Supporting CCGs to address vaccine inequalities
Contents
Official
Publication approval reference: C1158
To: CCG Accountable Officers
Cc:
- GP practices
- PCN leads
- LVSs
- ICS system leaders
- LAs
- Regional Directors of Commissioning
- Regional Directors of Commissioning Finance
24 February 2021
Dear colleagues
Thank you for the work you are doing to address vaccine inequalities in your area. This letter describes further national action to enable and locally deliver community activity and engagement to support COVID-19 vaccination access and uptake, building on the vaccine uptake strategy.
Our approach is influenced by three factors of vaccine hesitancy identified by the WHO: confidence, convenience and complacency and is intended to support local systems to intensify meaningful and respectful activity in their local communities to improve vaccine uptake and ensure health inclusion.
Emerging data shows differences in uptake rates within the first four JCVI priority cohorts, despite overall high level of vaccine confidence and approval in older age groups.
Initial data suggests that:
- Black African communities have the highest hesitancy compared to other ethnic groups
- Pakistani and Bangladeshi communities have higher hesitancy than White British/Irish and Indian communities
- Gypsy, Roma and Traveller communities, people experiencing homelessness and Asylum seeker, Refugee and migrant populations may need additional routes to access the vaccine
- Income and socio-economic circumstances correlate with lower levels of uptake
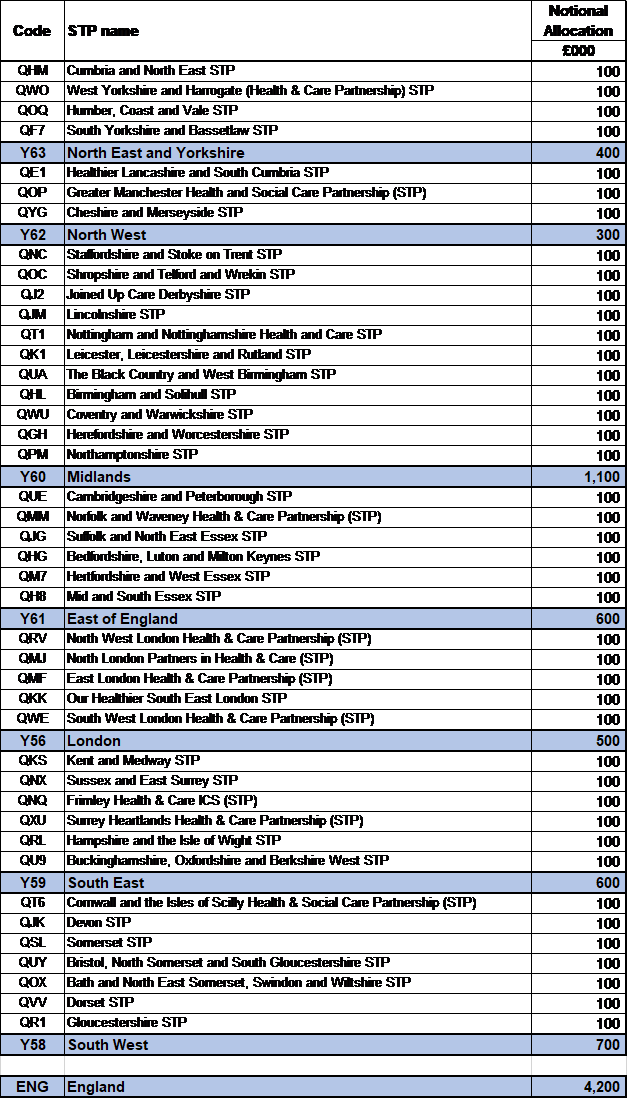
The COVID-19 vaccine deployment programme, working with partners, will make available an extra £4.2m of funding initially, to further support and enable locally led community engagement in all areas with health inequalities. Each STP will receive a notional allocation of £100k, to be used across its constituent CCGs (See Appendix I); the STP will determine how the funds will be shared between the CCGs, but we would expect the shares to take account of the relative health inequalities and existing sources of funding across the whole of the STP. This resource aims to complement the substantial investment made by the Ministry for Housing, Communities and Local Government to support community champions by offering a targeted resource to those systems that are performing poorest in vaccine uptake amongst ethnic minority communities. We expect that the best outcomes will come from working directly with local authorities and community organisations, building on their strong links into specific communities and effective communication tools.
Based on cohort penetration in cohorts 1 to 4, CCGs with low uptake in ethnic minority communities or low uptake in marginalised or deprived communities will be provided with data on vaccine uptake within their local PCNs and at a postcode level to support a focused and granular response to local challenges. The additional funding should seek to develop and deliver local solutions, and should be focused on intensifying existing or novel local engagement activity that focuses on one or all of the following:
Confidence (vaccine hesitancy)
a. Understanding the reasons for hesitancy, especially in BAME communities, and
b. Developing solutions for overcoming hesitancy, especially with BAME communities
Convenience (barriers to access)
c. Understanding the barriers to access, especially for health inclusion groups, and
d. Addressing, minimising or removing barriers, especially for health inclusion groups
Complacency
e. Understanding the reasons for complacency in certain groups, especially younger populations, and
f. Developing local solutions to support civic and individual responsibility, especially in younger populations
CCGs will be asked to develop a plan in collaboration with the local community, agreed with the local Director of Public Health, detailing how they intend to utilise the initial funding and outline any additional longer-term strategic and systemic engagement required to address local needs. These will be reviewed and evaluated by regions, with further monies released in March 2021 to support further implementation and delivery.
Resourcing approach
STPs should make plans to invest as required to i) support activity now to increase vaccine uptake, ii) support and intensify existing engagement activity, and ii) to support local systems to develop a plan for longer-term strategic and systematic engagement to address local need. CCGs should claim for costs actually incurred through the monthly claims process.
Measuring success
Regions and STPs have access to vaccine uptake data that can be split by ethnic minority background and deprivation. Directors of Public Health will also have access to patient level data. The progress and success of local approaches will be demonstrated by an increase in uptake among those communities that currently have low uptake, as described above.
Temporary vaccination clinics
Alongside this letter we are publishing details of how local vaccination services run by PCN groupings or community pharmacy can set up temporary vaccination clinics in community settings, including places of worship. This creates huge opportunity to make a tailored offer to communities that improves take-up.
Best wishes
Emily Lawson | NHS Chief Commercial Officer and SRO Vaccine Deployment
Dr Nikita Kanani | Medical Director for Primary Care
Eleanor Kelly | LA CEO advisor
Appendix I
Notional Allocations by STP
Appendix II
JCVI guidance – Health Inclusion Groups
Within the current JCVI guidance and cohort identification there is deliberate attention paid to mitigating health inequalities in how the vaccine is deployed:
JCVI advises that implementation of the COVID-19 vaccine programme should aim to achieve high vaccine uptake. An age-based programme will likely result in faster delivery and better uptake in those at the highest risk. Implementation should also involve flexibility in vaccine deployment at a local level with due attention to:
- mitigating health inequalities, such as might occur in relation to access for inclusion health groups (homeless, traveller, Gypsy, Roma communities) and ethnic minority groups
- vaccine product storage, transport and administration constraints
- exceptional individualised circumstances
- availability of suitable approved vaccines, for example for specific age cohorts
Whilst the data for inclusion health populations is inadequate there is a wealth of research that highlights the cliff edge of health inequalities. ONS data shows that for people experiencing homelessness the mean age of death for men was 44 years and for women 42 years*. Life expectancy for Gypsy Traveller men and women is 10 years lower than the national average.
*Deaths of homeless people (identified cases only and total estimated number) registered in 2013 to 2017 Office of National Statistics
Inclusion health populations are less likely to present for preventative health care and are less likely to be registered with a GP, and many have been refused access to health care due to not being able to provide proof of address or ID. As a result they are less likely to have a formal diagnosis of underlying health conditions that would identify them as Clinically Extremely Vulnerable (CEV) to COVID-19. Cohort studies of people experiencing homelessness show large numbers of excess deaths due to cardiovascular and chronic respiratory diseases*, which increase the risk of severe COVID.
*Hwang, S.W., et al., Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. 2009. 339.
These populations are at significant risk of severe disease and higher mortality and should be considered a priority for vaccination.
Deployment considerations
- Liaison with Local Authority and Voluntary Sector organisations providing accommodation and support.
- Produce a good estimate of the number of people in inclusion health cohort – Local Authorities hold data on: number of people being accommodated; estimates on those continuing to sleep rough; and GRT populations. Home Office hold data on number of Asylum Seekers and Refugees in Initial Accommodation (including temporary hotels).
- Identify where a significant number of people are being housed e.g. temporary hotels, hostels, refuges etc.
- Agree the best approach for engaging with the homeless residents in these places and on the street and encouraging uptake of vaccine (outreach).
- With community leaders agree the best approach for Gypsy, Roma and Traveller communities given level of vaccine hesitancy known within the population.
- Define the outreach team and the resources that they will require to carry out the vaccinations including mobile devices to access Pinnacle.
- Establish a paper based recording system for those who are not registered with a GP / with an NHS number, where possible register individuals prior to vaccination or at point of vaccination.
- Agree follow up protocol for 2nd vaccination and surveillance for those without stable contact details.
Local case studies
An increasing number of local areas have taken action using the flexibility identified in the JCVI guidance. All of the areas that have taken early action have specialist inclusion health practices and / or local leaders who understand the vulnerabilities of this population.
Oldham registered their homeless population with General Practice during wave one and have actively developed their outreach model to deliver the vaccine to everyone who has been identified and worked with local partners to reach those not in contact with General Practice: https://www.bbc.co.uk/news/uk-england-manchester-55661823
Liverpool – Brownlow practice (specialist inclusion health practice) with Central Liverpool PCN have written up their approach here: https://www.qni.org.uk/2021/02/01/covid-19-vaccination-for-inclusion-health-groups-in-liverpool/
Bradford – the vaccine board approved roll-out to inclusion health populations and Bevan Healthcare have commenced outreach delivery with a reportedly high uptake rate.
Crawley – in partnership with Metro, the Local Authority and Voluntary Sector partners have launched a COVID-19 vaccine bus that is outreaching in to communities who may otherwise not access the vaccine: https://www.bbc.co.uk/news/uk-england-sussex-55891472#:~:text=A%20Covid%2D19%20vaccination%20bus,for%20Better%20Care%20(ABC).
