Primary care

GPs have one of the highest public satisfaction ratings of any public service, at over 85%, (25) but we know improving access to primary care services is a top priority for patients (26). General practice is undeniably the bedrock of NHS care and we have more GPs per head than Germany (27). General practice provides over 300 million patient consultations each year, compared to 23 million A&E visits. So if general practice fails, the NHS fails. Yet a year’s worth of GP care per patient costs less than two A&E visits, and we spend less on general practice than on hospital outpatients. For the past decade funding for hospitals has been growing around twice as fast as for family doctor services.
That’s why the General Practice Forward View set out a detailed, costed package of investment and reform for primary care now through to 2020. It will mean more convenient access to care, a stronger focus on population health and prevention, more GPs and a wider range of practice staff, operating in more modern buildings, and better integrated with community and preventive services, hospital specialists and mental health care. In doing so we are working with the Royal College of GPs, the General Practitioners Committee, the National Association of Primary Care, and others. See the General Practice Forward View (28).
What’s been achieved in England over the past three years?
- More convenient access to primary care services, with 17 million people now able to access GP appointments at evenings and weekends.
- First steps to expand the primary care workforce, including an additional 300 GP trainees, and 491 clinical pharmacists. New national mental health service for GPs launched.
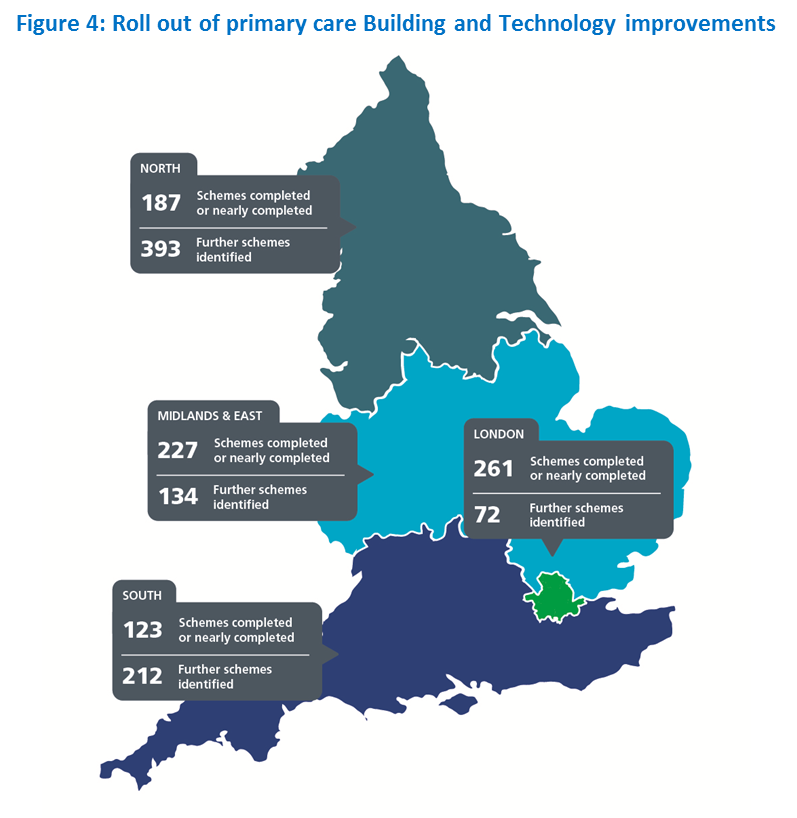
- 560 new schemes completed and over 200 in progress to modernise GP surgery buildings, IT and equipment.
- New ‘vanguard’ models of scaled primary care across 23 areas, covering nearly 10% of the population, which have seen lower growth in emergency hospital admissions than the rest of England.
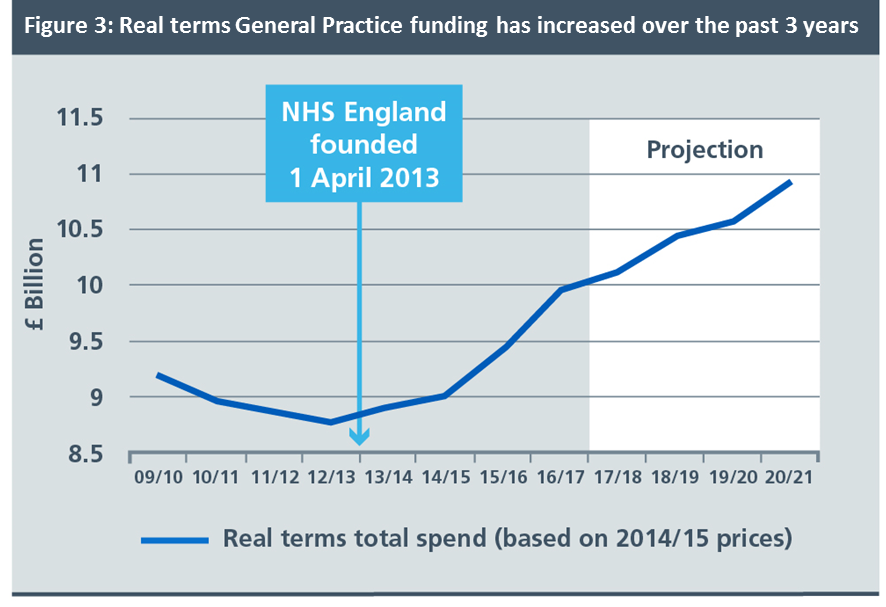
- In the years prior to the creation of NHS England, investment in general practice was falling in real terms. Each year since the establishment of NHS England we have made sure it has gone up, with real terms funding increasing by 8% over the past 3 years.
Key improvements for 2017/18 and 2018/19
- Boost GP numbers. The Government has set an objective of an extra 5000 doctors working in general practice by 2020. Numbers entering GP training are up by 10% since 2015 and HEE will fill a further 230 places in 2017/18 to ensure they reach 3250 trainees per year. Initial applications for GP training in 2017 are up by 5% on the same time last year. Practical action to boost GP retention, as set out in the GP Forward View, will include:
- The GP Career Plus scheme in 10 sites across the country, supporting retention of experienced doctors by allowing them to continue working without the responsibilities of a partnership.
- The Time to Care programme, investing £30 million to help practices reduce their workload and free up GP time.
- The new NHS GP Health Service, to support doctors suffering from mental ill-health and addiction.
- For many people with jobs, particularly self-employed and hourly paid workers, tackling inequalities in access will mean making available bookable evening and weekend appointments. By March 2018, the Mandate requires that 40% of the country will benefit from extended access to GP appointments at evenings and weekends, but we are aiming for 50%. By March 2019 this will extend to 100% of the country. This does not require every practice itself to be open each evenings or weekend, but it does mean that patients anywhere will be able to book appointments when they need them. To provide these additional services, general practices will increasingly cooperate with other practices in formal or informal networks.
- More convenient patient access to GP services. As additional GPs, therapists, pharmacists and nurses come on stream we want to improve access to convenient and needed practice appointments. During daytime surgery hours, practices are increasingly ‘streaming’ patients so as to offer convenient same day urgent appointments, while preserving continuity of care for patients with more complex long term conditions. During 2017/18 practice profiles will be published including patient survey results and ease of making an appointment. From October 2017 the new agreed GP contract means that practices who shut for half days each week will not be eligible for a share of the £88 million extended access scheme.
- Expand multidisciplinary primary care. We will:
- increase the number of clinical pharmacists working in GP surgeries from the 491 we are co-funding today to over 900 by March 2018 and over 1300 by March 2019. Not only will patients benefit from pharmacy services, but the introduction of clinical pharmacists will also help free up GP time to focus on those patients who need it most, for example, by supporting patients to manage high risk conditions such as high blood pressure earlier and more effectively, preventing cardiovascular disease. Clinical pharmacists and will also help to ensure efficient use of medicines.
- 800 mental health therapists will be placed in primary care by March 2017 rising to over 1500 by March 2018. These therapists will lead the way in how we integrate physical and mental healthcare outside of hospital.
- HEE is supporting universities to train 3000 physician associates by 2020. HEE will work with NHS England to incentivise up to 1000 of these staff to work in General Practice.
- HEE has also published findings on how to improve the future of general practice nursing. NHS England and HEE will work with partners on this, backed by £15m as promised in the GP Forward View.
- Modernise primary care premises. We have been investing steadily in upgrading primary care facilities, benefiting both patients and staff. Over 800 further infrastructure projects are identified for investment by 2019.
How changes will be implemented
- Continue to increase investment in GP services, so that by 2020/21, funding will rise by £2.4 billion, a 14% real terms increase. Targeted national investment in a growing number of clinical pharmacists and mental health therapists embedded in primary care.
- Encourage practices to work together in ‘hubs’ or networks. Most GP surgeries will increasingly work together in primary care networks or hubs. This is because a combined patient population of at least 30,000-50,000 allows practices to share community nursing, mental health, and clinical pharmacy teams, expand diagnostic facilities, and pool responsibility for urgent care and extended access. They also involve working more closely with community pharmacists, to make fuller use of the contribution they make. This can be as relevant for practices in rural areas as in towns or cities, since the model does not require practice mergers or closures and does not necessarily depend on physical co-location of services. There are various routes to achieving this that are now in hand covering a majority of practices across England, including federations, ‘super-surgeries’, primary care homes, and ‘multispecialty community providers’. Most local Sustainability and Transformation Plans are intending to accelerate this move, so as to enable more proactive or ‘extensivist’ primary care. Nationally we will also use funding incentives – including for extra staff and premises investments – to support this process.
- Contract reform. The 2004 GP contract linked a proportion of practice income to performance against detailed indicators – the Quality and Outcomes Framework (QOF). There is now wide agreement that this particular approach has run its course, and is now partly a tick-box exercise (29). We will seek to develop and agree with relevant stakeholders a successor to QOF, which would allow the reinvestment of £700 million a year into improved patient access, professionally-led quality improvement, greater population health management, and patients’ supported self-management, to reduce avoidable demand in secondary care.
Find out more
See more information by visiting our GP and primary care commissioning pages.
References
25. https://www.england.nhs.uk/statistics/2016/07/07/gp-patient-survey-2015-16/
26. As shown by Healthwatch’s annual survey, the 2016 British Social Attitudes Survey, and the annual NHS GP patient survey.
27. https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-016-0458-3
28. https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
29. See for example: The Lancet (17 May 2016) Volume 388, Issue 10041, 268 – 274. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. Ryan, Andrew M et al.