking forward, at the right time and following decision by Government, we will then need to move into the NHS’s phase three ‘recovery’ period for the balance of the 2020/21 financial year, and we will write further at that point.
In the meantime, please accept our personal thanks and support for the extraordinary way in which you and your staff have risen to this unprecedented global health challenge.
With best wishes,
Simon Stevens | NHS Chief Executive
Amanda Pritchard | NHS Chief Operating Officer
ANNEX
ACTIONS RECOMMENDED FOR URGENT CLINICAL SERVICES OVER THE NEXT SIX WEEKS
Urgent and routine surgery and care
- Strengthen 111 capacity and sustain appropriate ambulance services ‘hear and treat’ and ‘see and treat’ models. Increase the availability of booked appointments and open up new secondary care dispositions (SDEC, hot specialty clinic, frailty services) that allow patients to bypass the emergency department altogether where clinically appropriate.
- Provide local support to the new national NHS communications campaign encouraging people who should be seeking emergency or urgent care to contact their GP, go online to NHS 111 or call 999 if necessary.
- Provide urgent outpatient and diagnostic appointments (including direct access diagnostics available to GPs) at pre-Covid19 levels.
- Ensure that urgent and time-critical surgery and non-surgical procedures can be provided at pre-Covid19 levels of capacity. The Royal College of Surgeons has produced helpful advice on surgical prioritisation available at: (https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0221-specialty-guide-surgical-prioritisation-v1.pdf)
- In the absence of face-to-face visits, primary and secondary care clinicians should stratify and proactively contact their high risk patients to educate on specific symptoms/circumstances needing urgent hospital care, and ensure appropriate ongoing care plans are delivered.
- Solid organ transplant services should continue to operate in conjunction with the clinical guidance developed and published by NHS Blood and Transplant.
- Where additional capacity is available, restart routine electives, prioritising long waiters first. Make full use of all contracted independent sector hospital and diagnostic capacity.
- All NHS acute and community hospitals should ensure all admitted patients are assessed daily for discharge, against each of the Reasons to Reside; and that every patient who does not need to be in a hospital bed is included in a complete and timely Hospital Discharge List, to enable the community Discharge Service to achieve safe and appropriate same day discharge.
Cancer
- Providers have previously been asked to maintain access to essential cancer surgery and other treatment throughout the Covid19 pandemic, in line with guidance from the Academy of Medical Royal Colleges and the NHS (https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0239-Specialty-guide-Essential-Cancer-surgery-and-coronavirus-v1-70420.pdf and https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0239-Specialty-guide-Essential-Cancer-surgery-and-coronavirus-v1-70420.pdf ). An exception has been where clinicians consider that for an individual patient the risk of the procedure at the current time outweighs the benefit to the patient.
- Local systems and Cancer Alliances must continue to identify ring-fenced diagnostic and surgical capacity for cancer, and providers must protect and deliver cancer surgery and cancer treatment by ensuring that cancer surgery hubs are fully operational. Full use should be made of the available contracted independent sector hospital and diagnostic capacity locally and regionally. Regional cancer SROs must now provide assurance that these arrangements are in place everywhere.
- Referrals, diagnostics (including direct access diagnostics available to GPs) and treatment must be brought back to pre-pandemic levels at the earliest opportunity to minimise potential harm, and to reduce the scale of the post-pandemic surge in demand. Urgent action should be taken by hospitals to receive new two-week wait referrals and provide two-week wait outpatient and diagnostic appointments at pre-Covid19 levels in Covid19 protected hubs/environments.
- High priority BMT and CAR-T procedures should be able to continue, where critical care capacity is available.
Cardiovascular Disease, Heart Attacks and Stroke
- Hospitals to prioritise capacity for acute cardiac surgery, cardiology services for PCI and PPCI and interventional neuroradiology for mechanical thrombectomy.
- Secondary care to prioritise capacity for urgent arrhythmia services plus management of patients with severe heart failure and severe valve disease.
- Primary care clinicians to continue to identify and refer patients acutely to cardiac and stroke services which continue to operate throughout the Covid19 response.
- Hospitals to prioritise capacity for stroke services for admission to hyperacute and acute stroke units, for stroke thrombolysis and for mechanical thrombectomy.
Maternity
- Providers to make direct and regular contact with all women receiving antenatal and postnatal care, explaining how to access maternity services for scheduled and unscheduled care, emphasising the importance of sharing any concerns so that the maternity team can advise and reassure women of the best and safest place to receive care.
- Ensure obstetric units have appropriate staffing levels including anaesthetic cover.
Primary Care
- Ensure patients have clear information on how to access primary care services and are confident about making appointments (virtual or if appropriate, face-to-face) for current concerns.
- Complete work on implementing digital and video consultations, so that all patients and practices can benefit.
- Given the reduction of face-to-face visits, stratify and proactively contact their high-risk patients with ongoing care needs, to ensure appropriate ongoing care and support plans are delivered through multidisciplinary teams. In particular, proactively contact all those in the ‘shielding’ cohort of patients who are clinically extremely vulnerable to Covid19, ensure they know how to access care, are receiving their medications, and provide safe home visiting wherever clinically necessary.
- To further support care homes, the NHS will bring forward a package of support to care homes drawing on key components of the Enhanced Care in Care Homes service and delivered as a collaboration between community and general practice teams. This should include a weekly virtual ‘care home round’ of residents needing clinical support.
- Make two-week wait cancer, urgent and routine referrals to secondary care as normal, using ‘advice and guidance’ options where appropriate.
- Deliver as much routine and preventative work as can be provided safely including vaccinations immunisations, and screening.
Community Services
- Sustain the Hospital Discharge Service, working across secondary care and community providers in partnership with social care. Includes daily reviews of all patients in a hospital bed on the Hospital Discharge List; prompt and safe discharges when clinically and in line with infection control requirements with the planning of ongoing care needs arranged in people’s own homes; and making full use of available hospice care.
- Prepare to support the increase in patients who have recovered from Covid and who having been discharged from hospital need ongoing community health support.
- Essential community health services must continue to be provided, with other services phased back in wherever local capacity is available. Prioritise home visits where there is a child safeguarding concern.
Mental Health and Learning Disability/ Autism services
- Establish all-age open access crisis services and helplines and promote them locally working with partners such as local authorities, voluntary and community sector and 111 services.
- For existing patients known to mental health services, continue to ensure they are contacted proactively and supported. This will continue to be particularly important for those who have been recently discharged from inpatient services and those who are shielding.
- Ensure that children and young people continue to have access to mental health services, liaising with your local partners to ensure referral routes are understood, particularly where children and young people are not at school.
- Prepare for a possible longer-term increase in demand as a consequence of the pandemic, including by actively recruiting in line with the NHS Long Term Plan.
- Annual health checks for people with a learning disability should continue to be completed.
- Ensure enhanced psychological support is available for all NHS staff who need it.
- Ensure that you continue to take account of inequalities in access to mental health services, and in particular the needs of BAME communities.
- Care (Education) and Treatment Reviews should continue, using online/digital approaches.
Screening and Immunisations
- Ensure as a first priority that screening services continue to be available for the recognised highest risk groups, as identified in individual screening programmes.
- Increase the delivery of diagnostic pathways (including endoscopy) to catch up with the backlog of those already in an active screening pathway, followed by the rescheduling of any deferred appointments.
- Antenatal and Newborn Screening Services must be maintained because this is a time critical service.
- Providers and commissioners must maintain good vaccine uptake and coverage of immunisations. It is also likely that the Autumn/Winter flu immunisation programme will be substantially expanded this year, subject to DHSC decision shortly.
Reduce the risk of cross-infection and support the safe switch-on of services by scaling up the use of technology-enabled care - In response to Covid19, general practice has moved from carrying out c.90% of consultations with patients as face-to-face appointments to managing more than 85% of consultations remotely. 95% of practices now having video consultation capability live and the remaining few percent in the process of implementation or procurement of a solution. GP Practices should continue to triage patient contacts and to use online consultation so that patients can be directed to the most appropriate member of the practice team straight away, demand can be prioritised based on clinical need and greater convenience for patients can be maintained.
- Referral streaming of new outpatient referrals is important to ensure they are being managed in the most appropriate setting, and this should be coupled with Advice and Guidance provision, so that patients can avoid an outpatient referral if their primary care service can access specialist advice (usually via phone, video too).
- All NHS secondary care providers now have access to video consultation technology to deliver some clinical care without the need for in-person contact. As far as practicable, video or telephone appointments should be offered by default for all outpatient activity without a procedure, and unless there are clinical or patient choice reasons to change to replace with in-person contact. Trusts should use remote appointments – including video consultations – as a default to triage their elective backlog. They should implement a ‘patient initiated follow up’ approach for suitable appointments – providing patients the means of self-accessing services if required.
