IAPT at 10: Achievements and challenges
To mark 10 years of Improving Access to Psychological Therapies (IAPT), Professor David M Clark, one of the founders of the programme which has inspired similar models across the globe, reviews the growth and successes of this landmark psychological therapy service during its first decade. Plans set out in the NHS Long Term Plan build on the ambitions of the Five Year Forward View for Mental Health, and will see the number of people with anxiety disorders or depression who can access help each year through IAPT increase by an additional 380,000 to reach 1.9 million by 2024.
The Improving Access to Psychological Therapies (IAPT) programme started in October 2008. The National Institute of Health and Care Excellence (NICE) had recently issued clinical guidelines recommending psychological therapies as first choice interventions for depression and anxiety. Patient preference studies showed these recommendations were popular. Psychological therapies were preferred to medication at a ratio of 3:1. However, the public was not getting what it wanted. Very few people with depression or anxiety disorders were being offered evidence-based psychological therapy and waiting lists were inordinately long.
A revolution in mental health
To overcome this problem, the NHS has trained over 10,500 therapists and deployed them in new psychological therapy services. Each IAPT service follows stepped care principles. NICE recommends cognitive behavioural therapy (CBT) for depression and all anxiety disorders, so it is available in all services. NICE also recommends other therapies for depression and most (93%) services provide patient choice. Counselling is the most commonly offered alternative. In a unique exercise in public transparency, IAPT ensures that almost everyone (99%) who has a course of treatment has their anxiety and depression measured at the beginning and end of treatment. Service outcomes are available on public websites (see NHS Digital IAPT reports and Public Health England’s Profiles Tool). Learning from this data has improved understanding of how to best deliver the therapies and has enabled services to progressively improve the help they provide to patients.
Achievements
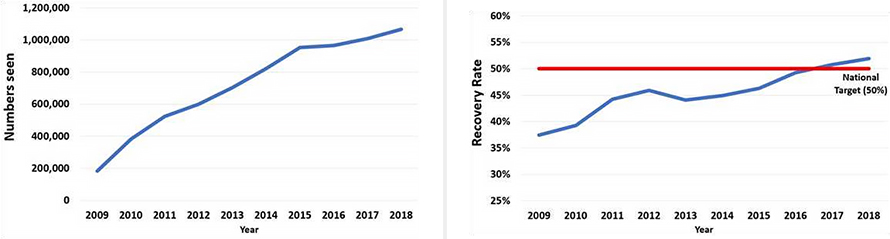
IAPT has grown each year since 2008. It now sees over 1 million people each year. Around 550,000 have a course of therapy. The others receive an assessment, advice and signposting (if appropriate). Waiting times are much improved. The latest data show the average wait to be seen is 19 days. Overall outcomes are good. Approximately, 7 of every 10 people (67%) who have a course of treatment (two or more sessions) show reliable and substantial reductions in their anxiety/depression. Around 5 in every 10 (51%) improve so much they are classified as recovered.
The below charts show the number of people seen in IAPT services 2009 to 2018 and IAPT recovery rate, 2009 to 2018.
Psychological treatments are more difficult to deliver than medication. Some reduction of clinical outcomes might be expected when treatments are delivered in routine services, rather than in the research studies that underpin NICE guidance. However, IAPT aimed for similar results, specifically at least 50% recovery. Initially, this was an elusive target but was achieved in January 2017 and has been maintained each month since. This remarkable achievement is a testament to the skill, tremendous hard work, openness to learning, and dedication of the thousands of clinicians and other staff who work in IAPT services.
International praise
IAPT has attracted favourable international attention. In 2012 an editorial in science journal Nature stated that the programme “represents a world beating standard”. More recently (December 2018) a piece in the Canadian Globe and Mail was headed ‘For better mental-health care in Canada, look to Britain’. Building on the UK model, Norway now has 40 IAPT services. Australia’s New Access for depression and anxiety programme is strongly influenced by IAPT, Stockholm has a very successful IAPT service, and several other countries are developing plans for IAPT-like services.
Future challenges
Despites its successes, IAPT is still a work in progress. Most people suffering from anxiety or depression in the community still do not have an opportunity to access psychological therapy. For this reason, the NHS Long-Term Plan commits the NHS to expanding IAPT so 1.9 million people are seen each year by 2024. That represents around a quarter of the latest prevalence figures for depression/anxiety.
To achieve this expansion, all IAPT services need to increase their workforce. While this is happening, commissioners and service leads will want to ensure the quality standards that underpin IAPT’s excellent outcomes are maintained. To help, NHS England’s IAPT Manual summarizes 10 years of learning and covers all the essential features of an IAPT service. Areas requiring particular attention include:
- adequate doses of treatment,
- reducing waits between initial assessment and subsequent treatment,
- patient choice,
- staff well-being initiatives,
- equal access to IAPT for people with a long-term physical health conditions (LTCs) as well as a mental health problem, and
- capitalizing on developments in digital healthcare.
New integrated IAPT services which bring together physical and mental healthcare are now established in a third of clinical commissioning groups (CCGs) and have greatly increased access to therapy for people with LTCs. Integrated IAPT needs to expand to the whole of England.
Digitally assisted therapies, where patients receive regular support from a therapist but learn many of the key lessons of psychological therapy from online materials, are starting to be used with success and will become a more prominent feature of IAPT. Digital initiatives may also facilitate initial entry into IAPT services and help services more consistently follow-up patients after treatment to help ensure they stay well.