Deploying the healthcare science workforce to support the NHS clinical delivery plan for COVID-19
Contents
- 1. Introduction
- 2. Principles
- 3. Redeploy healthcare science staff to support critical care, high dependency units and those on oxygen therapy
- 4. Regulation and indemnity
- 5. Staffing scope and competencies
- 6. Cross-cutting teams in critical care and HDU: contribution of healthcare scientists
- Appendix 1: COVID-19 testing: laboratory competency-based training requirements
- Appendix 2: Potential cross-skilling and upskilling for HCS
- Appendix 3: Self-assessment competency reporting framework for laboratory staff
- Appendix 4: Self-assessment competency reporting framework for physiological sciences staff
- Appendix 5: Self-assessment competency reporting framework for physical sciences staff
- Appendix 6: Bedside clinical experienced workers
- Appendix 7: Opportunities to deploy healthcare science staff
Classification: Official
Publication approval reference: 001559 / C0143
12 May 2020, Version 3 with updates highlighted in yellow
This is a working document created during an evolving situation. It will be updated based on emerging experience.
1. Introduction
This document has been produced to assist trusts and other organisations in deploying the healthcare science (HCS) workforce in the surge response to coronavirus. It sets out how healthcare scientists support these areas and the issues that need to be addressed, with detailed advice broken down by professional area. It builds on work already being undertaken by HCS staff across the NHS to adapt to the challenges posed by COVID-19
Specifically, this guidance is to support the provision of:
- new and expanded roles for specialists in healthcare science
- proactive leadership by HCS Leads, which is crucially important to ensure the HCS workforce is fully embedded in all planning and delivery stages
- troubleshooting to help individuals work in environments where they will have to adapt rapidly, as well as alter allegiances to individual trusts, departments and management structures
- COVID-19 molecular testing in laboratories using staff who have the potential skills and experience
- expertise and support for critical care and high dependency settings
- clinical engineering services to support crucial logistics and equipment operation and maintenance in laboratories, critical care and high dependency settings
- physical science services to support and coordinate regional equipment procurement, logistics, compliance with regulation, equipment assessment, installation, acceptance and maintenance in both the laboratories and in critical care settings
- ongoing healthcare science diagnostic and treatment services, which must continue to be maintained for urgent and emergency care pathways including cancer, dialysis, and acute cardiac events.
This guidance defines:
- the skills that exist across all HCS specialties, to help identify those who could quickly be upskilled to take on different roles and activities
- the required competencies for upskilling
- recommended training resources.
Who belongs to the HCS workforce?
There are over 50 healthcare science specialties and 4 major sections of the workforce – Laboratory (Life) Scientists; Physiological Scientists; Medical Physicists and Clinical Engineers; and Clinical Bioinformaticians. Healthcare scientists work in direct patient care and other indirect roles, either providing information for, or being part of multi professional teams. Healthcare scientists start to specialise early in their careers so although some will work with acutely unwell patients with cardiac and respiratory conditions or work in areas such as theatre, critical care or high dependency units, a large number may have not encountered an acutely unwell patient with severe respiratory problems.
Highly skilled Vascular, Cardiac and Neuro Physiologists can be redeployed to support their Respiratory Physiology colleagues managing COVID-19 patients working within critical and high dependency care teams and supporting direct patient care, with others back-filling for those that are re-deployed. Laboratory (Life) Scientists may be re-deployed to COVID-19 testing in microbiology/virology laboratories, with training provided where needed, provided this does not compromise other essential laboratory services. Medical Physicists and Clinical Engineers will be essential in ensuring all equipment, including mechanical ventilators, are safe for use and maintained. They will also be critical in setting up field hospitals.
It should be noted that a proportion of the healthcare science workforce (students/trainees) are in different types of undergraduate and postgraduate training and are following curricula set by the National School for Healthcare Science or the professional bodies. It is important therefore to consider not only the specialty, but also the stage of training. In addition, some of the healthcare science workforce will be relatively junior; others will have worked in the NHS for a decade or more. Nonetheless, the full range of people working and training in healthcare science should be available for deployment as patients and the services demand
Working differently
The anticipated surge of coronavirus patients will require increased critical care/HDU beds and laboratory testing capacity. Existing staff may have to work in significantly and fundamentally different ways to help to respond to service demands, including responding to the potential high levels of staff absence. In addition, staff with related skills, but limited knowledge of these services, will need to be re-deployed from other areas into these critical care/HDU and testing services.
A regular review of staffing is therefore needed, to support changes in working practice and staff movement from other areas, while keeping patients safe. The HCS workforce will make a major contribution in both areas.
There will also be a requirement to support patients in community and social care who have had COVID-19 and have been discharged from hospital but still requiring support, in addition to adapting services to work with those at risk of acquiring COVID-19 infection. It is also necessary to recognise there will be a need for end of life care and bereavement support across the care continuum, which parts of the HCS workforce could support.
Practical implications for the HCS workforce during the COVID-19 pandemic
Existing hospitals and healthcare facilities are working to expand their critical care/HDU and laboratory capacity. Healthcare Scientists within these areas are already engaged in planning and carrying out activities to support this expansion, as are Healthcare Scientists in the services that support them. All these staff are having to work differently under intense pressure as hospitals reconfigure their services in response to the pandemic.
New facilities (‘Field Hospitals’) are being set up in locations across the country and require significant HCS input. For example, the new Nightingale Hospital in London being the first to be commissioned with expert leadership and skills from healthcare scientists in laboratory (life) science, clinical engineering, respiratory physiology, cardiac physiology and vascular science.
Guidance for employers
Guidance has been collated by the Department of Health and Social Care, NHS England and Improvement, Public Health England, Health Education England and NHS Employers in collaboration with NHS Staff Council, so that the latest advice is available to employers in one central resource. This guidance has also been shared with colleagues from the main health unions and staff organisations, to ensure that this is a supportive and co-ordinated response. Please see link below for guidance:
In particular this includes advice on how to care for staff health and well-being whilst working so differently and longer hours:
https://www.nhsemployers.org/covid19/health-safety-and-wellbeing/staff-wellbeing-and-support
HCS staff who are redeployed should not be disadvantaged in pay, terms, conditions and status and there must be acknowledgement that the redeployment is a temporary change rather than a permanent change.
2. Principles
Safe for staff and patients:
- Staff will likely be working in new ways with expansion/adaptation of physical facilities and flexible working patterns, including collaboration and excellent team working with other staff groups.
- COVID-19 testing is crucial and will be increased at pace in the coming days and will have to be on-going and sustained. COVID-19 Testing Competency Based Training Requirements can be found in Appendix 1.
- The potential for cross-skilling and upskilling of healthcare science staff is found in Appendix 2. Ideally all redeployed staff should self-assess their competence to perform the required tasks (under supervision initially) to confirm their suitability. An example framework is given in Appendix 3.
- All staff who may be required to wear Personal Protective Equipment (PPE) should be trained within their place of work in the procedures of ‘donning and doffing’ PPE.
- Staff should be aware of and trained in excellent infection control practices, ensuring that local guidelines and practices are adhered to.
- https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control
- Returning HCSs should also self-assess according to their competence, which may depend on their length of time away from practice. They will be placed initially on the basis of this assessment, recognising that their competences may quickly improve after a return to practice.
- Staff should ideally not be removed from roles which would leave urgent or emergency non-COVID-19 pathways understaffed or with inexperienced staff e.g. providing diagnostic or therapeutic HCS services for patient within a cancer pathway, acute cardiac pathways or home dialysis. This will need to be kept under review locally as “shelved” services are re-established or re-ramped.
- When taking redeployed staff into a service consideration should be given to the impact on routine staff of the need for additional training and supervision of the inexperienced colleagues.
- Staff who move to new areas, to work alongside existing staff, may be at high personal physical and mental health risk. Local teams should consider how they can support all their staff working in challenging circumstances and unfamiliar environments.
- Induction, rota management and training by employers must include: PPE training (face-to-face/simulation), basic life support (online) and induction/orientation to their working environment.
- The guideline https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/ provides information for healthcare professionals looking after pregnant patients with severe coronavirus infection.
Efficient:
Use designated teams, outlined in the cross-cutting teams section, to deliver routine tasks for whole wards or hospitals.
All staff should have their role clearly defined and identifiable (including while wearing PPE), to facilitate communication and appropriate distribution of tasks.
Patient-centred care:
Every staff member has a responsibility to contribute to patient care, as part of the wider laboratory or clinical care team, according to their competency and ability to do so. They should not, however, feel pressured to undertake tasks for which they are not competent.
www.ahcs.ac.uk/2020/03/06/statement-of-accredited-registers-about-covid-19-coronavirus/
3. Redeploy healthcare science staff to support critical care, high dependency units and those on oxygen therapy
Below is a list of healthcare scientist professions who can make a valuable contribution to critical care teams caring for COVID-19 patients. Where required, we are seeking permissions nationally for these professional groups to work outside their normal scope of practice:
Many from the HCS workforce may be redeployed in critical care roles, eg Respiratory Scientists, Cardiac Scientists, Neurophysiological Scientists, Perfusionists, Vascular Scientists, Critical Care Scientists, Medical Physicists and Clinical Engineers. Some specific examples include:
- Respiratory Physiologists who are routinely delivering Sleep Services and Nasal Ventilation Support Services can be utilised in acute Nasal Ventilation and Mechanical Ventilation.
- Cardiac Scientists in cardiac theatres, whose work may be scaled down significantly, can be released for additional duties in critical care, helping to support ventilated patients
- Perfusionists with theatre and critical care experience can support critical care teams, especially with ventilation requirements.
- Clinical Engineers/technologists will support the expansion of critical care departments into new environments, assist with equipment validation and operation and the rapid application of new techniques in both clinical care and where required, in the laboratories.
- Clinical Engineers/technologists can be upskilled in basic critical care techniques, such as blood gas analyser support.
- Renal Technologists can support Clinical Engineering.
- MRI Physicists can support Radiation Safety or Clinical Engineering.
- Medical Physicists could also help assist with equipment and preparation teams.
- Neurophysiologists could be reskilled to work in a critical care science setting, their skills may be utilised to aid prognostication testing.
- Respiratory Scientists and Cardiac Scientists with additional training, can also perform arterial blood gases.
- Cardiac Scientists and Vascular Scientists can undertake patient monitoring and diagnostic techniques, e.g. ultrasound studies, pressure monitoring.
- Genetic Counsellors, Audiological Scientists, Gastrointestinal Scientists, Reproductive Medicine Scientists and Urodynamic Scientists can support communications with patients and relatives and sustaining the wellbeing of staff who are working as part of the critical care team. Where the HCS workforce are not being deployed into expanded roles, those designated as Healthcare Science Clinically Experienced Worker will contribute to the thousands required to support service expansion.
Health and wellbeing
We do not yet know how long COVID-19 emergency support provision will need to be sustained. It is essential that staff receive support from their employer and have access to tools to ensure they can maintain good health and wellbeing. Local support mechanisms should be made readily available, and a range of additional resources can be found here (https://people.nhs.uk/).
NHS Employers – free access to wellbeing Apps for all NHS staff
A mental health platform that empowers staff to proactively improve their mental wellbeing
- Sign up with your NHS email address
Download the Unmind App from your AppStore – your organisation name is NHS.
Science-backed mindfulness and meditation, app providing unique tools and resources to help reduce stress, build resilience, and aid better sleep.
Click the link above for NHS staff access and select either the clinical or non-clinical staff option.
Use your NHS email address to sign-up.
Sleepio is a clinically-evidenced sleep improvement app, using cognitive behavioural techniques to help improve poor sleep.
Daylight is a smartphone-based app and provides help to people experiencing symptoms of worry and anxiety.
A range of free and paid for apps that have been assessed against a range of NHS standards are also available at the link above.
Other useful resources
- PHE – Guidance for the public on the mental health and wellbeing aspects of coronavirus
- Intensive care society: wellbeing library
- World Health Organisation – Coronavirus mental health considerations
- Mental Health Foundation – coronavirus
- Every mind matters
- Mind – Coronavirus and your wellbeing
4. Regulation and indemnity
Staff should work within their usual frame of competence and experience but may have to work outside their usual teams and hierarchies adhering to the principles of the joint statement from the professional regulators:
In addition, the emerging model from the development of the new Nightingale Hospital is that new hospitals being urgently developed in response to the COVID-19 pandemic will be absorbed into an existing local Trust, as an additional site, and follow their governance models and professional leadership. All staff redeployment will be managed by HEE, who will implement secondment agreements and employment contracts as part of the process.
Mechanisms of regulation for healthcare scientists
Within the UK there are two mechanisms to regulate healthcare scientists; by a statutory regulator, Health and Care Professions Council (HCPC), as a clinical scientist, biomedical scientist or hearing aid dispenser, and for the remaining healthcare scientists regulation is via voluntary registration on a register held by one of the following organisations, the Academy for Healthcare Science (AHCS), the Institute of Physics and Engineering in Medicine, Register of Clinical Technologists (RCT) or the Registration Council for Clinical Physiologists (RCCP).
Statutory register
Following an official request from the UK government, and the passing of the Coronavirus Act 2020, professional regulators have enacted emergency powers to temporarily register those who have recently left their profession. The process for returners differs between professional groups. Specific information for each profession can be found at https://www.england.nhs.uk/coronavirus/returning-clinicians/. The Health and Care Professions Council (HCPC) has created a temporary register and automatically re-registered all clinical scientists and biomedical scientists who voluntarily left the register in the last three years. https://www.hcpc-uk.org/covid-19/temporary-register/. Those who have chosen to return to work and are temporarily registered will be contacted by the regional teams who undertake basic screening and pre-employment checks. Healthcare scientists offering to return to the workforce are also invited to complete an online skills survey. Once these checks are complete, details are forwarded to employers so that individual professionals can be deployed where their skills are most in need.
Voluntary registers
- There are three organisations that hold registers which have been accredited by the Professional Standards Authority (PSA) that healthcare science professionals can join if they meet the required criteria: The Academy for Healthcare Science (AHCS), Register of Clinical Technologists (RCT) and Registration Council for Clinical Physiologists (RCCP).
- The Academy for Healthcare Science (AHCS), the Institute of Physics and Engineering in Medicine (IPEM) and the Registration Council for Clinical Physiologists (RCCP) have been working together to establish a Shared Temporary Register (STR) for healthcare science practitioners. The STR is open to final year healthcare science students across the UK, who meet the agreed criteria, and allows them to practice as registered professionals within the healthcare science workforce. This supports the public health response to the COVID-19 epidemic.
- There is no fee to join the STR and joining is voluntary.
- The STR is for the duration of the COVID-19 emergency and AHCS, IPEM and RCCP will make a joint decision about when it is appropriate to close the STR, considering advice from the administrations in the four home countries and any decision to close the temporary registers held by statutory regulators.
- A more detailed joint statement, including the criteria for eligibility and how to join the STR can be found at: https://www.ahcs.ac.uk/education-training/
- The AHCS, IPEM and RCCP are working with the relevant universities to identify eligible students and gather details to be included in the STR.
- The register will be co-ordinated by the AHCS on behalf of all three organisations and will be available via the AHCS website.
All the registration bodies have agreed there will be no fee for entry onto their temporary registers.
Indemnity: COVID-19 NHS Indemnity
Due to the ever-increasing pressure on our NHS during this time, employers have asked for clarity regarding the application of the Clinical Negligence Scheme for Trusts (CNST) during the deployment of clinical staff to other departments, roles and clinical duties as a result of COVID-19.
NHS Resolution indemnifies those NHS organisations which are members of its schemes for clinical negligence through the NHS (Clinical Negligence Scheme) Regulations 1996. Clinical negligence defined as “a liability in tort owed by a member [NHS organisation] to a third party in respect of or consequent upon personal injury or loss arising out of or in connection with any breach of a duty of care owed by that body to any person in connection with the diagnosis of any illness, or the care or treatment of any patient, in consequence of any act or omission to act on the part of a person employed or engaged by a member in connection with any relevant function of that member”.
We have received confirmation from NHS Resolution that clinical staff at NHS trusts in England will still be protected by the CNST if they are deployed to a new area of work at the trust, including one which is outside their normal speciality, or at a different trust, during the pandemic. Under section 11 of the Coronavirus Act 2020, the government will provide indemnity for clinical negligence liabilities associated with Coronavirus which are not covered by alternative indemnity arrangements such as those provided by the CNST, insurance companies or medical defence organisations.
NHS Resolution is reassuring all NHS employees (and honorary contract holders) that levels of protection and indemnity will continue to be in place through this time. Volunteers, including retired returners and deployed students and trainees, who have been sourced by NHS Trusts to assist with the delivery of clinical services, will also be covered by these schemes.
NHS Resolution has set out its position on its website, making it clear that indemnity arrangements should not be a barrier to changed working arrangements during the pandemic (https://resolution.nhs.uk/2020/03/19/covid-19-and-business-continuity/).
A joint letter on clinical negligence indemnity sent from the Department for Health and Social Care, NHS Resolution, and NHS England and NHS Improvement to all healthcare professionals, and others working in the NHS in England, can be found here https://resolution.nhs.uk/wp-content/uploads/2020/03/20200402-Tripartite_Indemnity_letter.pdf
5. Staffing scope and competencies
Category A: Qualified clinical scientists, biomedical scientists, and healthcare science practitioners, including mortuary (anatomical pathology) practitioner
Laboratory (Life) Sciences
- Virology, Microbiology, Molecular Pathology, Genetics and Genomics undertaking COVID-19 testing
- All specialisms undertaking urgent laboratory investigations
- Quality systems support for the delivery of all tests at the point of care.
- Decontamination Science supporting all clinical and laboratory areas
- Genomic Counsellors supporting clinical teams and patients in communication
- Mortuary services (Anatomical Pathology)
Physical Sciences
- Medical device risk management and governance: optimisation of medical device effectiveness and efficiency, equipment acquisition, installation, management, modification, availability and dissemination of information
- Radiotherapy Physics, Radiation Physics, Imaging with Ionising and Non-Ionising Radiation undertaking urgent diagnostic testing and treatments
Physiological Sciences
- Critical Care Science, Respiratory Physiology, Neurophysiology, Cardiac Science, Vascular Science, Perfusion Science as team members in Critical Care Settings
- All specialisms undertaking urgent diagnostic investigations
Clinical Bioinformatics
- Physical Sciences managing advanced networked computerised medical devices as part of therapeutic, diagnostic or patient monitoring functions, specification and procurement of complex equipment and software, design and, where appropriate, write bespoke software, management of complex patient data
- Health Informatics Science protecting patients (e.g. prevention and avoidance of errors and adverse incidents), support efficiency, specialist analytical interpretation
Category B: Healthcare Science Staff in Training to become Clinical Scientists, Biomedical Scientists and Healthcare Science Practitioners: to be team members or support staff working in:
- Laboratory (Life) Sciences
- Physiological Sciences
- Physical Sciences
- Clinical Bioinformatics
Category C: Healthcare Science Support Staff: Healthcare Science Associates and Healthcare Science Assistants as team members or support staff working in:
- Laboratory (Life) Sciences
- Physiological Sciences
- Physical Sciences
- Clinical Bioinformatics
Category D: Clinical Academics with Healthcare Science or Life Sciences experience, especially those with Category 3 and PCR experience
Many clinical academics are being asked, or requesting, to return to clinical/diagnostic duties to support patient care. Further information can be found at: https://www.rcplondon.ac.uk/news/clinical-academics-and-covid-19
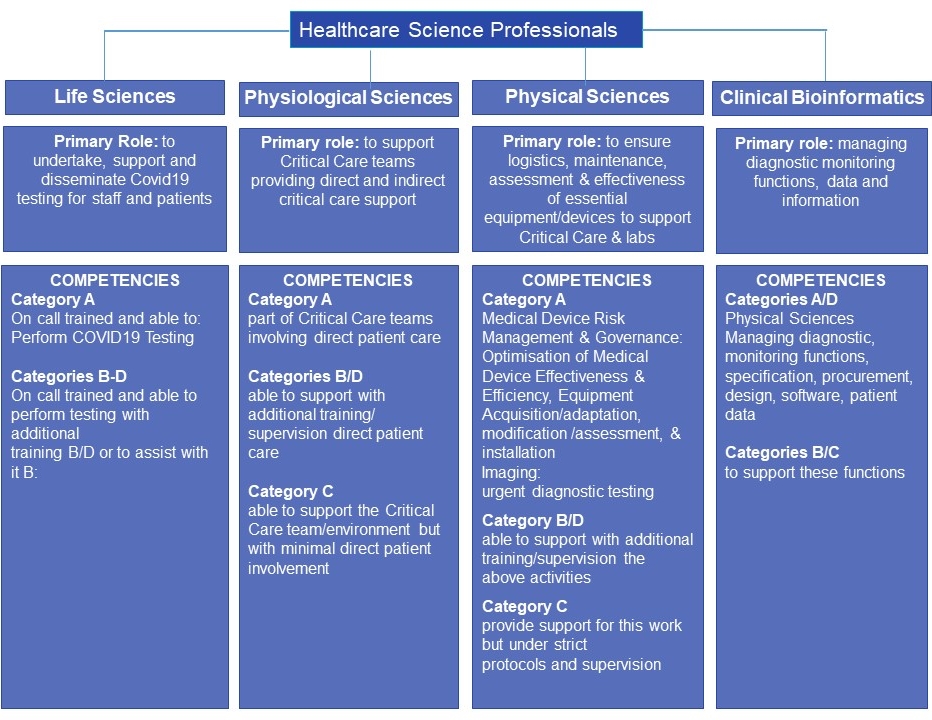
The diagram below shows the structure of the Healthcare Science Profession and their primary roles/competences during the COVID-19 outbreak. There will also be the need for on-going tests/evaluations to support patients who do not have COVID-19 but other medical needs.
6. Cross-cutting teams in critical care and HDU: contribution of healthcare scientists
This section advises on proposed team structures and numbers. The number of teams within a particular unit (ward or hospital) will depend on the size of the unit and should be reviewed daily, alongside projected patient figures based on local modelling data. The contribution of healthcare scientists is highlighted
| Cardiac arrest team: one per hospital | |
| Staff | Usual staffing No other responsibilities |
| Role | Cardiac arrest calls ONLY (2222) |
| Transfer team: one per hospital | |
| Staff | Transfer competent anaesthetic trainee Porter Anaesthetic assistant (ODP, theatre nurse) |
| Role | Transfers to and from radiology, ED, between wards etc |
| Lines team: one per ‘unit’ of 30+ critical care patients | |
| Staff | Line insertion: any of the following Surgeon; Interventional Radiologist; Interventional Cardiologist; Renal physician Vascular access nurse* * Vascular access nurses can help with some of these tasks dependant on competency Assistant: Medical student; HCA, Respiratory, Cardiac and Vascular Scientists and other Physiological Sciences Scientists |
| Mobile emergencies rapid intubation team (merit): one per hospital | |
| Staff |
Range of healthcare scientists e.g. Clinical Engineers, Medical Physicists and Physiological Scientists as well as helping with replacement lines |
| Role |
|
| Role |
|
| Critical care outreach team: one per hospital | |
| Staff |
|
| Role |
Seeing critically ill referrals – inpatient and ED
Escalation of care decisions
|
| Palliative care team: one per hospital | |
| Staff |
|
| Role |
|
| Proning team: one per unit of 30+ patients | |
| Staff | Lead: Senior anaesthetist Team: 4 people who have undertaken the relevant training from any of the following groups Surgeons who regularly position patients Other members of staff with manual handling training Healthcare Science Physiologists |
| Role | Ensure safety of the airway and management of infusions, lines etc. Coordination of team Manual handing of patient under the direction of the lead Sourcing of pillows, slide sheets etc. |
| Pharmacy care team: one per unit of 30+ patients | |
| Pharmacy technician Pharmacist Double checking of drugs with other staff members Monitoring of stock levels and ordering of drugs Assistance with drug preparation |
|
| Equipment and preparation team: one per hospital | |
| Staff | Team leader: OPD, Anaesthetic nurse, Clinical engineer with the assistance of one of the following
|
| Role | Preparation of grab bags – non-drug items (clean roles) Preparation of equipment packs (clean roles) e.g. Intubation, lines, PPE Stocking up of the bed spaces (dirty role) |
| Renal support team: one per hospital | |
| Staff | Renal Nurses Renal Technicians Urodynamic Physiologists |
| Role | Setting up of RRT Troubleshooting issues RRT Central and arterial blood sampling |
| Comfort/hygiene team: on per unit of 30+ critical care patients | |
| Staff | Supervision by a critical care nurse for intubated patients Bedside buddy plus two of:
|
| Role | Supports the bedside buddy with turning washing etc. |
| Runners: one per unit of 30+ critical care patients | |
| Staff | Porters HCAs Medical students< Nursing students< Dental nurses Healthcare Science support staff Equipment Library staff (where available) |
| Role | Transport of bloods and Arterial blood gases Fetching of equipment |
Appendix 1: COVID-19 testing: laboratory competency-based training requirements
Background
- Training and Competencies needed for workforce groups such as BMSs from other Pathology disciplines e.g. Blood Sciences, to be transferred into Microbiology/Virology Departments to support COVID-19 testing;
- HCSs from other specialisms e.g. Genomics, Reproductive Medicine, to be transferred into Microbiology/Virology Departments to support COVID-19 testing;
- Other non-scientific NHS HCS and other Multidisciplinary workforce e.g. Dental, Research Staff to be transferred into Microbiology/Virology Departments to support COVID-19 testing.
The e-Learning for Health (e-elf) website https://www.e-lfh.org.uk has developed COVID training in a number of areas. These are free and registration is not required. Mandatory Training modules are also available which require registration. HCSs might find it helpful to register for an NHS on-line learning resource in order to track and record their learning.
| Training resources | Competencies required | |
|---|---|---|
| Health and Safety | ||
| Basic Infection Prevention Control |
|
|
| Laboratory Health and Safety including donning and doffing of Personal Protective Equipment (PPE) |
|
|
| Sample Reception | ||
| Unpacking High Risk Samples | M-924 LF – Molecular Training Manual for BMS & MLA
|
M-77 Competency assessments:
|
| Booking in Samples | ||
| Preparing Samples for Pre-analytical testing | ||
| Storing High Risk Samples | ||
| Setting Up Extraction of RNA/DNA | ||
M-924 LF – Molecular Training Manual for BMS & MLA
|
|
|
M-924 LF – Molecular Training Manual for BMS & MLA
|
|
|
| Compiling Results | ||
M-924 LF – Molecular Training Manual for BMS & MLA
|
|
|
| Writing Reports |
||
M-924 LF – Molecular Training Manual for BMS & MLA
|
|
|
| Reporting Results |
||
M-924 LF – Molecular Training Manual for BMS & MLA
|
|
|
Appendix 2: Potential cross-skilling and upskilling for HCS
The e-Learning for Health (e-elf) website has developed COVID training in a number of areas. These are free and registration is not required. Mandatory Training modules are also available which require registration. HCSs might find it helpful to register for an NHS on-line learning resource in order to track and record their learning.
| Tasks | Competence | Cross-skilling | Upskilling | Potential training resources |
|---|---|---|---|---|
| General Skills | Infection control, cleaning | All specialisms | E-Learning for Health Infection Prevention and Control – Level 1
GOV.UK: infection prevention and control Infection Prevention and Control – Level 2 Infection Prevention |
|
| Handwashing | All specialisms | NHS handwashing guide | ||
| Corona virus Guidance | All specialisms | NHS England coronavirus guidance | ||
| Healthcare support worker tasks | Physiological Sciences | All other specialisms | ||
| Audit, research and development | All specialisms | |||
| Non-critical care staff: Emergency Induction for non-critical care staff working in Critical Care to support the escalation process in times of surge | Critical Care Science Cardiac Science Respiratory Physiology Clinical Perfusion |
Non-Critical Care Staff in Critical Care Emergency Induction
Quick Look Procedure Resource for NON-CRITICAL CARE staff Safe Alarm Setting in Critical Care Areas |
||
| General patient care | Gathering a patient history | All Specialisms | ||
| Administer Appointments | All Specialisms | |||
| Communicate Information to Authorised Personnel | All Specialisms | |||
| Accessing, Registering and Inputting patient data into digital systems | All Specialisms | |||
| Maintain Stocks of Resources, Equipment and Consumables | All Specialisms | |||
| Prepare and support Individuals for Healthcare Activities | All Specialisms | |||
| Public Health Measures for COVID-19 | All Specialisms | London School of Hygiene and Tropical Medicine: coronavirus online short courses | ||
| Patient Care | Critical Care Setting | Critical Care Science | Cardiac Science Clinical Perfusion Clinical Engineers |
Select ABCDE |
| PPE Donning and Doffing | Critical Care Science Cardiac Science Respiratory Physiology |
All other specialisms | E-Learning for Health YouTube video |
|
| Removal and disposal of PPE | Critical Care Science Cardiac Science Respiratory Physiology |
All other specialisms | E-Learning for Health YouTube vide0 |
|
| PPE Assess and teach Donning and Doffing | Critical Care Science Cardiac Science Respiratory Physiology Microbiology |
All other specialisms | YouTube vide0 by PHE
YouTube video by PHE |
|
| Gathering a patient history | Clinical Scientists across all specialisms | |||
| Triage | Physiological Sciences Specialisms | All other specialisms | ||
| Male and Female Catheterisation | Urodynamic Science | Gastrointestinal Physiology | ||
| Observations (BP, Temperature, Respiratory Rate, Pulse Oximetry) | Physiological Sciences | All other specialisms | Quick Look Procedure Resource for NON-CRITICAL CARE staff | |
| Moving and handling patients | Physiological Sciences | All other specialisms | e-Learning for health website: statutory and mandatory training | |
| Provide Point-of-care Testing | Life Science Specialisms Some Physiological Science Specialisms |
All other specialisms | Short introduction by a Biomedical Scientist | |
| Resuscitation |
Basic Life Support training | All Specialisms | ||
| Intermediate Life Support training | Cardiac Science | |||
| Advanced Life Support training | Cardiac Science | |||
| Airway Management |
Basic mask ventilation skills | Critical Care Science Cardiac Science Respiratory Physiology |
All other specialisms | |
| Advanced airway management skills | Respiratory Physiology | Cardiac Science | YouTube video | |
| Respiration | Blood gas sampling | Critical Care Science Cardiac Science Respiratory Physiology Life Sciences Clinical Engineering |
Other Physiological Science specialisms | Select ABG+analysis |
| Basic ventilator skill CPAP and NIV Oxygen therapy | Respiratory Physiology Critical Care Science Cardiac Science |
Clinical Engineering | Select Oxygen Therapy | |
| Respiratory Assessment | Respiratory Physiology Critical Care Science |
Cardiac Science | Select Respiratory Assessment | |
| Observations/MEWS | Respiratory Physiology Cardiac Science |
Other Physiological Science Specialisms | ||
| Circulation | Insertion of peripheral lines | Nuclear Medicine | Physiological Science Specialisms | |
| Cardiac Output Monitoring including data interpretation | Critical Care Science Cardiac Science |
Other Physiological Science Specialisms | Quick Look Procedure Resource for NON-CRITICAL CARE staff Safe Alarm Setting in Critical Care Areas | |
| Measuring Central Venous and Arterial Pressure | Critical Care Science Cardiac Science |
Other Physiological Science Specialisms | Select Arterial and CVP Monitoring: British Association of Critical Care Nurses
Quick Look Procedure Resource for NON-CRITICAL CARE staff Care of and sampling from an arterial line |
|
| Blood Pressure and Oxygen Saturation | Critical Care Science Cardiac Science |
Other Physiological Science Specialisms | Quick Look Procedure Resource for NON-CRITICAL CARE staff What to do if the SpO2 monitor alarms
Simple explanation of how to measure oxygen saturation: |
|
| Arrhythmia Management | Cardiac Science | |||
| Blood sampling | Phlebotomy | Life Sciences Nuclear medicine | Other Physiological Science Specialisms | |
| Store Biomedical Specimens and Samples | Life Sciences | All other specialisms | ||
| Prepare Samples and Documentation for Transport | Life Sciences | All other specialisms | ||
| Laboratory | Data Entry | All Specialisms | May need training on specific systems | |
| Cell Biology Techniques | Reproductive Science | |||
| Sample reception | All Life Science Specialisms | All other specialisms | ||
| Preparation of samples for analysis | Genomics Reproductive Science Clinical Biochemistry Microbiology |
All other Life Science Specialisms | ||
| Molecular techniques | Genomics Reproductive Science Clinical Biochemistry Microbiology |
Immunology | ||
| Reporting of tests | Genomics Biochemistry Microbiology |
All other Life Science Specialisms | ||
| Laboratory Quality assurance | Life Sciences Specialisms | |||
| Second check of drugs, documentation, ID | Medical Physics | Other Healthcare Science Specialisms | ||
| Sterile technique, microscopy, centrifuge | Reproductive science | All other Life Science Specialisms | ||
| Evaluating tests | Microbiology | All other Life Science Specialisms | ||
| Creating community testing pack kits | Microbiology | All other Life Science Specialisms | ||
| Preparing Culture Media and Solutions | Microbiology | All other Life Science Specialisms | ||
| Equipment | Provision of equipment | Clinical Engineering Medical Physics Critical Care Science |
Cardiac Science | |
| Management/testing | Clinical Engineering Critical Care Science |
Medical Physics including Radiation Safety Urodynamic Science Gastrointestinal Physiology Other Physiological Science Specialisms |
||
| Safe Handling of Liquid Nitrogen and other gases | Some Life Sciences including Reproductive Science Critical Care Science |
Respiratory Physiology |
||
| Cleaning and Disinfection of Medical Devices Testing, Maintenance and Breakdown | Decontamination Science Clinical Engineering Critical Care Science |
Clinical Pharmaceutical Science Cardiac Science |
||
| Inspection, Assembly, un-packaging of Medical Device | Decontamination Science Clinical Engineering |
Clinical Pharmaceutical Science Other Physiological Science specialisms |
||
| Management of Decontamination Equipment | Decontamination Science | Clinical Engineering Medical Physics |
||
| Technical Support for Computerised Medical Devices | Medical Physics Clinical Engineering |
Clinical Bioinformatics | ||
| Clinical Engineering Workshop Skills | Clinical Engineering Medical Physics |
|||
| Acceptance Testing of Medical Equipment | Clinical Engineering Medical Physics |
Other Physiological Science specialisms | ||
| Diagnosing and Rectifying Equipment Faults | Clinical Engineering Medical Physics Life Sciences |
|||
| Technical skills | ECG | Cardiac Science Critical Care Science |
Respiratory Physiology Vascular Science Urodynamic Science Gastrointestinal Physiology |
|
| Echocardiography: Screening | Cardiac Science | Critical Care Science Vascular Science |
||
| Echocardiography: Full Study | Cardiac Science | |||
| ICU Echo and Basic Lung Ultrasound | Cardiac Science | Vascular Science | Intensive Care Echo and Basic Lung Ultrasound (ICE-BLU) | |
| Magnetic Resonance Imaging | Medical Physics | |||
| Setting up a Cardiac Monitor and Cardiac Monitoring | Cardiac Science Critical Care Science |
Other Physiological Science Specialisms | Quick Look Procedure Resource for NON-CRITICAL CARE staff: What to do if the ECG monitor alarms | |
| Psychological care | Colleague support and debrief | Genomic Counsellors Audiological Science |
||
| Supporting Informed Consent | Reproductive Science Cardiac Science Gastrointestinal Physiology |
All other specialisms | ||
| Initial bereavement counselling | Genomic Counsellors | |||
| Support, breaking bad news, discussing and arranging tests, facilitating decision making. | Genomic Counsellors Reproductive Science Audiological Science |
All other specialisms | ||
| IT systems | Data analysis | Clinical Bioinformatics Medical Physics Applied Epidemiology |
All other specialisms | |
| Patient Pathway Management | Clinical Bioinformatics | All other specialisms | ||
| IT tasks | Medical Physics | All other specialisms | ||
| Risk management | Medical physics | All other specialisms | ||
| Data entry and record keeping | All Specialisms | |||
| Software/database design and development | Clinical Bioinformatics Medical Physics Applied Epidemiology |
|||
| Phyllogenics/sequence assembly | Clinical Bioinformatics | |||
| Statistics/implementing ISO standards to accept untested medical equipment, | Clinical Bioinformatics | Medical Physics Clinical Engineering Applied Epidemiology |
||
| Audit, research and development | All specialisms | |||
| Use of Information Communication Technology within the Clinical Environment | All Specialisms | |||
| Public Health Measures for COVID-19 | All Specialisms | London School of Hygiene and Tropical Medicine: coronavirus online short courses |
Appendix 3: Self-assessment competency reporting framework for laboratory staff
Below is an example self-assessment template that you could use to assess the competency of your staff in order to evaluate their suitability for redeployment.
Personal Details and Competency Information
| Your details | Answer | Comments |
|---|---|---|
| Name | ||
| Current role | ||
| Location | ||
| Registration number e.g. HCPC | ||
| Date of birth | ||
| Date last worked clinically | ||
| Date of last DBS check | ||
| Postcode of home address | ||
| Mobile number | ||
| Email address |
Please spend a few minutes reviewing the list to decide which of the crucial tasks you might be able to assist with:
- For any task you COULD manage, try to assess how much supervision you would need. Could you manage to do the skill or task without supervision, or would you need someone nearby to help if you struggled?
- There may be some tasks that would be a real struggle to start with but with some supervision and support you will be able to take on. For these tasks indicate “direct” supervision here.
| Skills you have | Competence in the following | Yes / No / with additional training | Supervision required: Direct (D) Indirect (I) None (N) |
|---|---|---|---|
| Health and safety | |||
| Personal Protective Equipment -Including Donning and Doffing -PP3 | |||
| Basic Infection Prevention Control | |||
| Laboratory Health and Safety | |||
| Sample reception | |||
| Unpacking High Risk Samples | |||
| Booking in Samples | |||
| Preparing Samples for Pre-analytical testing | |||
| Storing High Risk Samples | |||
| Setting up extraction of RNA/DNA | |||
| Equipment – Operation of Roche MagNA Pure 96 | |||
| Equipment – Maintenance of Roche MagNA Pure 96 | |||
| Equipment – Operation of Roche MagNA Pure Compact | |||
| Equipment – Maintenance of Roche MagNA Pure Compact | |||
| Routine Manual Plate – Extraction and Set Up | |||
| Setting up PCR | |||
| Routine Manual Plate – Extraction and Set Up ( as above ) |
|||
| Equipment – Operation of Roche LightCycler 480 |
|||
| Equipment – Maintenance of Roche LightCycler 480 |
|||
| Equipment – Operation of Roche PCR Setup (PSU) |
|||
| Equipment – Operation of Roche MagNA Pure 96 |
|||
| Equipment – Operation of Roche Primary Sample Handling (PSH) |
|||
| Equipment – Maintenance of Roche Primary Sample Handling (PSH) |
|||
| FLOW – Set Up |
|||
| Navigation of Aurora Software |
|||
| Flow Errors and Troubleshooting |
|||
| Compiling results | |||
| Routine Manual Plate – Analysis |
|||
| FLOW – 1 Analysis and Reporting |
|||
| FLOW- 2 Analysis and Reporting |
|||
| FLOW – 3 Analysis and Reporting |
|||
| Writing reports | |||
| Routine Manual Plate – Reporting |
|||
| FLOW – 1 Analysis and Reporting |
|||
| FLOW – 2 Analysis and Reporting |
|||
| FLOW – 3 Analysis and Reporting |
|||
| Reporting results | |||
| Routine Manual Plate – Reporting |
|||
| FLOW – 1 – Analysis and Reporting |
|||
| FLOW – 2 Analysis and Reporting |
|||
| FLOW – 3 Analysis and Reporting |
|||
Appendix 4: Self-assessment competency reporting framework for physiological sciences staff
Below is an example self-assessment template that you could use to assess the competency of your staff in order to assess their suitability for redeployment.
Personal Details and Competency Information
| Your details | Answer | Comments |
|---|---|---|
| Name | ||
| Current role | ||
| Location | ||
| Registration number e.g. HCPC, Voluntary registers | ||
| Date of birth | ||
| Date last worked clinically | ||
| Date of last DBS check | ||
| Postcode of home address | ||
| Mobile number | ||
| Email address |
Please spend a few minutes reviewing the list to decide which of the crucial tasks you might be able to assist with:
- For any task you COULD manage, try to assess how much supervision you would need. Could you manage to do the skill or task without supervision, or would you need someone nearby to help if you struggled?
- There may be some tasks that would be a real struggle to start with but with some supervision and support you will be able to take on. For these tasks indicate “direct” supervision here.
| Skills you have | Competence in the following | Yes / No / with additional training | Supervision required: Direct (D) Indirect (I) None (N) |
| Patient Care | PPE Donning & doffing | ||
| PPE Assess and teach donning and doffing | |||
| Washing & personal hygiene | |||
| Lifting and handling patients | |||
| IV drug administration training | |||
| National Early Warning Scoring | |||
| Resuscitation | Basic/ Intermediate Life Support training | ||
| Advanced Life Support training | |||
| Completing respect forms/DNAR | |||
| Airway Management | Basic mask ventilation skills | ||
| Advanced airway management skills | |||
| COVID-19 Intubation trained | |||
| Respiration | Ventilator management | ||
| Proning trained | |||
| Circulation | Insertion of peripheral lines | ||
| Insertion of central lines | |||
| Cardiac output monitoring interpretation | |||
| Arrhythmia management | |||
| Renal | Renal replacement therapy | ||
| Admission and Daily assessment
Technical skills |
Medical patients | ||
| ED Patients | |||
| Critical Care Patients | |||
| Ultrasound of chest | |||
| Echo – screening (FICE) | |||
| Echo full study | |||
| Central line insertion | |||
| Arterial line insertion | |||
| Tracheostomy – percutaneous | |||
| Tracheostomy – surgical | |||
| Blood gas sampling | |||
| Arterial line insertion | |||
| Easi-IO insertion | |||
| Psychological Care
|
Debriefing/TRiM training | ||
| Family interaction skills – support after breaking bad news | |||
| Prepare equipment according to instruction |
| Previously worked in | Yes/No | Comments |
|---|---|---|
| ICU | ||
| Anaesthetics | ||
| ED | ||
| Operating Theatres |
Appendix 5: Self-assessment competency reporting framework for physical sciences staff
Below is an example self-assessment template that you could use to assess the competency of your staff to assess their suitability for redeployment.
Personal details and competency information
| Your details | Answer | Comments |
|---|---|---|
| Name | ||
| Current role | ||
| Location | ||
| Registration number e.g. HCPC, IBMS | ||
| Date of birth | ||
| Date last worked clinically | ||
| Date of last DBS check | ||
| Postcode of home address | ||
| Mobile number | ||
| Email address |
Please spend a few minutes reviewing the list to decide which of the crucial tasks you might be able to assist with:
- For any task you COULD manage, try to assess how much supervision you would need. Could you manage to do the skill or task without supervision, or would you need someone nearby to help if you struggled?
- There may be some tasks that would be a real struggle to start with but with some supervision and support you will be able to take on. For these tasks indicate “direct” supervision here.
| Skills you have | Competence in the following | Yes / No / with additional training | Supervision required: Direct (D) Indirect (I) None (N) |
|---|---|---|---|
| Health and Safety | Use of Personal Protective Equipment | ||
| Basic Infection Prevention Control | |||
| Electrical safety | |||
| Oxygen safety Electronic Workshop Health and Safety |
|||
| Equipment decontamination | |||
| Engineering | Gas and air management | ||
| Pressure Systems, Pumps & Compressors | |||
| PCB diagnostics | |||
| Biomedical equipment |
Equipment acceptance | ||
| Commissioning and functional testing | |||
| Preparing equipment for use | |||
| Software configuration | |||
| Calibration and functional checks | |||
| Preventative and scheduled maintenance | |||
| Fault finding and Repair | |||
| Electrical safety testing | |||
| Training |
Production of training materials | ||
| Training delivery | |||
| Quality systems |
Working under formal quality systems | ||
| Support tasks |
Helpdesk | ||
| Stores and equipment management | |||
| Project management |
| Previously worked in | Comments | Yes/No |
|---|---|---|
| ICU or high intensity care areas | ||
| General ward environment | ||
| Electronic equipment repair facilities | ||
| Medical equipment manufacturer / service supplier |
Appendix 6: Bedside clinical experienced workers
Basic requirements for bedside support workers include an understanding of healthcare and a commitment to work in healthcare environment, compassion/kindness, personal resilience, willingness to learn.
Any HCS with patient facing experience can be upskilled to support the bedside team, e.g. Audiological Science, Cardiac Science, Respiratory Physiology, Neurophysiology, Reproductive Sciences, Nuclear Medicine
Examples of potential Bedside Support Workers from the HCS workforce include:
- Healthcare Science Assistant: Level 2
- Healthcare Science Assistant: Level 3
- Healthcare Science Associate Level 4
- Healthcare Science Practitioner Level 6
- Healthcare Science Research Staff
- Healthcare Science Scientist Training Programme Trainees
- Healthcare Science Practitioner Trainees
Appendix 7: Opportunities to deploy healthcare science staff
Some Healthcare Science specialisms have seen a large reduction in their workload. This appendix includes ideas for re-deployment of staff, for example in Audiological Science, to support staff during the COVID-19 outbreak and could help employers consider redeployment of their HCS staff. Some additional high level tasks for example project management, would be ideal for experienced healthcare scientists.
- Assist pathology with analysis of COVID-19 test results
- Calibration and repair of respiratory equipment including oxygen cylinders
- Calibration and repair of renal equipment
- Assistance with ward-staff in obtaining samples to test for COVID-19
- Dispensing in pharmacy where staff shortages are present
- Cleaning and distribution of PPE to medical staff
- De-sanitising and cleaning of medical areas exposed to COVID-19
- Distribution of supplies of equipment needed to treat COVID-19 patients
- Triaging of incoming patients into the hospital based upon severity of symptoms based upon any available clinical guidelines with support from triage nurse.
- Support to 111 staff to help telephone triage suspected cases
- Family liaison role contact via phone between patient and families, including basic bereavement counselling and signposting for support
- Stock ordering and monitoring within the new hospital
- Documenting of in-patient notes off-site – may be a useful timesaving mechanism to avoid doctors / nurses writing down information in the ward, information could be relayed via phone from medical staff to HCS and stored electronically.
- Statistics reporting of capacity / demand in hospital, number of cases etc.
- Assisting clinicians with respiratory function tests and renal function tests.
- Provision of oxygen, fluids and food to non-ICU COVID-19 patients
- Staff-wellbeing phone line – providing advice and signposting
- Discharge nurse role – to ensure treated patients return to community safely
