Advice on how to establish a remote ‘total triage’ model in general practice using online consultations
Contents
- Introduction
- How to implement total digital triage
- Start planning
- Support and training
- Make changes
- Using total triage
- Implementing total triage across primary care networks
- Appendix 1: Practical guidance for reception staff in managing workflow
- Appendix 2: Top tips on online consulting
Publications approval reference: 001559
15 September 2020, Version 3
Introduction
In response to the COVID-19 pandemic, NHS England and NHS Improvement have produced this guide to support all general practices in England with the rapid implementation of a ‘total triage’ model using telephone and online consultation tools.
Total triage means that every patient contacting the practice first provides some information on the reasons for contact and is triaged before making an appointment. It is possible to do this entirely by telephone but using an online consultation system is likely to leverage further efficiency and benefit. Total triage is important to reduce avoidable footfall in practices and protect patients and staff from the risks of infection. This information accompanies a walkthrough webinar.
Key messages
- All practices should be using a total triage model to protect patients and staff from avoidable risks of infection.
- All practices must have access to an online consultation system to support triage.
- Patient requests should be triaged wherever possible to decide on what the most appropriate mode of care delivery is for that patient and to enable care to be provided by the right healthcare professional with the right level of urgency.
- Practices should continue to provide remote consultations (online, phone, video) alongside face to face care for those that need it. The approach should be tailored to the person, the circumstance and their needs.
- Information for patients about how they can access services should be clear; with explanation of triage, the modes of communication available to them and reassurance that face to face care always remains available when clinically appropriate and provided in line with the standard operating procedure to keep patients and staff safe.
- There is no one size fits all approach. Adjustments will need to be made to ensure those who are unable to access or engage with services remotely can still access appointments and care. Digital channels should be available alongside other routes to access services (telephone, in-person).
- The number of face-to-face contacts that a patient requires should be minimised by co-ordinating care so that as much as possible is done in a single consultation.
- In general, online pre-bookable appointments should not be used so that all demand goes through triage, however, there may be some exceptions to this – such as flu clinics.
- Practices should continue to encourage use of other online patient-facing services, e.g. repeat prescription ordering and patient access to medical records.
- Appointments made available to NHS 111 for direct booking should be set up as remote appointment slots or as an un-timed ‘worklist’ to enable further clinical review by the practice.
- Implementation resources and capacity are available to ensure practices and primary care networks (PCNs) are fully supported to deliver the changes required for a successful total triage model and optimisation of digital first pathways. These can be accessed by contacting your CCG or your NHS England and NHS Improvement regional team via england.digitalfirstprimarycare@nhs.net
Dr Minal Bakhai | Deputy Director and National Clinical Lead for Digital First Primary Care | NHS England and NHS Improvement | General Practitioner
How to implement total digital triage
In response to the COVID-19 pandemic we have seen an acceleration in the adoption of digitally supported triage (total digital triage) and, where appropriate, the use of remote consultations to maintain safe service delivery and protect our patients and staff.
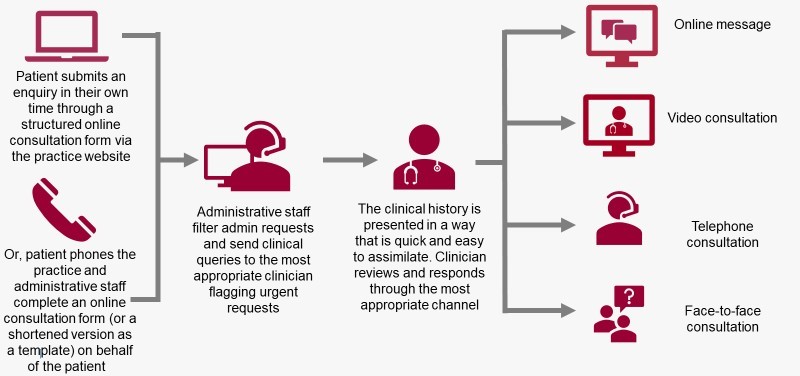
Total digital triage uses an online consultation system to gather information and support the triage of patient contacts, enabling care to then be provided by the right person, at the right time, using a modality that meets the patient’s needs. Non-digital users may be supported by carers or are taken through the same online form or a short template by administrative staff over the telephone or in person (with some agreed exceptions, for example, vulnerable patients). Practices are then able to manage demand via a single workflow, prioritising care based on need, rather than on a first come, first served basis. This approach helps to ensure equity of access for digital and non-digital users. It can also free up the phone lines for those who cannot or choose not to go online. Digital channels are an additional way of supporting patients and should be used to augment traditional models of care delivery , providing increased choice for patients in how they interact with their general practice.
With a need to minimise footfall in practice and reduce the risk of infection, the relative advantage of remote consultations has changed dramatically. Data suggests that practices using total digital triage were better able to respond flexibly to variations in demand for care during the initial stages of the pandemic (The Health Foundation, July 2020).
Data also show that digital triage systems can enable about a third of all patient requests to be closed with an electronic message (askmygp. Consultation use data issued by askmygp 2020). The online consultation system captures the patient’s history and symptoms asynchronously (completed by the patient in their own time), allows patients to send pictures and offers signposting to self-help or local services. The systems increase resilience by enabling more adaptable working patterns (i.e. customised appointment lengths) and giving staff more control over managing their time and workloads (e.g. prioritising activities to maximise use of resources/capacity and working flexibly). Staff working remotely (e.g. if they are self-isolating) can use digital triage systems from home. Research shows online (written) consultations can remove barriers for some people traditionally marginalised from access to general practice, including those with a physical disability, hearing loss, carers and people who feel apprehensive about accessing health services – e.g. for a mental health, sensitive or embarrassing problem.* ** However, there is ‘no one size fits all’ and a blended approach to communication should be offered and matched to the patient and their needs.
*Atherton et al (2018) Alternatives to the face-to-face consultation in general practice: focused ethnographic case study.
**Atherton et al (2018) The potential of alternatives to face-to-face consultations in general practice, and the impact on different patient groups.
This is the recommended model for practices to move to, enabling requests to enter through a single workflow and matching the approach for providing care to the person, the circumstance and their needs.
Moving to a total triage model may represent a significant change in how a practice or PCN functions. To deliver any change like this successfully, it is essential to consider organisational culture and to support people through the change process. Resilience resides in teams, particularly in complex and ambiguous times. It is important to remain flexible and supportive of one another in order to realise benefits and build effective new ways of working.
Summary
| Plan |
|
| Support |
|
| Change |
|
| Use |
|
All practices must have access to an online consultation (OC) system to support total triage. Many practices already have OC systems but may have used them only for a small proportion of patient contacts. This guide will help you to use your OC system to manage your entire workflow.
If there is no OC system in your practice, please contact your commissioner for advice. Commissioners should contact their NHS England and NHS Improvement regional digital team or contact the commercial procurement hub. For more information on procurement, funding and assurance of supplier* systems see here.
*For clarity, the term ‘supplier’ in this guidance refers to your online consultation supplier.
For information on the different types of online consultation system, see the summary implementation toolkit section on getting started.
NHS England and NHS Improvement have produced templates and resources to help practices and commissioners safely implement and optimise the use of online and video consultation systems. Clinical safety risk management is a joint responsibility of commissioning and deploying organisations, and the resources developed give advice on how CCGs and practices should work together to mitigate risk and clarify the responsibilities of commissioners and practices according to the route of procurement.
Start planning
| Practice planning |
|
| Cultural change |
*Get Digital Heatmap and the Consumer Data Research Centre map of neighbourhoods **Video consulting – a quick guide for patients and Health at Home campaign |
| Capacity planning |
|
| Workflow redesign |
*A data collection template may be provided by your OC supplier **VC: SNOMED CT ID = 325921000000107 (consultation via video conference) and OC: SNOMED CT ID = 32591100000010 (consultation via multimedia encounter type) |
| Continuity of care |
Clinicians may update the record if they decide the patient needs reallocating after a consultation. Alternatively, some practices use a personalised list. |
Support and training
| System resilience |
|
| Training |
|
| Trying it out |
|
Make changes
| Change your appointment system |
|
| Adapt staff rotas |
|
| Update the practice website and telephone messages |
|
| Update other communication methods with patients |
* Online Centres Network, Barclays online resources, AgeUK resources ** Get online @ home – access to low cost computers, laptops and tablets *** Learn my way – signpost those with access to IT but lacking in confidence or skills to free courses on how to use the internet. |
| Information and clinical governance |
|
Using total triage
| Going-live |
|
| Monitoring |
|
Implementing total triage across primary care networks
Collaboration between practices, primary care networks (PCNs) and community services has supported sustainability of services as pressure on the health system has escalated. Setting up a virtual hub offers practices the opportunity to share staff, resources and workload (both administrative and clinical) within their PCN(s) and wider. Remote consultations could be managed centrally by a group of clinicians working on behalf of the PCN(s), provided there is appropriate technical infrastructure. Clinicians need to be able to triage and consult as if they were physically present in a GP practice. Record sharing and smart card access should be enabled across PCNs/sites if it is not already.
For resources on virtual hubs see the online consultations implementation toolkit section on the eHub under practice implementation (page 52).
Appendix 1: Practical guidance for reception staff in managing workflow
| 1 | When patients make contact
|
| 2 | Doing the signposting
Agree who and how often staff will monitor either a dedicated inbox or the online system for incoming online requests. Admin staff should go through incoming online requests, validate the patient’s details against the clinical record and take the following steps:
|
| 3 | Clinician triages the request and responds to the patient using the method that best meets their needs (online, phone, video, face to face)
Due to the risks of COVID-19, the current recommendation [GP Standard Operating Procedures, August 2020] is that all requests are triaged by a member of the practice team first to manage any infection risk before a face-to- face appointment is offered. |
Appendix 2: Top tips on online consulting
1. Aim to respond promptly
Experience shows that a prompt initial response to clinical requests, ideally within two hours (as opposed to an ‘end of next working day’ response), even if it is simply letting the patient know their consultation is being reviewed, leads to greater patient satisfaction, safer identification of urgent problems and avoids duplicating work (such as failed encounters, the patient calling the practice thinking they have been ignored, or trying to bypass the system). Some forms allow practices to communicate bespoke response times for different types of queries. Set expectations that are feasible and according to safe clinical thresholds.
2. Don’t be daunted if you see a lot of requests
A list of OC requests can usually be done very quickly. Use messaging where possible. If arranging a face-to-face review, consider whether it will change the intervention – discuss dilemmas with colleagues and make decisions collectively. If phoning patients or using video, make use of all the information available. Provide a precise time window for appointments so patients can prepare and find a quiet, safe and private location for the consultation, provide the name of the clinician who will be calling and let patients know if there is a delay. We have learnt that you can save a lot of time by:
- trying to avoid repeating data collection and instead summarising the information you have and clarifying if anything has changed or checking specifics
- arranging next steps remotely when possible (eg requesting 2-week wait referrals where indicated)
- asking patients to use online/remote consultations for follow-up (consider scheduling a diary entry as a safety net)
- keeping calls short if it becomes clear that a face-to-face review will be needed
- following up with a short summary or link to key points via an electronic message
3. When communicating with a patient online
- Be clear about who is responding – e.g. give your name and role in the practice and be clear if admin staff are responding on behalf of a clinician.
- Check the patient’s understanding of management plans and provide appropriate safety netting with specific instructions that the patient can refer back to.
- Make sure patients are told how they can ask questions, query a decision or discuss something further.
- Before sending clinical information by SMS, ask the patient if they are happy with this mode of communication (but avoid using this route for sensitive or urgent issues).
- Consider the wording of messages and how this may be received by the patient – think ‘how would I feel if I got this response?’
- Be alert to written cues: e.g. you might be able to identify a patient’s concern through the language they use.
- Avoid jargon and acronyms, use large text, keep sentences short. Structure your response.
- Provide information and/or a demonstration (e.g. via online videos or champions) for patients on using the online and/or video consultation system including a code of conduct. Guidance should include advice on what to do if the technology is not working. Receiving information in advance helps patients feel prepared and supported.
4. Pass the online consultation to the patient’s regular clinician
- If the request is non-urgent, pass it to the patient’s usual clinician.
- If a patient later requires a further consultation, pass this to the clinician who originally dealt with the online consultation.
5. Quick wins
- Add links to advice on NHS.uk, send attachments or digital leaflets to your messages.
- Use pre-set messages or questions that you can customise.
- Code using templates provided by suppliers.
- Update any outstanding QOF items.
6. Try to do today’s work today
- If a patient needs to be contacted, book this for the current session rather than a future date wherever possible (also consider continuity). This is more sustainable than having a surge of appointments later.
Resources
- FutureNHS digital community and resources
- Video consultation guide for general practice, GPs and patients
- NHSx Information governance guidance
- Demand and capacity tool
- Principle for supporting high quality consultations by video in general practice during COVID-19
- Key principles for intimate clinical assessments undertaken remotely in response to COVID-19
- Health Education England e-resource on remote total triage model in general practice
- Online consultations implementation toolkit
- Digital Devon Accelerator pack (includes communication examples)
- Training video: good and bad online consultation
- Remote assessment of COVID-19
- NHSE/I Digital First Primary Care webinar recordings
- Clinical safety and information governance templates
- Q&A on procurement, funding and assurance
- More accurate general practice appointment data guidance
- Public facing Health at Home campaign
- Digital inclusion for health and social care
- Example appointment templates one and template two
