Secondary care: document of preparedness
Contents
- Introduction
- Workforce
- Infrastructure
- Service reconfiguration
- Equipment
- Data and information management
- Communications
- Escalation procedure
- Appendix 1: Wellbeing information
- Appendix 2: Glossary of terms for infrastructure and estates
Publication approval reference: C0280
Secondary care: document of preparedness
11 April 2020
This is a live document that will be routinely updated. Please send any comments or local insight to England.covid-secondarycareDOP@nhs.net
1. Introduction
This guidance supports secondary care organisations to respond to the expected surge in inpatient demand due to COVID-19, supplementing local surge and escalation plans already in place. It is recognised that some trusts are already experiencing surge while others are in the preparation phase. For those reviewing their surge and escalation plans, this document can be used as a checklist.
The document acts as a reference point for secondary care organisations, bringing together existing publications, although is not intended to be exhaustive. For the duration of the COVID-19 pandemic, this document will support local decision-making processes and will be routinely updated to include the latest available guidance.
This document should be used by the chief executive’s designated accountable emergency officer when managing their organisation’s response to the COVID-19 pandemic. It is likely that sections of this document will be passed on to the relevant operational managers/executive leads within the organisation for review.
2. Workforce
This section is useful for the director of HR.
Decisions around the workforce should be locally determined, supported by national guidance and shared learning from other organisations and regions.
This chapter should be read in conjunction with Chapter 4: Service reconfiguration which, for some specialties, contains speciality-specific guidance on workforce issues.
The NHS Employers website and the workforce section of the NHS England and NHS Improvement website, should be routinely reviewed for updates regarding workforce issues during the COVID-19 pandemic.
NHS England and NHS Improvement have published guidance on deploying staff safely. This includes:
- principles for workforce redeployment
- profession-specific guidance for allied health professionals, dentists, doctors, healthcare scientists, nurses and midwives, pharmacists and pharmacy technicians and non-clinical staff
- expansion of the workforce: returners, students and volunteers
- regulation
- induction and training
- indemnity
Guidance on redeploying specific workforce groups
NHS England and NHS Improvement are developing a suite of guidance documents to support the redeployment of the secondary care workforce.
Examples of currently available guidance:
Redeploying your secondary care medical workforce safely
Adult critical care novel coronavirus (COVID-19) staffing framework
Deploying the healthcare science workforce to support the NHS clinical delivery plan for COVID-19
Advice regarding NHS volunteers relating to COVID-19
Staff wellbeing including protecting vulnerable staff
Staff wellbeing
Staff will likely be stretched beyond their usual working practices, impacting on wellbeing and staff morale. Local support systems should be developed as a priority and communicated to all staff. Trusts should also ensure that there are appropriate rest facilities for staff.
In conjunction with stakeholders, NHS Employers has facilitated the development of guidance on staff health, safety and wellbeing. This includes chapters on occupational health, vulnerable staff, fatigue and mental wellbeing. In addition, NHS England and NHS Improvement have released a suite of wellbeing guides to support the workforce.
Further useful resources on staff wellbeing can be found in Appendix 1.
Vulnerable staff
Individual staff circumstances including their current health and medical history should be considered in local decision-making.
In conjunction with stakeholders, NHS Employers has facilitated the development of guidance for identifying and redeploying vulnerable staff groups.
Infrastructure
This section is useful for the director of estates and facilities.
Secondary care trusts should optimise their infrastructure and estates in preparation for surge capacity during the COVID-19 outbreak. This chapter addresses issues specific to the additional requirements of the COVID-19 pandemic situation. It is not an exhaustive list for estates operational policy.
The following documents should continue to provide the reference points for the estates leads when considering the effect of increasing demand on all aspects of their infrastructure and estates operational policies. Where COVID-19 specific advice has been produced, this is noted.
Redesigning existing space for clinical use
When repurposing clinical areas, trusts should consider a common design layout where possible to aid staff productivity.
For guidelines on extending existing facilities to increase the inpatient bed capacity for adult inpatients (Level 1) please see the HBN 04 01. The HBN 04-01 Supplement on isolation facilities has also been published. (See Appendix 2 for glossary of terms).
For guidelines on extending existing facilities to increase the inpatient bed capacity (Level 2-3) please see the HBN 04 02, and the Estates and facilities COVID-19 SOP: design note. (See Appendix 2 for glossary of terms).
Coping with increased demand
Local resilience planning for infrastructure and estates should form part of overall hospital planning for the COVID-19 outbreak.
Existing Department of Health and Social Care (DHSC) guidance outlines best practice for waste management, including safe working practices. Some elements are more immediately relevant than others during the COVID-19 pandemic.
A COVID-19 standard operating procedure for waste is being produced. This will include details on how you should handle and consign waste, details of the national co-ordination cell, links to government advice and regulatory position statements/authorisations from relevant governing bodies: eg the Environment Agency and the Department for Transport.
Existing DHSC guidance on the design, installation, commissioning, testing, monitoring and operation of water supply systems in healthcare premises.
Existing DHSC advice regarding best practice for water management and efficiency in the healthcare sector. Some elements are more immediately relevant than others during the COVID-19 pandemic.
Electricity and electrical safety (including surge capacity)
Existing DHSC guidance containing information on the design, installation and testing of all fixed wiring and integral electrical equipment used for electrical services.
Existing DHSC guidance outlining the work and safety procedures for operation and management of low voltage electrical installations in healthcare premises.
Existing DHSC guidance covering safe systems of work and safety procedures for operation and management of high voltage (11Kv) electrical installations in healthcare premises.
Ventilation, air condition and heating (including areas being adapted or expanded for use of clinical activity)
Existing DHSC guidance on the design and management of heating and specialised ventilation in health sector buildings.
NHS England and NHS Improvement have published guidance on completing fire risk assessments for temporary wards providing COVID-19 care.
Existing guidance published by DHSC sets out its policy on fire safety in the NHS in England. It includes best practice guidance on management arrangements for fire safety.
Existing DHSC guidance on legislation and government policy with regards to fire safety in the design of healthcare premises.
Existing DHSC suite of guidance on fire safety measures for health sector premises.
Medical gases (including oxygen flow capacity)
Medical gases are medicines, and organisations’ pharmacy departments must be involved in dialogue around supply of and quality assurance of medical gases and medical gas pipeline systems.
Existing DHSC guidance can be found in two parts. Part A covers piped medical gases, medical and surgical air, and medical vacuum installations, and Part B covers operational management.
You should consider health and safety together with fire risks in an oxygen-enriched environment, where wards/clinical areas have increased use of piped or medical gas cylinder supplied oxygen. Cylinders must be safely moved and sited while being stored and while in use.
Existing DHSC document outlining the guidance on acoustic design for healthcare building development.
As announced, NHS organisations are expected to provide free parking to their staff for the duration of the COVID-19 pandemic.
Guidance for car-park management and sustainable transport is provided. Trusts are encouraged, where appropriate, to consider diverging from standard guidelines, in the interest of facilitating preparedness planning more broadly.
Estates planning for patients after death
Unfortunately, during this pandemic, organisations may have increased demand on their mortuary services. Trusts should complete the daily mortuary capacity statistics that will inform national planning around mortuary capacity being led by NHS England and NHS Improvement and DHSC. In the movement of bodies and storage of patients after death, dignity, privacy and confidentiality must always be respected and maintained. Guidance for the care of the deceased with suspected or confirmed COVID-19 has been published.
Additional elements, with guidance to follow
Estates and facilities workforce
NHS England and NHS Improvement are developing guidance on the estates and facilities workforce. The link to this guidance will be added to this document when published.
NHS England and NHS Improvement are developing guidance on catering. The link to this guidance will be added to this document when published.
4. Service reconfiguration
This section is useful for the director of strategy and transformation and the medical director/nursing director.
Rapid learning
NHS England and NHS Improvement have published learning from centres that have already experienced a surge in coronavirus cases. This will be routinely updated as learning emerges from more sites.
Specialty-specific guidance
NHS England and NHS Improvement are developing a suite of guidance documents to support the management of patients with specialty-specific presentations. This should be read in conjunction with guidance from Public Health England on diagnosis, management and testing of COVID-19 patients.
5. Equipment
This section is useful for the director of estates and facilities.
Secondary care trusts should ensure that procedures are in place to manage equipment availability in response to COVID-19. Essential equipment to consider throughout is personal protective equipment (PPE), infection control resources and respiratory support.
Procurement: Trusts should re-evaluate their delivery ordering schedules and minimum stock levels and adjust accordingly. This should be frequently reviewed by the procurement and materials management teams in partnership with clinicians.
For COVID-19 emergency ordering and failed orders, trusts should visit the COVID-19 section of the NHS Supply chain website. Non-NHS Supply Chain customers should e-mail details of their shortage to supplydisruptionservice@nhsbsa.nhs.uk or call 0800 915 9964 or 0191 283 6543.
PPE: Trusts should continue to work with suppliers to ensure a sufficient stock of PPE is maintained. Trusts can obtain information on their expected PPE push deliveries through the self-service section of the NHS Supply Chain website. This information should be considered when placing business-as-usual orders.
Stock and inventory: Stock availability should be assessed and recorded daily for each clinical area with the ability to share information regionally and nationally where required. Storage of stock should be organised and well-signposted to aid staff productivity. For information on ward-based consumables, click here.
National procurement and supply chains: Each trust should work directly with its internal procurement teams and use its existing supply chain network to meet the changing demands. Trusts should not stockpile locally. Supply chain ward information is here and suppliers are here. There are daily NHS supply chain customer update webinars, and trusts can register for these here.
Maintenance: There should be contingency plans for maintaining equipment (eg ventilators, blood gas machines). Information for maintenance, repair and calibration is here.
Clinical procedures: Clinical procedures should be organised to minimise aerosol droplet spread. Guidance on airway management is here. Pre-prepared packs and checklists should be used in accordance with infection control policies. Critical care preparation guidance is here.
Repurposing existing spaces: For newly repurposed clinical areas, preplanning of equipment requirements and their transport should be in place with the ability to monitor, communicate and transport equipment requirements in response to demand.
Trusts on split sites/neighbouring trusts: Equipment-sharing arrangements and robust pre-planned pathways to transport equipment between sites should be planned.
Sustainability: Processes to minimise theft and equipment misuse should be in place. Ensure minimal wastage of clinical and non-clinical items from all activity, including reuse where safe to do so.
6. Data and information management
This section is useful for the chief clinical information officer.
NHS England and NHS Improvement are only capturing data required to inform national decision-making by the NHS and government and communications to the general public.
Currently, information is being collected via the following platforms (in addition to the routine data collected by NHS England and NHS Improvement and NHS Digital):
- PHE’s COVID-19 positive test data
- daily situation reporting (sitreps)
- independent sector sitreps
- bed utilisation and PPE data
- supply chain data.
A national central system is being used to securely store the data to provide a population overview of COVID-19.
7. Communications
This section is useful for the director of communications.
In preparation for surge capacity during the COVID-19 outbreak, secondary care trusts should optimise their communication strategies to disseminate information to staff and patients. This should be done in a timely manner to ensure that the organisation is viewed as the most trusted and reliable source of information.
Trust communication teams should be central to the planning and delivery of the additional surge capacity. These teams will be supported regionally and nationally to ensure that communications are consistent and aligned. This will include template letters and messaging, which can be adapted for local needs.
NHS Employers has published guidance to support the communications process.
Internal communication
COVID-19 developments and latest guidance should be communicated to all staff in the hospital (clinical and administrative). This can be divided into the following:
Hospital-wide communication: Distribution of information to staff should be up to date, relevant and consistent. Staff should be signposted to wellbeing and mental health support.
Departmental communication: Staff should be briefed on how COVID-19 developments specifically apply to their department. This includes staff redeployment, departmental reorganisation, the designated service lead and patient safety escalation procedures. This is crucial to maintaining quality and safety of patient care.
Patient communication: It is the responsibility of all staff to educate and communicate to patients and their relatives the most up-to-date local COVID-19 hospital precautions to minimise risk to themselves and others.
External communication
Communication to the local community and stakeholders that the hospital serves should be consistent with public health and national messaging. Outpatients should be informed that elective and outpatient procedures will be postponed.
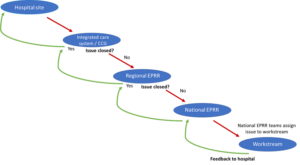
Escalation procedure
Trusts should ensure that their local major incident escalation procedures are robust, accounting for staff sickness.
Concerns including, but not limited to, workforce, infrastructure, estates or equipment should be escalated to the following:
- consultants/departmental leads/site managers should escalate internally
- accountable emergency officers/emergency planning officers/on-call directors/CEO/COO/CNO should escalate externally to the ICS/CCG and the regional emergency preparedness, resilience and response (EPRR) team.
The regional EPRR team will escalate unresolved issues to the national EPRR team. Responses are then fed back downstream.
Figure 1: Escalation procedure
Appendix 1: Wellbeing information
| Theme | Advice |
| General wellbeing support |
|
| Mental health and burnout | |
| Coping with stress | |
| Resources aimed at healthcare professionals | |
| Coping with coronavirus stigma | |
| Caring for children | CDC managing anxiety and stress (chapter on children). |
| If you live with a vulnerable family member, or a child with a vulnerable condition | |
| Individuals with existing mental health conditions | |
| Advice for team leaders or managers in a health facility | WHO: Mental Health Considerations During COVID-19 |
Appendix 2: Glossary of terms for infrastructure and estates
HTM: Health Technical Memoranda. These contain comprehensive advice and guidance on the design, installation and operation of specialised building and engineering technology used in the delivery of healthcare.
HBN: Health Building Notes. These are best practice guidance on the design and planning of new healthcare buildings and on the adaptation or extension of existing facilities.
CFPP: Choice Framework for Local Policy Procedures. Pilot initiatives that have now become HTMs.
HFN: Health Facilities Notes; superseded by HBNs.
MES: Model Engineering Specification; archived.
FPN: Fire Planning Notes; some remain active, some archived.
