Vaccination as a Condition of Deployment (VCOD) for Healthcare Workers: Phase 1 – Planning and Preparation
Contents
- Introduction
- Overview
- A. Planning
- B. Preparation
- Resources
- Appendix 1: Workers required to be vaccinated as a condition of deployment for healthcare workers
- Appendix 2: VCOD Flowchart Scenarios
- Appendix 3: New starters
- Appendix 4: Key recommended actions checklist
Classification: Official
Publication approval reference: C1470
Guidance for employers in healthcare in England
6 December 2021 Version 1
Introduction
Regulations
The Department of Health and Social Care, on 9 November 2021, laid regulations which amend the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (“the 2014 Regulations”), to provide that the registered person can only employ or otherwise engage a person in respect of a CQC regulated activity, if the person provides evidence that they have been vaccinated with a complete course of an authorised vaccine against COVID-19 or, if otherwise vaccinated against coronavirus is also within a specified time period, vaccinated with a single dose of an authorised vaccine, subject to specific exemptions.
These regulations will sit alongside the already existing regulations which require registered persons of all Care Quality Commission (CQC) registered care homes (which provide accommodation together with nursing or personal care) to ensure that a person does not enter the indoor premises unless they have been vaccinated (subject to certain exemptions) which came into force on 11 November 2021.
These regulations will apply equally across the public (NHS) and independent health sector, and will require workers aged 18 and over, who have direct, face to face contact with service users to provide evidence that they have received a complete course of a Medicines and Healthcare products Regulatory Agency (MHRA) approved COVID-19 vaccine, subject to limited exceptions, by no later than 1 April 2022. This will include front-line workers, as well as non-clinical workers not directly involved in patient care but who nevertheless may have direct, face to-face contact with patients, such as receptionists, ward clerks, porters and cleaners.
These regulations will protect vulnerable people and individual workers in health and social care settings, including hospitals, GP practices, dentists, community services and where care is delivered in a person’s home. The requirements will apply to CQC-regulated activities whether they are publicly or privately funded. They will also apply where a regulated activity is delivered through agency workers, volunteers, locums, students or trainees, or contracted to another provider. Compliance will be monitored and enforced by CQC.
Registered person
Any person (individual, partnership or organisation) who provides regulated activity in England registered with the CQC.
The use of the term ‘employer’ in this document refers to the registered person. Further information regarding CQC registration can be found on the CQC website.
CQC regulated activity
CQC monitor and regulate services that provide health and social care.
Examples of the types of activities CQC regulates includes::
- personal care
- accommodation for persons who require nursing or personal care
- accommodation for persons who require treatment for substance misuse
- treatment of disease, disorder or injury
- assessment or medical treatment for persons detained under the Mental Health Act 1983
- surgical procedures
- diagnostic and screening procedures
- management of supply of blood and blood-derived products
- transport services, triage and medical advice provided remotely
- maternity and midwifery services
- termination of pregnancies
- services in slimming clinics
- nursing care
- family planning services.
Children’s services, clinics, community-based services for people with learning disabilities and substance misuse, hospices, health and justice secure settings are also types of services regulated by the CQC. A full list of activities and services can be accessed on the CQC’s website.
CQC activity
It is our expectation that the registered person would keep a record of vaccinations as part of their staff employment or occupational health records.
When registering with CQC and if inspected, the registered provider will need to be able to demonstrate that:
- They have systems in place to ensure that they can comply with the requirements of the regulations and that they can monitor compliance.
- There is a record to confirm that satisfactory evidence has been provided. This record must be kept securely by the registered person in compliance with the UKGDPR and the Data Protection Act 2018.
- They have systems in place to review whether they need further evidence in relation to vaccination or exemption status of the people they employ or otherwise engage for the purposes of the provision of the regulated activity, carry out those reviews and secure such further evidence.
- There is appropriate information and access to advice/guidance about vaccines and the requirements of the regulations available to all workers, and that individuals receive support in connection with the vaccine.
- Workers are provided with the appropriate support to access vaccination.
The purpose of this guidance
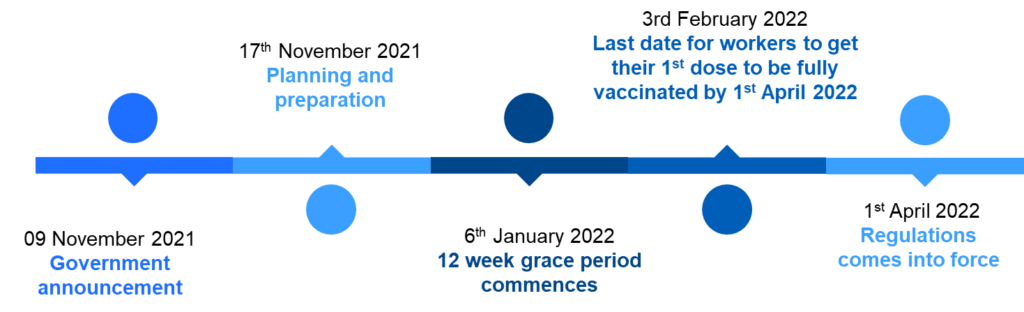
The regulations were laid in Parliament on 9 November 2021 and subject to parliamentary passage will come into force on the 1 April 2022. If the regulations are approved, unvaccinated individuals will need to have had their first dose of an approved COVID-19 vaccine by 3 February 2022 (this date is subject to change), in order to have received their second dose by the 31 March 2022 deadline.
NHS England and Improvement (NHSEI) has engaged with the Social Partnership Forum (SPF), NHS Employers and Department of Health and Social Care (DHSC) to develop this guidance to support service providers in preparing and planning for the regulations.
Guidance will be produced in two phases and will be reviewed and updated accordingly. The focus of this ‘phase one’ guidance is to:
- support compliance with the regulations,
- maximise vaccination rates,
- minimise the impact of the regulations on the NHS workforce capacity,
- provide a consistent approach in the planning and preparation for the regulations, with minimal operational differences between organisations, and
- support employers ensuring the best protection for vulnerable patients and staff in healthcare settings.
Phase two of the guidance will focus on the safe transition of services and will cover the formal steps that should be considered when implementing the regulations.
Who this guidance is aimed at?
This guidance is aimed at NHS Trusts and Integrated Care Systems (ICS), however, the purpose of this guidance and principles set out can generally be applied to other NHS organisations such as primary care services. It is noted that as independent employers, primary care providers may wish to seek individual legal advice.
Overview
Key actions and indicative timeline (subject to parliamentary passage – dates below may change)
Regulation objectives
Making COVID-19 vaccination a condition of deployment in health and adult social care settings (domiciliary care and other CQC-regulated settings) is intended to:
- Protect all those who use health and care services, a large number of whom are vulnerable, as well as the wider community.
- Protect workers themselves by increasing vaccination rates.
- Help reduce COVID-19 related sickness absences.
When do employers need to act on these changes?
The regulations are expected to come into force on 1 April 2022, subject to the passage of the regulations through Parliament. In advance of this date, the government approach will include a 12-week grace period from when the regulations are made to when the regulations come into force. This period is intended to give providers and workers the time to meet the new regulatory requirements. Under current vaccination guidance, eight weeks are required between the first and second vaccine dose.
Employers in partnership with local staff side representatives need to act now to:
- Review and assess which roles are likely to fall within the scope of the new regulations.
- Review and update privacy notices (please refer to data information section in this guidance).
- Actively support uptake of vaccination via communication and engagement. Evidence has shown that sensitive 1:1 conversations approached holistically, with empathy and respect, are the best way to convert vaccine hesitancy to vaccine uptake.
- Understand and document ‘in scope’ workers vaccination and exemption status. Ensuring systems are in place to keep this under review.
- Agree arrangements with suppliers of temporary, agency or bank workers, education institutions who provide students and any other partners who supply workers or volunteers who will be required to evidence vaccination to continue to be deployed into relevant settings.
- Start to identify options for potential redeployment to non-face-to-face roles, however, avoid taking formal action in regard to redeploying workers or reallocating duties until the regulations have received parliamentary approval. There will be a 12-week grace period from when the regulations are made to when the regulations come into force which will give workers time to decide to get vaccinated.
- Proactively plan and identify potential workforce reconfigurations and redesign, ahead of 1 April 2022, to support staff wellbeing and avoid disruption to services.
It is recommended that formal redeployment of workers should not commence until the regulation has been approved by Parliament which is expected on 6 January 2022 (this date is subject to change).
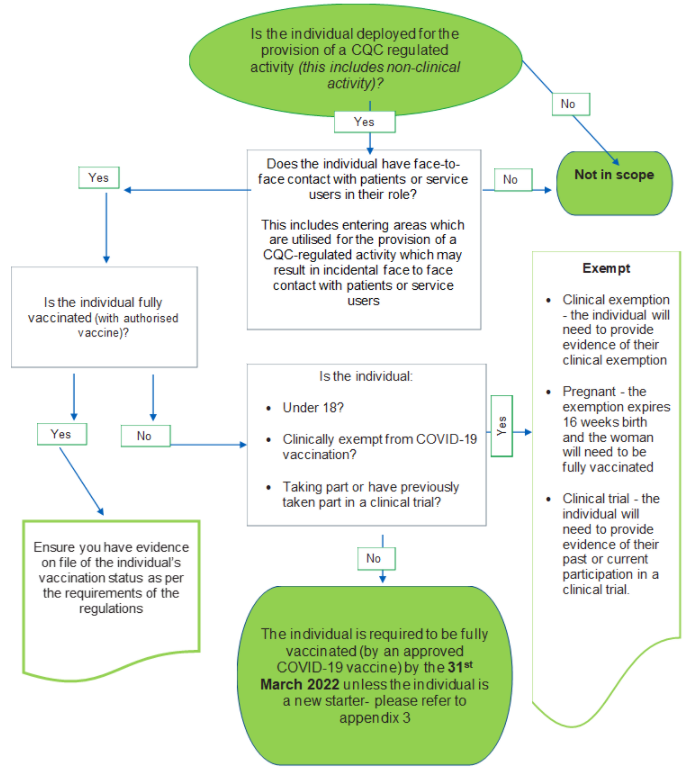
Who is in scope of the regulation?
Workers who have face-to-face contact with patients and/or service users and who are deployed as part of CQC regulated activity.
The regulations apply to health and social care workers who are deployed in respect of a CQC regulated activity, who have direct, face-to-face contact with service users. This include individuals working in non-clinical ancillary roles who enter areas which are utilised for the provision of a CQC-regulated activity as part of their role and who may have social contact with patients, but not directly involved in patient care (e.g. receptionists, ward clerks, porters, and cleaners), regardless of contracted hours or working arrangements. All honorary, voluntary, locum, bank and agency workers, independent contractors, students/trainees over 18, and any other temporary workers are also in scope.
The requirements would not apply to those employed, or otherwise engaged, in the provision of a CQC regulated activity if they do not have direct face to face contact with patients and/or services users/patients. For example, those providing care remotely, such as through triage or telephone consultations or those in managerial roles working on sites separate from patient areas would not have direct face to face contact and so registered persons could continue to deploy them in those roles as usual. People on long term absence from work, such as maternity, shared parental leave or sickness absence, would not be in scope unless and until they return to having any face to face contact (which would include on one off visits such as Keeping in Touch (KIT) days).
A person may be deployed in the provision of the regulated activity despite not having been vaccinated if that person:
- Is under the age of 18
- Is clinically exempt
- Is exempt due to a short-term medical condition (which is an option that some pregnant women may choose to take; for pregnant women the exemption expires 16 weeks post-partum and so will allow them to become fully vaccinated after birth)
- Has taken part or is currently taking part in a clinical trial for a COVID-19 vaccine
Refer to appendix 1 Workers Required to be Vaccinated as a Condition of Deployment – Flow Chart, if help is required in determining if a worker is in scope of the regulations.
Students and trainees
The registered person is required to demonstrate that they have systems and processes in place to evidence and monitor that all students and trainees (over 18) on placement within a healthcare setting, who have face-to-face contact with patients and/or service users and who are deployed, as part of CQC regulated activity, are fully vaccinated against COVID-19.
Students and trainees who opt not to have the vaccination but are not exempt from the regulations, should be directed to their educational provider to discuss the impact this will have on their progression through their programme.
Organisations should ensure that students and trainees are included is all communication and engagement plans to drive up vaccination uptake. Where possible, this should include any targeted campaign, webinar, supportive 1:1 conversations, and disseminating vaccine education and information material on the facts around vaccination.
Contractors, suppliers and bank and agency workers
The registered person is required to demonstrate that they have systems and processes in place to evidence and monitor that all independent contractors, agency or bank staff who have face-to-face contact with patients and/or service users and who are deployed, as part of CQC regulated activity, are fully vaccinated against COVID-19.
If applicable, employers should work with independent suppliers of staff to agree and plan any steps and update contractors to ensure the employer can comply with the requirements of the regulations.
Primary care and independent sector
The new regulations also apply to those working in specific primary care settings (general practice and dentistry) and the independent sector. In most cases the principles set out in this guidance document can be applied to workers in these settings, however, primary care providers may wish to seek individual HR and legal advice to take into account variations in local contractual terms and conditions.
Partnership working within and across primary care networks and ICSs are also encouraged to share resources and expert knowledge. We will engage further with primary care representatives to consider any specific guidance needs for this sector.
How can workers evidence that they are fully vaccinated?
Recognised evidence of COVID-19 vaccination
- The NHS COVID pass, or equivalent from NHS Scotland, NHS Wales or the Department of Health in Northern Ireland; or
- The EU Digital COVID Certificate; or
- The Centers for Disease Control and Prevention vaccination card; or
- A certificate in English, French or Spanish issued by the competent health authority which contains:
- the individual’s full name
- the individual’s date of birth
- the name and manufacturer of the vaccine that the individual received
- the date that the individual received each dose of the vaccine
- details of either the identity of the issuer of the certificate or the country of vaccination, or both.
NHS appointment cards cannot be used as proof of vaccination status.
Vaccinated abroad
Individuals who are vaccinated abroad will be required to provide evidence of their vaccination status and, where necessary, have a top-up dose with a UK authorised vaccine consistent with the UK Health Security Agency (UKHSA) guidance on vaccines. To avoid doubt, mixed doses (that is, where different vaccines have been administered to complete the dose schedule) will be accepted for the purposes of the vaccination requirements.
Clinical exemptions
Some individuals may have grounds not to have the vaccine for clinical reasons. Anyone who is unable to get vaccinated for clinical reasons will have to use the NHS COVID Pass to show their exemption status.
The domestic NHS COVID Pass will look and work in the same way for people with clinical exemptions as it will for people who are fully vaccinated. The pass will not show that a worker has a clinical exemption. Workers will receive a confirmation letter which they should keep for their records and use to prove that their unable to get vaccinated. The letter will explain that the individual is medically unable to get vaccinated, the pass does not.
Registered persons can continue to use workers for whom vaccination is not clinically appropriate, however, managers should take steps with regards to ensuring the health and safety of both the individual, other workers, patients and visitors. Managers will be required to update existing risk assessments to ascertain the potential risk of COVID-19 spread caused by unvaccinated (but exempt) workers and to identify the level of risk of exposure to the individual, other workers, patients and visitors. As a result of this assessment, managers may be required to put in place other ‘measures’ and reasonable adjustments to help reduce the risk, which may include reviewing current personal protective equipment (PPE) use, regular lateral flow testing, remote working, sufficiently ventilated workplaces, cleaning regimes and hand hygiene etc.
Pregnancy and fertility
The Joint Committee on Vaccination and Immunisation (JCVI) has advised that pregnant women should be offered COVID-19 vaccines and that pregnant women should discuss the risks and benefits of vaccination with their healthcare professional, including the latest evidence on safety and which vaccines they should receive. Women trying to become pregnant do not need to avoid pregnancy after vaccination and there is no evidence to suggest that COVID-19 vaccines will affect fertility.
While the Royal College of Obstetricians and Gynaecologists (RCOG), the Royal College of Midwives (RCM) and the UK Tetralogy Service recommend the COVID-19 vaccination for pregnant and breastfeeding women, pregnant women are eligible to request short-term medical exemptions from vaccination.
For pregnant women, the exemption expires 16 weeks after giving birth. This will allow them to become fully vaccinated after birth. A MATB1 certificate can be used to provide evidence of exemption status.
For further guidance regarding supporting pregnant women in the workplace, please refer to Coronavirus (COVID-19): advice for pregnant employees – GOV.UK (www.gov.uk) and COVID-19 vaccines, pregnancy and breastfeeding (rcog.org.uk).
Occupational Health and risk assessments
It is imperative that employers refer individuals who are exempt from having the COVID-19 vaccine, who may be clinically exempt, and pregnant women to Occupational Health for advice and recommendations including locally commissioned occupational health services for primary care providers.
Primary care organisations should contact their local commissioner if they require details of their local OH supplier.
Risk assessments will need to be reviewed and repeated as necessary in line with changes to individual circumstances, emerging evidence and/or national advice, to ensure the mitigation of workplace risk, identification of reasonable steps to be taken and additional support required.
Exemption from COVID-19 vaccination due to participation in clinical trial
In line with clinical advice, those who are taking part or have previously taken part in a clinical trial for a COVID-19 vaccine will be exempt from the requirement.
The registered provider will need to evidence that workers are exempt from having the completed course of an approved COVID-19 vaccination due to participation in a clinical trial.
The worker should provide the registered persons with confirmation in writing, from the organiser of the clinical trial, evidencing that the clinical trial they are participating in / has participated in is:
- For a vaccine against coronavirus; and
- Is regulated by one of the regulatory bodies included in annex B of the code of practice included in the ‘Making vaccination a condition of deployment in health and wider social care sector. Government response to public consultation’ document
Is the COVID-19 booster included in the regulations?
At present, the regulations do not require evidence of boosters, but employers are strongly advised to provide supportive advice to workers to encourage uptake of the booster vaccine if eligible.
Is the flu vaccination a condition of deployment?
At present, it is not proposed that flu vaccination requirements will be introduced as a regulation, however, the government will keep this under review following this winter and ahead of winter 2022/23.
Phase 1: Planning and preparation
A. Planning
Workforce planning
It is noted that this section on workforce planning is primarily applicable to NHS Trusts and ICS’s however the information included can also be considered by primary care organisations.
In all NHS organisations it is the responsibility of the registered manager to implement the regulations, however, employers should, where possible, form a cross-functional team (for example, including HR, Heads of Clinical Services, Information Governance leads and Staff Side representatives) to drive planning and related action. Employers should consider a partnership approach to the application of the new regulations within their Integrated Care Systems (ICS) in an effort to share resources, expert knowledge, provide support and widen opportunities for the redeployment of unvaccinated staff into non face-to-face roles/projects if possible.
Employers are advised to proactively plan their approach to compliance with the regulations in partnership with staff side representatives, commencing with the identification of the staff groups in scope and a review of staff vaccination data. Local data should confirm the numbers of staff in scope, staff vaccination status and inform options for action, key messaging and the resources required.
Employers should start to investigate how certain roles could be redesigned to enable the re-allocation or restriction of duties (taking into consideration the impact upon other staff and services) and opportunities for staff to potentially be redeployed.
Employers should plan redeployment processes and parameters and put in place a proposed timetable and consistent processes for staff engagement on redeployment and next steps. Where possible this should be undertaken within the planning phase, to support staff wellbeing and minimise the potential for service disruption once the regulations come into effect.
Action plan
We recommend that an action plan is drawn up as soon as possible to include the following:
- Initiatives to increase local vaccine uptake taking into consideration the needs of groups where there are low vaccination levels. Resources available for engaging and communicating with staff to increase vaccination uptake can be found here
- Build in support and training time for the managers responsible for working through the process.
- Note the deadlines for individuals to receive their first vaccination is 3 February and second vaccination is 31 March 2022.
- Allow sufficient time for the relevant processes to be implemented and/or concluded by 1 April 2022 deadline, including exploring all options with those who are not exempt and have indicated that they will not be fully vaccinated by the deadline date.
- A specific COVID-19 vaccination policy / procedure.
- Review and assess which roles are likely to be in scope (appendix 1).
As part of the action plan, subject to the timescales / deadlines mentioned above and subject to the passage of the regulations through Parliament, we recommend the following, for individuals directly employed:
- Ask workers to confirm their vaccination status / intentions in writing and set deadlines. All declarations confirming a full completed course of the COVID-19 vaccine will need to be evidenced as per the information in the overview section of this guidance.
- Engage in supportive conversations with colleagues who are indicating that they may not get vaccinated at the earliest opportunity. Encourage vaccine take up and talk honestly about the impact of their decision on their role and, if relevant, the limitations of redeployment into non face-to-face roles/projects.
- Have a meeting with those who refuse or are exempt to confirm evidence required, assess risk and discuss next steps.
- If workers have been vaccinated or are exempt from the vaccine, obtain evidence.
- If it is unlikely that the worker will be fully vaccinated by 1 April 2022 (and no exemption applies), undertake a formal process with the individual in line with internal policy if applicable ensuring that the individual is aware of the possible implications of their failure to be vaccinated by 1 April 2022.
Engagement with unions
It is best practice for employers to engage with unions and/or staff representatives to collaboratively agree a supportive approach to encourage workers to be vaccinated, agree processes to inform staff, discuss concerns and to consider practical and operational issues. Employers should refer to local partnership agreements and where relevant, consider seeking their own independent legal advice if necessary.
In addition, employers should schedule regular discussions with their Freedom to Speak up Guardian(s) and local staff Equality, Diversity and Inclusion (EDI) networks to support dialogue with staff, identify barriers to participation in the COVID-19 vaccination programme and to address staff concerns.
Adopting a vaccination policy/procedure
Developing (or updating) a policy on COVID-19 vaccination in partnership with staff side representatives, allows employers to outline the organisation’s stance on vaccination and explain the role and expectations of managers, HR and employees.
The policy might cover matters such as:
- The benefits of vaccination and how employees can contribute to wider public health by protecting themselves and other employees and wider community by being vaccinated.
- Whether staff over 18 are entitled to time off work (with or without pay) to be vaccinated or obtain evidence of medical exemption.
- Any arrangements relating to leave if staff experience side effects from vaccination. For example, it may be preferable to avoid a large number of staff being vaccinated on a single day.
- How an individual’s vaccination status can be evidenced.
- How data about vaccination or exemption will be processed.
- How any formal policies will apply to staff who cannot comply with the requirement.
- How vaccination requirements of new recruits and agency staff will be addressed.
- Any equality issues that arise from complying with the regulations (see section on Equality Act 2010).
Equality Impact Assessments
DHSC has completed an Equality Impact Assessment (EIA) on the potential impact of the policy on people with protected characteristics. The analysis can be found here.
Local EIAs should be completed to consider and understand the likely impact of the regulations on staff with protected characteristics. Employers will need to have due regard to the potential risks and challenges of decisions and actions associated with making vaccinations a condition of employment.
Working in partnership with Equality, Diversity and Inclusion (EDI) colleagues, local EDI staff network leads may be able to provide specialist advice on the potential impact and mitigations associated with staff groups and guidance on targeted approaches with groups in which vaccination uptake is low.
Data considerations
Vaccination status is ‘health’ information and would be regarded by many as confidential. It is also ‘special category’ data for the purposes of data protection legislation (the UK GDPR), which means that it must be used fairly, lawfully, supported by good reasons, and in compliance with other specific obligations under data protection law.
Employers will need to comply with requirements of data protection law, for instance updating privacy notices explaining to individuals how their data is being used, ensuring that the data is kept securely, and that access is controlled. In the circumstances, it would also be prudent for employers to undertake a data protection impact assessment (DPIA). Please refer to ICO Guidance and local Information Governance policies.
Employers must not use the data for purposes other than checking vaccination status for the purpose of the regulations, nor store the data for any longer than is necessary to fulfil that purpose.
We recommend that employers take the following points into account when collating vaccination data:
- Employers should be clear with workers about how details of whether or not they have had the vaccine will be used. Staff privacy notices should be updated to include such information.
- Work with staff side representatives and other stakeholder groups to ensure that staff understand what data is being proposed and why.
- Involve the employer’s data protection officer and, where applicable, the Caldicott Guardian.
- Ensure that if data about vaccine status is shared, it only goes to those who ‘need to know it’. Consider also other documenting policy issues such as what employees should be told about how the data will be used, how the organisation will handle the data, what technical and organisational arrangements in place to secure storage and limit access.
- Consider for how long vaccination data will be retained, in line with data protection law, and update any data retention schedules covering staff data.
- Have a policy and documented “risks versus benefits” assessment which demonstrate how decision making is justified.
Recruitment
We recommend that employers should include a provision about vaccination and clinical exemption into recruitment processes, offer letters and contracts for new employees. When recruiting staff and workers whose roles are likely to involve Care Quality Commission (CQC) regulated activities and face to face contact with patients and/or service users, it will be lawful to ask candidates about their vaccination status.
New starters
The proposed amendment of the Code of Practice on Infection Prevention and Control and its associated guidance detail that those newly joining the workforce will also need to be vaccinated in order to be deployed by a CQC registered person. The registered person must only deploy those who have had their first dose of vaccination, with a second dose within 10 weeks. This approach is intended to help balance the requirements of the policy with workforce pressures in health and care services.
The effect of the regulations for different staff based on the date that they are first employed or engaged for the purposes of the regulated activity is described in detail, in appendix 3 ‘New Starters’.
B. Preparation
Driving vaccination uptake
The Health and Safety at Work Act 1974 obliges employers to take reasonable steps to reduce any workplace risks; this duty gives employers justification for encouraging their employees to be vaccinated to protect themselves and everyone else at the workplace. COVID-19 is also a reportable disease under the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations (known as RIDDOR) which strengthens employers’ encouragement that employees should agree to vaccination.
Whilst many staff, volunteers, students, and bank/agency and temporary workers, have welcomed the opportunity to be vaccinated against COVID-19, there are still individuals who are reluctant or hesitant to have the vaccine. Whether to be vaccinated or not is a personal decision based on many factors and it is important to bear in mind that in most cases a decision not to have the vaccination is not a disciplinary or conduct issue. The reasons could be many and varied, including individuals who can’t have the vaccine (for example, on medical grounds), those who can have the vaccine but do not wish to do so (for example, on religious or spiritual grounds) and those who can have it but have concerns and are uncertain (for example, due to a mistrust of vaccinations generally).
Employers should refer to previous COVID-19 vaccination communications and engagement campaigns which remain a vital tool in promoting and encouraging vaccinations amongst their workforce. Employers are urged to review key messaging to ensure it is clear, complete, and accurate, and it aligns with current circumstances.
Employers should commence with:
- Liaising with staff side colleagues and EDI networks for support in encouraging workers to receive the vaccine.
- Showing support for vaccination from senior leadership.
- Ensuring line managers responsible for working through the process are aware of the organisational policy and approach and are supported throughout.
- Running an awareness campaign, drawing on NHS information and directing people to trusted sources of information.
- Disseminating vaccine education and information material on the facts around vaccination. Offer employees consistent, accessible and factual safety data which promotes the genuine achievement of science in producing an effective vaccine.
- Further increase engagement with targeted communities where uptake is the lowest, including extensive work with BAME and faith networks to encourage healthcare workers to receive the vaccine.
- Making it as simple and convenient as possible for people to receive the vaccine and to make the most of walk-ins, pop-ups, and other delivery models, such as hospital hubs, vaccinations centres and local vaccination services.
- Holding webinars and Q&A sessions with COVID-19 experts and community leaders, especially inviting doctors or public health experts who reflect the race/ethnicity or cultural identity of the workforce. This can be done as a system wide approach to efficiently share resources.
- Holding 1:1 conversations for all unvaccinated NHS staff with their line manager, with clear guidance on how to do this. This was associated with an increase in vaccine uptake by 10% in phase 1.
It is recommended that a system wide, panel of diverse experts who can provide specialist advice regarding vaccinations, is assembled to provide accessible advice to workers who still have queries or questions.
Targeted information is available from NHSEI to tackle misconceptions around vaccinations. For example, we are engaging with clinicians, BAME networks and faith leaders through our advisory groups to ensure we provide appropriate support across the workforce; and have created videos with experts around fertility and pregnancy to reassure staff of the safety and importance of being vaccinated against COVID-19.
Supportive 1:1 conversations
We know that one-to-one conversations have been the most effective way to support colleagues to make an informed choice, often leading to vaccination uptake. Therefore, we ask organisations to ask line managers to have supportive one-to-one conversations with unvaccinated staff to identify reasons for vaccine hesitancy and provide information that will support them to make an informed decision about the vaccine.
To ensure conversations are focused on support, compassion, understanding and encouragement, we recommend employers coach and train managers as to how to conduct the conversations. This can help to ensure consistent messaging and best practice approach in addition to mitigating against individuals feeling that the conversation with them had not been handled correctly or that they were being ‘forced’ to have the vaccination.
Conversations should include:
- Ensuring the individual is aware of the regulations and advising them of the impact of the regulations on their role.
- Discussing any individual circumstances that may currently be stopping them from getting the COVID-19 vaccination with understanding and compassion.
- If the individual advises that they are medically exempt, please signpost them to obtaining evidence of clinical exemption.
- Addressing concerns and vaccine hesitancy.
- Providing details of access to expert clinical advice from clinicians locally wherever possible.
- Signposting the employee to support services (including health and wellbeing and occupational health) and COVID-19 vaccination information resources from NHS England and the Department of Health and Social Care.
- Encouraging the employee to have further conversations with their own GP or trusted healthcare professional if they have any further questions around vaccination.
A detailed record of informal conversations should be maintained.
Resources to assist with 1:1 conversations can be found here.
Redeployment
Employers should consider the possibility of redeployment for staff in scope of the regulations and who remain unvaccinated on 1 April 2022. It is noted that the possibility of preserving security of employment applies only to those employed under a contract of employment with that employer and not to other workers who are in scope of the regulations. A national redeployment framework designed in partnership with staff side colleagues will be developed and shared in due course. Employers can refer to internal redeployment policies but should be mindful of the extension of such policies in these exceptional circumstances.
If alternative solutions such as the amendment, reallocation or restriction to staff duties and responsibilities are not applicable for staff in scope of the regulations who are directly engaged on a substantive contract and who choose not to participate in the COVID-19 vaccination programme, it is recommended that employers start to consider potential redeployment opportunities locally and across the ICS.
It is acknowledged that opportunities for redeployment may be challenging for smaller organisations, including many primary care providers.
The approach to the redeployment agreed in partnership with staff side, should be guided by a set of best practice principles to ensure a fair and transparent process in addition to local policies, including consideration of the following:
- Vaccination period extended – subject to the outcome of a risk assessment, staff may be redeployed on a temporary basis where possible if the first dose of the vaccine has been received and the second dose is scheduled after 1 April 2022 (while individuals will be afforded some protection against COVID-19 from 3 or 4 weeks after their first vaccine dose, they must not be permitted by the employer to work in roles that require face-to-face contact with patients or service users until they receive their 2nd dose).
- Staff who are temporarily redeployed during the extended vaccination period may be eligible for pay protection in accordance with an organisation’s protection arrangements.
- Whether potential suitable alternative roles should be ring-fenced with consideration given to other staff who may be subject to redeployment for a reason unrelated to the regulations.
- Clear guidance should be in place regarding the redeployment process and how staff will be assessed as suitable for a role (focus on assessing transferable skills from the point of what staff can do as opposed to what they can’t).
- A selection framework may be agreed for similar roles to ensure consistency of approach.
- If there are several potentially suitable redeployees, some form of competitive assessment will need to take place and should be made clear in advance and applied consistently.
- Consideration of equality principles in accordance with usual recruitment approach.
- Written feedback provided to the employee if they are not a suitable match for a vacancy, detailing clear justification as to why the redeployee has been unsuccessful. This feedback can support future job searches.
- Whether a trial period will be offered for staff who are permanently redeployed to alternative roles.
- The extent to which training, and development will be available to support permanent redeployment if applicable.
Permanent redeployment of employees will potentially impact upon their pay and pension. For clinical staff moving to a non-clinical role maintaining their professional registration will also be impacted. Staff are encouraged to seek advice from the NHS Business Services Authority (NHSBSA) and their professional governing body.
If local redeployment is exhausted, managers should consider wider redeployment within other Trusts, local authority and ICS.
Health and wellbeing support
In addition to signposting individuals to internal health, wellbeing and psychological support, NHSEI has put in place a comprehensive package of wellbeing support for health and social care workers which is available to all primary, secondary and tertiary care organisations. The support package includes:
- a dedicated health and care staff support service including confidential support via phone and text message
- free access to a range of mental health apps
- a range of counselling and talking therapies
- online resources, guidance, and webinars
Resources
- COVID-19 vaccination: guide for employers – GOV.UK (www.gov.uk)
- Bridging-the-uptake-Gap-BABAC-Toolkit-210622.pdf (england.nhs.uk)
- NHS England and NHS Improvement London » COVID-19 vaccine communication materials
- COVID-19 vaccination: guide for adults – GOV.UK (www.gov.uk)
- COVID-19 vaccination: easy-read leaflets – GOV.UK (www.gov.uk)
- Coronavirus » Primary care guidance (england.nhs.uk)
- Coronavirus infection and pregnancy (rcog.org.uk)
- https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/health-conditions/
Appendix 1: Workers required to be vaccinated as a condition of deployment for healthcare workers
Appendix 2: VCOD Flowchart Scenarios
Scenario 1: electrician (tradesperson) visits a hospital ward to fix some loose cabling
Is the individual deployed by the registered person for the provision of a regulated activity? NO: the individual is not in scope of the policy.
The tradesperson is not deployed for the provision of a CQC-regulated activity.
**Maintenance workers in the hospital estates and facilities team are in scope of the policy as their role is part of the provision of a CQC-regulated activity. Additionally, they are likely to have social contact with patients in clinical areas.
Scenario 2: cafe workers who serves food and drink to both staff and patients
Is the individual deployed by the registered person for the provision of a regulated activity? NO: the individual is not in scope of the policy.
Although this worker is likely to have direct face-to-face contact with patients, they are not deployed by the registered person for the provision of a regulated activity and as such the worker is out of scope.
**Please note that canteen or catering staff who are involved in providing food to patients or service users, particularly in inpatient or residential settings, are in scope as their roles facilitate the delivery of CQC-regulated activities.
Scenario 3: volunteer in a hospital shop located within an ante-natal clinic
Is the individual deployed by the registered person for the provision of a regulated activity? NO: the individual is not in scope of the policy.
While the volunteer may have social contact with patients within the clinic, they are not deployed by the registered person for the provision of a regulated activity and as such are not in scope of the policy.
Scenario 4: pharmacist is an outpatient pharmacy service, which is outsourced to an independent provider
Is the individual deployed by the registered person for the provision of a regulated activity? NO: the individual is not in scope of the policy.
The pharmacy is regulated by the General Pharmaceutical Council and, as an outpatient pharmacy, is not part of the CQC-regulated activity in the hospital. Since the patient may take their prescription to any pharmacy, this service should be considered as a community pharmacy and out of scope of the policy.
**Please note that workers in inpatient pharmacy services are considered within scope as their roles facilitate CQC-regulated activity in the hospital.
Scenario 5: NHS 111 call handler answers and resolves query from patients
Is the individual deployed by the registered person for the provision of a regulated activity? YES: does the individual have face-to-face contact with patients or service users in their role – this includes entering areas which are utilised for the provision of a CQC-regulated activity which may result in incidental face-to-face contact with patients or services users? NO: the individual is not in scope of the policy.
This worker does not have direct face-to-face contact with patients. As such, the worker is not in scope of the policy.
Scenario 6: service manager whose office is located on a clinical floor in a hospital
Is the individual deployed by the registered person for the provision of a regulated activity? YES: does the individual have face-to-face contact with patients or service users in their role – this includes entering areas which are utilised for the provision of a CQC-regulated activity which may result in incidental face-to-face contact with patients or services users? YES: the individual is in scope of the policy.
While non-clinical, this workers manages a service providing a CQC-regulated activity. As part of their role, they have face-to-face contact with patients/service users. This worker is therefore in scope of the policy.
Scenario 7: finance manager based in a hospital but not located in or near a clinical area
Is the individual deployed by the registered person for the provision of a regulated activity? YES: does the individual have face-to-face contact with patients or service users in their role – this includes entering areas which are utilised for the provision of a CQC-regulated activity which may result in incidental face-to-face contact with patients or services users? NO: the individual is not in scope of the policy.
While non-clinical, this worker is deployed by the registered person for the provision of regulated activity, however they do not have direct face-to-face contact with patients, and as such the worker is out of scope.
*If the worker’s office is based in or near a clinical area and they are likely to have contact with patients and service users (including incidental contact), they will be in scope of the policy.
Appendix 3: New starters
The following has been extracted from the proposed addition to the code of practice – criterion 10 which is subject to the passage of the regulations through Parliament.
The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
The effect of the regulations for different staff based on the date that they are first employed or engaged for the purposes of the regulated activity is described below:
1. Individual is employed or engaged for the purposes of a regulated activity for the first-time during grace period (i.e. between the date the regulation is made and the date on which regulation 4 comes into force)
The employer must ensure that individual is not employed or otherwise engaged for the purposes of a regulated activity after the (the date on which regulation comes into force) unless the individual has provided the employer with evidence that either:
a) the individual meets one of the conditions described above (in paragraph 1); or
b) the individual has been vaccinated with one dose of an authorised vaccine. After a period of 10 weeks from the date that the first dose was administered, the employer will need to ensure that the individual has provided evidence that individual then meets one of the conditions described in paragraph 1.
2. The individual is employed or otherwise engaged for the purposes of a regulated activity for the first time on or after (the date on which reg 4 comes into force).
The employer must ensure that individual is not employed or otherwise engaged for the purposes of a regulated activity unless individual has provided the employer with evidence that either:
c) The individual meets one of the conditions described in paragraph 1
d) the individual has been vaccinated with one dose of an authorised vaccine at least 21 days before the first day of deployment. After a period of 10 weeks from the date that the first dose was administered, the registered provider will need to ensure that individual has provided evidence that individual then meets one of the conditions described in paragraph 1.
Appendix 4: Key recommended actions checklist
| Planning | |
| Establish the roles that are in scope of the regulations. | |
| Identify vaccination status of workers in scope of the regulations and ensure there are clear methods of recording and reporting (including exemptions). | |
| Review staff vaccination data and identify areas of low uptake e.g. in diverse groups or service areas, to help plan targeted communication and engagement actions | |
| Update staff privacy notices and consider how long vaccination data will be retained, in line with data protection law. Update any data retention schedules covering staff data. | |
| Engagement with staff side, speak up guardian and staff Equality, Diversity and Inclusion networks | |
| Complete Equality Impact Assessment (EIA) | |
| Draft action plan – noting key dates for action | |
| Amend/draft vaccination policy and procedure | |
| Form a cross-functional team inclusive of organisational representatives, to drive planning | |
| Plan organisation wide communication and engagement utilising subject expert leaders within the organisation community and across integrated care systems | |
| Engage with contractors, suppliers, bank and agencies | |
| Freeze vacancies that may be suitable alternative employment for redeployment | |
| Consider how roles can be reconfigured to enable the reallocation or restrictions of duties | |
| Amend adverts, offers letter and contract templates to reflect regulation | |
| Preparation | |
| Disseminate vaccination education and information material | |
| Communicate practical information regarding how workers can get their vaccination | |
| Hold staff meetings, webinars and targeted conversations to enable individuals to discuss any queries or concerns they may have. Engage subject experts | |
| Hold supportive 1:1 conversation with staff to address barriers and vaccination hesitancy | |
| Record vaccination status updates (including staff who are exempt from the COVID-19 vaccination) and evidence | |
| Consider if duties can be reallocated and redeployment opportunities | |
| Ensure staff and workers are aware of and have access to health and wellbeing Support | |
