Supporting patients of all ages who are unwell with coronavirus (COVID-19) in mental health learning disability autism
Contents
- Principles
- Managing a suspected or confirmed COVID-19 case
- Infection control prevention considerations
- Table 1: Considerations for patients with different levels of risk and symptom severity, and suggested actions
- Patient, family and carer engagement
- Training requirements and workforce support
- Palliative care
- Additional considerations
- Useful resources
Classification: official
Publication approval reference: C1557
Supporting patients of all ages who are unwell with coronavirus (COVID-19) in mental health, learning disability, autism, dementia, and specialist inpatient facilities
24 January 2022, Version 2
Updates to version 1 are highlighted. This guidance supersedes the previous version
The scope of this guidance includes NHS commissioned independent sector providers of inpatient services
This guidance has been assessed to identify potential equality impacts of the COVID-19 pandemic on people with mental health problems or a learning disability and/or autism. It is acknowledged that people with mental health needs, a learning disability or autism who contract COVID-19 may require reasonable adjustments, and that the COVID-19 pandemic has the potential to affect mental health and wellbeing. Health services must continue to have due regard to their obligation to advance equality under the Equality Act 2010: this includes recognising and factoring-in the vulnerability of different cohorts with protected characteristics including BAME patients; and inequalities in access, experience and outcomes in health services. The Advancing Mental Health Equalities Toolkit provides support in identifying and addressing mental health inequalities in the round. Partnership working with the voluntary and community sectors is also encouraged to facilitate wrap-around support for vulnerable people, and to maximise engagement with underrepresented groups.
Throughout this guidance, the term ‘provider’ refers to providers of inpatient services for people with mental health needs, a learning disability, autism or dementia. This guidance is applicable to provision of all bed-based care, including acute, intensive care, rehabilitation and specialised services.
Certain key principles should inform the provision of care to individuals in these settings who are suspected/confirmed to have COVID-19:
- People with mental health needs, a learning disability, autism or dementia may need additional support, including by making reasonable adjustments to care systems and clinical practice.
- It has previously been recommended that inpatient settings should ‘cohort’ patients, as far as possible, into those:
- with confirmed COVID-19
- without confirmed COVID-19.
- Inpatient settings should reorganise wards/bays/en-suite facilities and staffing arrangements to separate these cohorts of patients, to maximise protection for the maximum number of patients. Specific local arrangements will need to be kept under regular review as the size and gender mix of these cohorts are likely to change over time; see Managing capacity and demand guidance.
- Some basic aspects of physical care for people with suspected or confirmed COVID-19 can be provided in mental health, learning disability, autism or dementia settings.
- When an individual’s physical health needs escalate, they may need to be transferred in a timely way to an acute medical setting. Providers and commissioners should work within existing protocols for transfer to an acute setting. These protocols should support joint decision-making and ensure timely transfer and equity of access.
- Some providers will be able to deliver more advanced physical healthcare, depending on their configuration and available resources, including workforce and equipment. Where possible, community and district nursing teams should provide advice, guidance and support virtually.
- Wherever possible we must continue to guard against overly restrictive practice, see corresponding legal guidance;
- Individuals and their families and carers as appropriate should be involved in key decisions about the patient’s care, where appropriate to do so and should be provided with all relevant information in an accessible format.
- Providers are advised to ensure that staff are up to date in their training in relation to physical health (eg monitoring vital signs and the management of a physically deteriorating patient, or rapid upskilling from neighbouring physical health teams). Training opportunities such as those available on E-Learning for Health should be made available to all relevant clinical staff so that they can provide some level of physical healthcare for people with COVID-19.
- Vaccination against COVID-19 should be a priority for patients who are admitted into inpatient services and have not yet received the required dose.
The rest of this document expands on the above key principles and Table 1 gives suggested actions and key considerations for providers when caring for people with suspected/ confirmed COVID-19.
1 It is recognised that the need to cohort patients under these circumstances may mean that providers breach current guidance on delivering same-sex accommodation. They should then complete a full assessment of the implications for individuals.
Managing a suspected or confirmed COVID-19 case
People with mental health needs, a learning disability, autism or dementia should receive the same protection and support with managing COVID-19 as other members of the population. This includes, where required, rapid, urgent or emergency access to acute care.
If an individual receiving care and support in an inpatient setting has confirmed or suspected COVID-19, the risk to their health and wellbeing must be assessed and appropriate action taken to provide relevant care and support in accordance with the National IPC guidance.
Infection control prevention considerations
Where an individual is suspected or confirmed to have COVID-19, self-isolation procedures should be followed and they should be tested immediately and regular observations taken. This can support the development of a management and isolation plan. This activity should be carefully planned, managed and communicated to the individual who is required to isolate, to reduce the risk of trauma. Providers should also adopt a trauma-informed approach, with particular consideration of the effects of staff in personal protective equipment (PPE) providing care and support to individuals, recognising the overall aim of reducing trauma.
It is important to notify patients and their relatives if another patient on their ward has tested positive for COVID-19, but in doing so providers should bear in mind the overall need to maintain patient confidentiality. In line with Regulation 20 of the Health and Social Care Act (2008), providers should inform family members or next of kin when a patient, who may be on the same ward as their relatives, is confirmed to have COVID-19. Similarly, family members or next of kin should be informed where adjustments and/or restrictions are being made in line with national guidance about self-isolation for the individual and those who have been in contact with them.
Standard infection control precautions (SICPs) and transmission-based precautions (TBPs) must be used when managing patients with suspected or confirmed COVID-19. Further guidance can be found in COVID-19 Guidance for infection prevention and control in healthcare settings.
Individuals with confirmed COVID-19 should be isolated as far as possible. If they do not have their own en-suite room, they should be moved to a side ward/bay at the earliest opportunity to reduce the risk of transmission. Where en-suite rooms already exist, providers should move people so that all COVID-19 cases are cohorted in one area. All rooms and individuals should be risk assessed before any individual patient is transferred. For further detail see Managing capacity and demand guidance.
Case-by-case clinical reviews will be required where any patient is unable to follow advice on isolation and testing. Providers should decide the appropriate use of the relevant legal framework for each case, with support from legal experts as required. Non-concordance with isolation represents a clear and obvious risk to other people. This should, in the first instance, be conveyed to the patient, helping them to understand the clinical reasons for self-isolation and testing. For further detail, see Legal guidance.
Monitoring and clinical management
Regular observations and key symptom monitoring (ie relevant symptoms of Covid) should be completed and documented. The National Early Warning Score (NEWS 2) may be used to monitor the rate of physiological deterioration in individuals with suspected or confirmed COVID-19 cases. NEWS2 assesses physiological deterioration in these patients when combined with knowledge of the patient’s usual presentation while well and the clinical judgement of the attending clinician. NEWS2 is not appropriate for use in those under 16s, rather the Paediatric scale PEWS should be used instead. Providers are encouraged to use appropriate, validated tools in specific populations, such as children and adolescents and pregnant women.
RESTORE2 is a physical deterioration and escalation tool for care/nursing homes based on nationally recognised methodologies including early recognition (Soft Signs), the national early warning score (NEWS2) and structured communications (SBARD).
RESTORE2mini is an adaptation based on ‘soft signs’ that has tool has also been adapted for use in care settings including Care Homes, Domiciliary/Home care and congregate living for people with a learning disability.
Individuals should be assessed for pre-existing conditions which would make them high risk if they contract COVID-19 as well as their current general physical health, including COVID-19 signs and symptoms. Advice from physical health specialists should be sought where required and arrangements made to obtain advice from a senior physical health physician via telephone. Additional consideration should be given to the known specific contra-indications of medications and their side effects in patients with COVID-19 and other infections. For further guidance refer to information from specialist pharmacy services (SPS) see https://www.sps.nhs.uk/home/guidance/covid-19/ the National Association of Psychiatric Intensive Care and Low Secure Units.
Patients with a learning disability, autism or dementia and a co-morbid physical health condition may present with additional, softer signs or early indicators of deterioration, eg mood or behaviour changes, becoming unsteady when walking, increasingly tired, sleeping more, restlessness and agitation. These may be harder for the clinician to appreciate and harder for the patient to express. In this situation it would be advisable to speak (where possible) to carers and those most familiar with the individual to assess and note in the patient record for future reference how the person usually presents when well.
In many cases, patients can be safely cared for in their existing mental health, learning disability and autism, dementia and specialist ward, depending on the availability and safety of local facilities and the competence of the staff team in each setting to assess, monitor and intervene in physical healthcare. However, in some circumstances, transfer to a local acute facility may be necessary. Where required, an individual should be transferred at the earliest opportunity. All care and support provided should be in the individual’s best interests, with the aim of promoting positive patient experience and outcomes.
Table one below sets out further considerations and suggested actions for patients with different levels of risk and symptom severity. Local areas may wish to develop local escalation frameworks to support clinical decision-making.
Table 1: Considerations for patients with different levels of risk and symptom severity, and suggested actions
| Risk level | Severity of symptoms | Suggested actions | Key considerations, including resource and workforce implications |
| 1 | Individual has mild symptoms |
|
|
| 2 | Individual has moderate symptoms and other factors that make them more susceptible to the effects of COVID-19, |
|
|
| 3 | Patient is acutely unwell with severe respiratory symptoms associated with COVID-19 |
|
|
Patient, family and carer engagement
Individuals, their families and carers should be involved in key decisions about the patient’s care, where appropriate to do so. Any impact on leave or Care (Education) and Treatment Reviews (C(E)TRs) should be appropriately communicated to the individual and their family. Conversations will inevitably have to take place remotely, rather than face-to-face, and arrangements to support remote visits will need to be put in place. Further guidance can be found on the NHS Digital website. Services should consider providing digital devices to individuals who do not currently own them to make it possible for them to maintain contact with their family. Further detail about C(E)TRS can be found in Guidance on managing capacity and demand. It is also appropriate to ensure that individuals have access to advice and guidance from an advocate, either digitally or over the telephone. It is always important that people have access to appropriate independent advocacy and IMCA etc
Training requirements and workforce support
Supporting staff wellbeing will be vital, both in our responsibilities as an employer and as providers of compassionate, safe, quality healthcare. Now more than ever it is important to ensure there are appropriate structures for restorative clinical supervision, reflective practice and peer support. Providers should ensure that staff are appropriately trained to deliver relevant healthcare interventions within their competency and capabilities. As stipulated, where a transfer is required to an acute facility for more specialist care this should be expedited in a timely way.
For further guidance on supporting the workforce, please see the NHS England and Improvement website and the NHS Employers website. The Royal College of Psychiatrist and developed COVID-19 guidance for clinicians and the Royal College of Nursing has developed similar guidance.
Staff should be up to date in their training in physical health assessment and monitoring (eg monitoring vital signs and the management of a physically deteriorating patient, or rapid upskilling from neighbouring physical health teams) and delivering relevant physical health interventions to ensure the relevant expertise is available within the workforce supporting each ward. The CCQI quality standards for inpatient care have more detail on the recommended level of training for staff in this regard. https://www.rcpsych.ac.uk/docs/default-source/improving-care/ccqi/ccqi-resources/rcpsych_standards_in_2019_lr.pdf?sfvrsn=edd5f8d5_2.
Providers should urgently review and start training courses to ensure psychiatrists and senior mental health professionals are competent and confident in incorporating certain physical healthcare interventions into a care plan, prescribing the correct treatment and delivering these interventions, as appropriate. The initial priority of training should be to support the broad goal of increasing skills in managing isolation, assessing physical health using NEWS2 and PEWS, and being aware of respiratory distress, hypoxia and shock.
Palliative care
Where possible, providers should follow existing processes for patient transfer to an acute facility. Guidance on patient transfer can be found in section 6.3 of Guidance for infection prevention and control in healthcare settings.
Very rarely, transfer to an acute facility may not be possible, e.g. where an individual has deteriorated significantly and is close to death, making transfer clinically inappropriate. Any decision not to transfer an individual to a local acute facility for further treatment should be discussed with the individual, their family and carers, and taking into account any previously expressed wishes and feelings, and advance statements https://www.nhs.uk/conditions/end-of-life-care/advance-statement/. It may be useful also to discuss with the provider’s local COVID ethics committee.
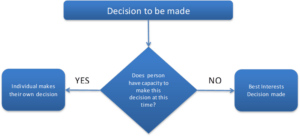
DNACPR forms should only be completed in appropriate circumstances where it is in the patient’s best interests, when the patient and their family and carers agree . If the person does not have capacity, then a due process of decision-making under the requirements of the Mental Capacity Act (2005) should be completed. For under-16 year olds, to whom the Mental Capacity Act (2005) does not apply, the principles of Gillick competence should be followed https://www.nhs.uk/conditions/consent-to-treatment/children/. Advance care planning guidance is available here.
No ‘blanket’ treatment plans across a group of individuals, based on their diagnosis, age or care setting, should be in place. The legal frameworks of the Mental Capacity Act and General Medical Council guidance on decision-making should continue to be followed. It is crucial that decisions are made on an individual basis even if the predicted outcomes are similar across patient groups. These decisions can be approached in a sensitive and timely way given the current situation.
A ‘do not attempt cardiopulmonary resuscitation’ (DNACPR) order is purely clinical guidance for a decision in the circumstances of a cardiac arrest, and not for a decision regarding any other clinical interventions. A DNACPR order does not cover decisions about escalation in the context of COVID-19 or an individual’s end-of-life care needs.
Regular observation measurement should continue, including NEWS2 testing and food and fluid monitoring. Comfort and pain issues should be regularly reviewed.
Palliative care support and advice should also be sought from specialists via telephone. Providers may wish to consider developing a shared protocol with local services around obtaining advice, guidance and support for the individual concerned. Friends, family and relatives should be consulted on a regular basis. Where appropriate, please refer to the Clinical guide for the management of palliative care in hospital during the coronavirus pandemic.
Decisions about conversations with friends and family will be driven by government guidelines on social distancing and Infection, Prevention and Control processes in individual wards. Where safe to do so, contact and visiting from family and friends should be maintained. Where it is not safe to do so face to face, due to an outbreak within the ward for example, people must be supported to communicate with their family over the phone/online
Some mental health and learning disability nurses may not have provided end-of-life care before and may need additional training and support through this.
Guidance for infection prevention and control in healthcare settings should be followed for the deceased. All steps should be taken to clear the area and carry out the required IPC measures.
Specialist eating disorder services
Wards that are compliant with NICE-guidance can provide NG feeding. Individuals with confirmed or suspected COVID-19 who are receiving NG/PEG feeds need to be managed with the correct PPE equipment in line with IPC guidance and appropriate training.
Where possible and in line with government guidance, providers should consider providing wrap-around care and intensive support in the community for this vulnerable group of patients.
Autistic people and those with a learning disability
Individuals with a learning disability have higher rates of morbidity and mortality than the general population and die prematurely. The third annual LeDeR report in 2019 showed that 41% of people with a learning disability died due to respiratory conditions. There is also a higher prevalence of diabetes, obesity and being underweight in this group. All of these factors make them more vulnerable to COVID-19.
Clinicians should be mindful of diagnostic overshadowing, when the symptoms of physical ill-health are mistakenly attributed to either a mental health/behavioural problem or as being inherent in the person’s learning disability. People with a learning disability have the same illnesses as everyone else but they may present, respond to or communicate symptoms, pain or distress in a very different way from other people. Specialist advice and support from clinical and liaison staff in learning disability and autism teams should be sought if they are not already involved.
Some people with a learning disability, autism or both may be inpatients in hospital settings that are not co-located with general hospitals. Local systems should proactively arrange clear arrangements for advice, support and facilitation of admission and subsequent discharge of patients with suspected or confirmed infection with COVID-19.
For further guidance on providing care for people with a learning disability who have tested positive for COVID-19 can be found on the NHS England and NHS Improvement website.
Mother and baby units
All women in the MBU should be supported to develop a COVID-19 management plan, outlining their personal care and support needs should they develop symptoms, in respect of their baby. To help them develop this plan, mothers should be able to access the latest advice and guidance from the Royal College of Obstetricians and Gynaecologists. Partners, co-parents and significant others should be involved in the development of this plan. The important role of the co-parent should be facilitated within service protocols, making full use of technology.
Services should continue to maintain links as needed with social services, health visiting and community services.
Adult and Children and young people secure services
Where secure services need to cohort patients due to COVID –19, this will need to be in line with the level of security required for individual patients based on clinical need and risk assessment and with agreement of Mental health Casework Section (MHCS) for restricted patients. This maybe more difficult in smaller providers where it may not always be possible to create capacity for COVID-19 positive patients.
Specifically, for adult medium and low secure services are encouraged to have a business continuity plan with their host NHS-Led Provider Collaborative to ensure that local systems can offer support. For CYP secure services, providers should consult with the relevant national network.
People with dementia
Most people with dementia are over 70, have other long-term conditions and are frail, meaning they are particularly vulnerable to develop complications if infected with COVID-19. People with dementia have a higher risk of getting COVID-19, are more likely to require hospitalization, and are more likely to have severe or fatal cases of this disease compared with people without dementia. It is important to recognise that the presentation of Covid-19 may be atypical in older adults.
Clinicians involved in screening and treatment should be aware of the additional anxieties people with dementia may experience on admission. It is advisable to allocate additional time for a holistic assessment, particularly getting information from any carers that know them about what they find reassuring and how they normally function. Advance care planning (ACP) can be used to identify the wishes and preferences of people with dementia; see My Future Wishes for further detail. Clinicians should identify if an individual has an ACP or a ‘health and welfare power of attorney’. Further detail on ACP can be found on the NHS England and Improvement website.
It may also be necessary to complete a swallowing assessment, to identify any potential swallowing difficulties that may put someone with dementia at increased risk of chest infections or dehydration.
It is important to ensure that all information regarding personal care and support for preventing COVID-19, such as self-isolation and handwashing, are available in accessible formats to ensure that all people with dementia can access it.
Individuals with dementia are much more prone to develop delirium (a confused state) if they become infected. Delirium can also be one of the first signs of a COVID infection in an older adult with dementia. They may also be less able to report symptoms because of communication difficulties. Clinicians should be alert to the presence of signs as well as symptoms of the virus (eg ‘look beyond words’).
Where required, conversations about end-of-life care should be tailored to reflect expectations in these two situations and palliative comfort measures offered.
If a person with dementia and COVID-19 is imminently close to dying and has symptoms such as breathlessness or severe delirium that are difficult to manage, specialist palliative care support and advice should be sought. Support also she be offered to carers Support also she be offered to carers.
In some cases, people with dementia may have impaired mental capacity. The Mental Capacity Act (2005) provides guidance on assessment of capacity and compliance with legal guidance to act in the individual’s best interests.
Antiviral Medications and Monoclonal Antibodies
There is a growing range of medications that are effective in reducing the risk of serious disease in people with COVID. These include neutralising monoclonal antibodies (nMABs, such as Casirivimab and Imdevimab (ronapreve) and Sotrovimab and antiviral medications (such a remdesivir and Molnupiravir).
These medicines are available only through organisational registration with the specialised BlueteqTM platform. It is unlikely that specialist providers of mental health, learning disability, autism or dementia services will either routinely access this platform or consistently operate a pharmacy model that supports equitable access to these medications across all of the commissioned services.
For people with severe COVID disease, these medications will be available following clinical criteria, in acute hospital settings.
People who are in the highest risk group of severe disease from COVID will benefit from access to these medications at the earliest opportunity in the course of symptomatic COVID infection. This will be before they become so ill with COVID that acute hospitalisation is required. COVID Medicine Delivery Units (CMDUs) have been established so that people in this eligible category are able to access these medicines in their communities (including in-patient facilities where transfers to CMDUs for administration or supply is not possible). This should be in line with latest policy guidance (currently within 72 hours of positive diagnosis by PCR and within 5 days of onset of symptoms of COVID).
Specific guidance for children and young people with COVID is available here: COVID-19 – guidance for management of children admitted to hospital and for treatment of non-hospitalised children at risk of severe disease | RCPCH. Children at increased risk are listed in Table 2.
CYP nMabs are licensed for use in children > 12 years of age and > 40Kg weight. There is a 5 day window for administration and there are regional MDTs who will advise on whether they are indicated. These MDTs are contactable by emailing: england.spoc-c19therapeutics@nhs.net [undefined:england.spoc-c19therapeutics@nhs.net with clinical details
The full statement of eligibility for community access to these treatments is defined in a Rapid Policy Statement published on 24th December 2021 and available at https://www.cas.mhra.gov.uk/ViewandAcknowledgment/ViewAlert.aspx?AlertID=103186
Note- guidance is updated regularly – check MHRA CAS alert for latest guidance https://www.cas.mhra.gov.uk/Home.aspx
Patients with Down Syndrome and rare neurological conditions are amongst the prioritised patient groups and may be amongst people who are inpatients in mental health, learning disability, autism, dementia and other specialist inpatient facilities. There are other people who may be inpatients who may have co-incidental physical health conditions which place them into one of the highest risk group categories.
Where a person who is in the highest risk group is diagnosed with symptomatic COVID disease, whilst an inpatient in a mental health, learning disability, autism or dementia service, and does not require acute hospitalisation, they must be able to access an antiviral medication or nMAB without delay.
If the person is able to access community leave, they should be supported to attend a CMDU to receive treatment. If the person cannot access community leave, then treatment should be provided in the place where the person is receiving treatment. Subcutaneous and oral forms of some treatments may be are available and will support administration in a mental health, learning disability, autism or dementia setting if eligible and indicated.
Providers of mental health, learning disability, autism and dementia services must identify any people who are in the highest risk groups and who are in their services as inpatients. Providers should ensure that any service in which people are treated has clear arrangements with their local CMDU, so that people can access treatment regardless of their ability to leave the hospital or care setting in which they are receiving treatment.
When considering the risks/benefits of transferring patients from mental health /non acute in-patient hospital settings in order to receive treatment providers should be aware of the emerging evidence which indicates a lower efficacy of oral Molnupiravir vs IV Sotrovimab in preventing hospitalised admission or death ( oral Molnupiravir relative risk reduction around 30% and IV Sotrovimab over 80%).
- Guidance for the public on the mental health and wellbeing aspects of coronavirus (COVID-19): https://www.gov.uk/government/publications/covid-19-guidance-for-the-public-on-mental-health-and-wellbeing/guidance-for-the-public-on-the-mental-health-and-wellbeing-aspects-of-coronavirus-covid-19
- ‘e-learning for health’ coronavirus resources: https://www.e-lfh.org.uk/programmes/coronavirus/
- Mencap: a range of easy read guides, including self-isolation, social distancing, and government guidance.
- UK Health Security Agency: easy read guidance on coronavirus
- UK Health Security Agency: advice about the coronavirus (easy read)
- Vaccination for people with dementia
- SPS Guidance on Covid treatments https://www.sps.nhs.uk/home/guidance/covid-19-treatments/
- Training https://portal.e-lfh.org.uk/Catalogue/Index?HierarchyId=0_45016&programmeId=45016
