Supporting CCGs to address vaccine inequalities – next steps
Contents
- Additional funding
- Annex A – Community funding evaluation framework
- Annex B – Funding application template
Classification: Official
Publication approval reference: C1217
To: CCG Accountable Officers
Cc:
- GP practices
- PCN leads
- LVSs
- ICS system leaders
- LAs
- Regional Directors of Commissioning
- Regional Directors of Commissioning/ Finance
19 March 2021
Dear colleagues
In our letter of 24 February, £4.2 million of funding was allocated to STPs to be used across constituent CCGs to support and enable locally led community engagement in all areas with health inequalities. We have heard about many excellent local approaches to engage with communities that have been historically underserved or that are not vaccine confident.
These include:
- In central Liverpool, a pop-up vaccination clinic was established at the Pakistan Multicultural Youth and Community Centre (aka the PAL centre). The vaccinators were medical students from ethnic minorities and faith and community leaders were engaged on-site.
- A vaccination bus that visited locations across Crawley to drive uptake in the Hindu community. This travelled to specific locations agreed through partnerships with the community to support increased confidence and outreach to vulnerable patients.
- In Winchester, for people experiencing homelessness and rough sleeping temporary vaccination clinics were held at several addresses acting as shelters for this high-risk group over two days. This saw 90% of those living at the night shelter vaccinated.
On Thursday 25 March from 12:00-12:45 we are hosting a webinar to showcase some of these local approaches and will be joined by Dr Habib Navi, Director NHS Race and Health Observatory who will outline some of the themes of effective approaches that are emerging across the country. You can register for the webinar here: https://www.events.england.nhs.uk/events/addressing-covid-19-vaccine-inequalities
Our thanks for your efforts to offer the opportunity for vaccination to all. The coming weeks allow the opportunity to refocus on ensuring that no one is left behind in cohorts 1-9.
Additional funding
CCGs were asked to develop plans in collaboration with the local community, agreed with local Directors of Public Health, detailing how the initial funding will be used and outline any additional longer-term strategic and systemic engagement required to address local needs. Regions should now assess these plans utilising the framework at Annex A as a starting point.
To support further local activity £3m of additional funding has now been made available, and from 26 March regions are invited to submit funding applications as sponsors for their CCGs. Applications from those areas that are assessed as having significant vaccine inequalities and that have not received community champion funding, that are novel or innovative approaches, or address an historically underserved community, will be prioritised. Applications will be assessed on a rolling basis and close once all allocated funding has been released. Applications should be made for around £100k-£150k with higher value applications considered under exceptional circumstances
A template is included at Annex B and should be submitted to england.vaccination-equalities@nhs.net. To keep this process rapid and responsive bids should be concise and adhere to the template requirements.
Alongside recently published guidance on Temporary vaccination clinic ‘pop-ups’ we are reviewing what further national guidance and frameworks would be helpful to support the development of local approaches.
Best wishes
Dr Nikita Kanani | Medical Director for Primary Care | NHS England and NHS Improvement
Dr Emily Lawson | NHS Chief Commercial Officer and SRO Vaccine Deployment | NHS England and NHS Improvement
Annex A – Community funding evaluation framework
CCG plans should be developed in collaboration with the local community, agreed with the local Directors of Public Health, and detail how they intend(ed) to utilise the initial funding and outline any additional longer-term strategic and systemic engagement required to address local needs. For guidance see “A guide to community-centred approaches for health and wellbeing” (Public Health England and NHS England (2015), accessed March 2021).
The following criteria should be utilised to assess the strength of local plans. The legacy impact of any interventions on addressing wider health inequalities should also form part of this evaluation. The six criteria should also be considered collectively as well as individually – for example, if the main source of lack of confidence was due to widespread misinformation, then these criteria could be considered together. The six criteria are:
- Removing barriers to access
- Reducing misinformation and disinformation
- Increasing vaccination confidence
- Cost of implementation
- Ease of implementation
- Increase in vaccination uptake
Removing Barriers to Access
Barriers to access should include both structural and systemic issues. As well as travel time and distance, physical accessibility, accessibility by public transport and availability of parking and availability of translators (including for BSL), planners should also be considering times of availability, staffing numbers, staff mix (by age, race and gender and ensuring diversity of the workforce which reflects the local community) and any other factors that might affect the accessibility of the service.
Reducing misinformation and disinformation
There is significant misinformation regarding coronavirus vaccinations being spread by social media, word of mouth, in publications, on fly posters and other media. This can impact vaccine confidence in groups that already lack confidence in government, the NHS, western healthcare or governmental services. Making information available to counter misinformation is vital, but the medium by which that information is disseminated is crucial. Trusted community leaders are potential advocates and schemes should seek to involve these individuals where relevant. This would include the use of faith leaders, community groups and other noted local people.
Increasing vaccination confidence
Whilst closely aligned to misinformation, confidence in underserved communities can be increased by addressing concerns about the effectiveness of the vaccine, side effects, new technology amongst others. Again, this needs to involve well researched information being made available through trusted routes, ensuring both messenger and messages are similar, clear and accessible.
Cost of implementation
The plan should be costed, and regions should assess value for money (NICE guidance on public health interventions may be a helpful reference*), including all the components of the plan such as staff costs, venue hire, equipment and so on. An evaluation analysis of effectiveness which compares the costs of alternative ways of producing the same or similar outputs could be considered.
*NICE (2013) “How NICE measures value for money in relation to public health interventions”, accessed March 2021.
Ease of implementation
The plan should be assessed against a range of factors including how quickly it can be implemented, how easy it is to source the required inputs and whether the initiative is sustainable over the period of vaccine distribution. This should not preclude development of complex approaches, with more challenging initiatives supported if they will have a high impact, especially in historically underserved communities or where vaccine uptake is low.
% increase in vaccination uptake
The plan should be assessed for its likely effectiveness in the targeted group(s), and the quantitative or qualitative data that can be gathered to support the measure of effectiveness in the targeted population.
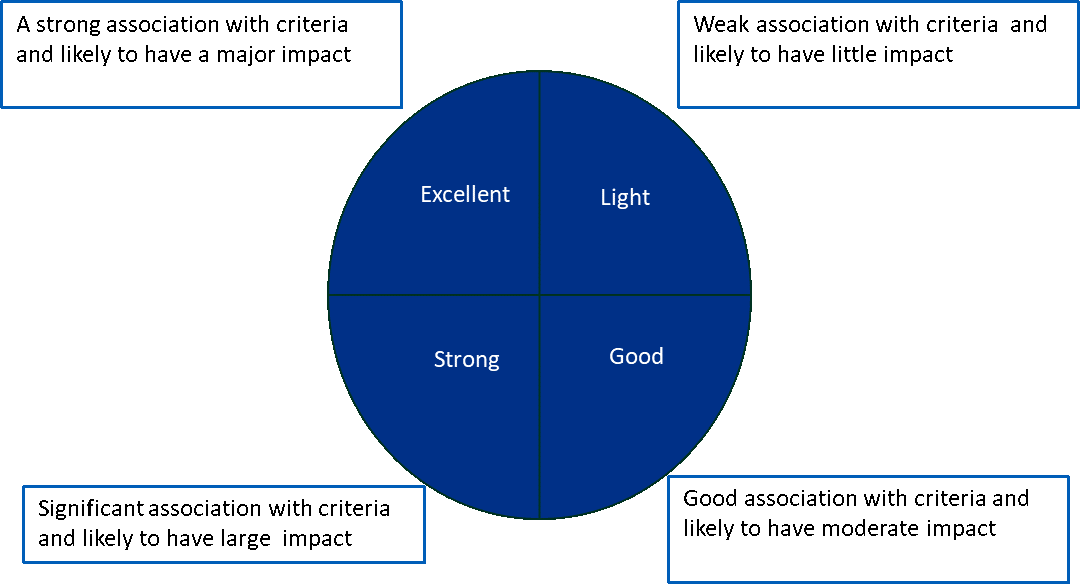
The diagram above gives some view on how the initiative should be assessed for each of the criteria above, with guidance below on questions that will inform the evaluation of those criteria.
1. Removing barriers to access
Structural and system i.e. staff capacity and attitudes
- Is the main purpose of this initiative to remove a structural or system barrier to access?
- What was/were the barriers are they specific to the locality?
- What was the mode of delivery utilized e.g. PoW, Community Centre etc?
2. Reducing mis and disinformation
- Is the main purpose of this initiative to reduce the spread of mis and/or disinformation?
- How was mis/disinformation being spread?
- Was it specific to the locality or a group?
3. Rising vaccination confidence – i.e. Trust
- Is the main or a significant focus of this initiative targeted at rising vaccination confidence?
- Is it targeted at a specific community – if so, which?
- Is it transferable to other communities?
4. Cost of implementation
- How much has it cost to implement (funding, staff)
- How sustainable is this investment (i.e. does it require ongoing funding to continue or a one-off initial investment?)
5. Ease of implementation
- How quickly was/can the initiative be deployed?
- How much was the ability to implementation reliant longstanding relationships?
- How easy is it to secure the resources required?
6. Percentage increase in vaccination uptake amongst EDI and inclusion groups
- What indications are there that the project is affecting uptake in the target group – can it or is it being measured?
- Is there data or qualitative feedback evidence?
Annex B – Funding application template
| CCG | |
| Named contact details (Name, email address) | |
| Please confirm Regional approval | |
| Region approver contact details (Name, email address) | |
| Expected start date of activity | |
| Expected end date (if available) | |
| Description of activity (750 words max)
To include summary of:
|
|
| Breakdown of cost
(Please specify separately any money to be used for admin/management, and any to be allocated to community/faith partners) |
|
| Expected total cost |
