Introducing the Universal Care Plan to the Islington Memory Service
Authors
Helen Souris
Senior Clinical Project Manager, London Dementia Clinical Network, NHS England
Co- authors
Laura Cook
Clinical Programme Lead – Ageing Well, London Clinical Network, NHS England
Nerida Burnie
GP and Primary Care Lead, London Dementia Clinical Network, NHS England
Acknowledgements
The Dementia Clinical Network NHS England London region would like to thank the clinicians from the Islington Memory Service who participated in this pilot and the SWL Universal Care Plan Programme team for their support with this project.
Background
The Universal Care Plan (UCP) is a dynamic, integrated digital care plan that is accessible to all health and care professionals across London. In its previous form, the UCP was used as a shareable Advance Care Plan (ACP), with a focus on supporting people in their last year of life. At the time, there was no shareable personalised care and support plan. Any care plans were either paper based and soon out of date or only visible to the organisation that recorded them. Patients were required to tell their story multiple times and clinicians were often expected to make important decisions about a person’s care with limited information.
In 2022 Clinical areas were invited to submit projects in which the UCP could be expanded and personalised for specific clinical areas. Dementia, Frailty and Learning Disabilities(LD), were the first clinical areas to go forward with the prototype for the new expanded UCP. The Dementia, Frailty and LD Clinical Networks worked alongside the Palliative End of Life Care (PEoLC) and Personalised Care Clinical Networks and the South West London UCP Programme team to develop the expanded template that has since been embedded into the UCP. There was extensive engagement with stakeholders and the template was co-produced with dementia and frailty clinicians in acute and community settings, social care as well as with people with lived experience and their carers. The UCP with the new expanded template was launched in January 2025.
Across London, most people with dementia are diagnosed in memory assessment services within Mental Health Trusts. Most memory services discharge people with dementia back to primary care after the initial post-diagnostic period (around 3-6 months). Memory services typically complete a dementia care plan and although a copy is shared with primary care, they cannot edit or update the plan. Primary care will then start their own dementia care plan using EMIS/SystmOne. This care plan is reviewed annually, which is a QOF requirement (everyone with dementia to have an annual review and care plan).
As writing care plans in this way has always been the practice within memory services, it seemed appropriate to pilot the UCP in a memory service that was not using the UCP. The Islington Memory Service was identified as a memory service which was not familiar with the UCP and had not used it in any capacity, that is, the UCP had not been accessed by the service for viewing, editing or creating. The UCP dashboard also indicated that no UCPs had been created by the team. This service was approached and were willing to engage in the pilot.
Aims and Objectives
- To identify a memory service that was not familiar with/not using the UCP to act as a pilot site
- To onboard and train clinicians to use the UCP
- To identify barriers and challenges to using the UCP as a care plan
- To support implementation of the UCP within that memory service
- To get a clear understanding of the value and benefit of the UCP for clinicians and patients within memory services
Methodology
The project was led by the Ageing Well collaboration Group which included the project leads from the Dementia, Frailty and Palliative End of Life Care Clinical Networks teams and the dementia primary care lead. A representative from the SWL UCP team was invited to attend the meetings to address any technical queries raised by the group. The participants in the pilot came from a variety of clinical professional backgrounds and bands. This included a Team Manager, Clinical Nurse lead, a Specialist Memory Nurse, Assistant Practitioner and a Dementia Navigator. The Banding ranged from Band 4 to Band 7.
An initial onboarding/introductory session was held with the team outlining the objectives of the pilot. This included a description of what the UCP was, how to access it, the benefits of the UCP to the patient and the clinicians and the timeline of the pilot project. An agreement was made regarding the frequency of meetings, but they were also offered support in between meetings, if needed.
The team were introduced to the UCP website and shown how to access the UCP Training modules. The training is delivered online in 3 different forms and can be accessed by the clinician dependent on the time that they have available, that is, in bitesize ‘Got 5 minutes?’, one hour ‘Time for lunch’ or 2-3 hours, ‘Protected learning’. In order to get an indication of how much training, clinicians may need to be able to create, edit and view a UCP, the Clinical Network signposted the clinicians to the existing learning modules but did not deliver the training.
Touchpoint meetings were held on a fortnightly basis for 30 minutes. There were standing items but the meeting agenda was generally flexible, allowing sufficient time for the clinicians to bring any issues to these meetings. Initial meetings focused on accessing the UCP and their initial experience of using it. The discussions raised over the course of the sessions included the NHS App, Proxy and Voluntary sector access, data sharing, and recording of the DNACPR. The UCP dashboard was demonstrated and the group were informed of the data collection by the UCP team representative.
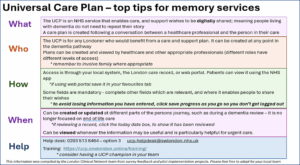
A delay in the launch of the UCP expanded template, meant there was time to prepare new resources. A UCP ‘Top tips guide’ was developed (Appendix 2). This arose following a survey that had been created within the Ageing Well collaboration group, to gauge the thoughts of the PEoLC clinicians on their tips for completing UCPs. This was presented to the group in draft form and updated by the team over the duration of the pilot. Although this version was created for a memory service, it can be adapted for use across all clinical areas.
Outcomes – learning from the pilot
The pilot took place between January to April 2025. Fortnightly meetings were held in this time period with a final meeting taking place 6 weeks later in mid-May; this meeting gave the team an opportunity to share any further experiences of using the UCP and to evaluate the learning. This was done using a Microsoft survey (Appendix 1). All seven participants of the pilot completed the survey.
At the start of the pilot, the clinicians stated having no prior knowledge of the UCP. Following the pilot, the clinicians reported having had limited time and capacity to complete all the training modules on the website. Despite this, they all felt that they were able to confidently view and edit a UCP and only one participant did not feel confident creating a new one. All participants reported that they found the experience of editing or completing a UCP easy and intuitive and felt that the UCP would benefit their patients.
The participants saw value in using the UCP, however, two did not feel that the current version of the UCP included enough information to replace the teams’ existing review templates, and five were not sure that it could. The reasons they gave related to the level of detail of the reviews, particularly in patients needing antipsychotic reviews which tend to be more frequent and may result in medication changes.
Of the seven clinicians that participated in the pilot, six felt that the UCP could be used as the shareable care plan for London and one was unsure.
Some of the benefits cited in the survey included:
“Beneficial holistic patient care online tool, allowing stronger connectivity between healthcare services in primary, secondary & social care”
“It is easily accessible. It will enable colleagues to access important information about what matters to the patient, their likes, dislikes & preferences”
“It includes a lot of useful medical information as a lot of our patients have comorbidities & will have been seen by several services. We can add to make more personal”
“It will serve to prevent unnecessary delays to care with its aim for providing the right care at the right time”
Their ‘Top tips’ included the following:
- Do the online training
- Familiarise yourself with the UCP template prior to attempting one
- Start with a patient who already has a UCP
- Only complete the sections that are relevant to your team or known to you at the time of your contact with the patient
- Raise the UCP as part of the multidisciplinary discussions to raise awareness of the UCP with all members of the team
- Keep practicing!
Summary and Next Steps
The London Ageing Well collaboration team within the London clinical networks engaged with the Islington Memory Service and conducted a pilot introducing the UCP to the team. This memory service was chosen as they had no prior knowledge or experience of the UCP and the Clinical Networks needed an indication of the level of input and support required to implement the UCP. The intention is, that learning gleaned from the pilot will shape the implementation of the UCP across all London memory services
The pilot was conducted between January to April 2025 with a final evaluation meeting held in May.
Seven participants of varying bands participated in the pilot. The training was online, provided by the UCP website. Clinicians only had capacity to access the short training modules however, they felt that this was sufficient as they described the UCP as being intuitive and easy to complete. By the end of the pilot, participants felt they had the skills to access, edit and create a UCP. They felt it was of benefit to the patient as it was a holistic tool that was easily accessible, personalised, informative and could potentially avoid delays by providing the ‘right care at the right time’.
Following the analysis of the surveys, the pilot was presented at the London Memory Service Network meeting to raise awareness and to encourage services to start making use of the UCP. Next steps include supporting the implementation of the UCP in all London memory services and acute hospital settings.
Appendix 1
Microsoft survey outcomes
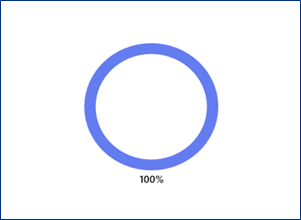
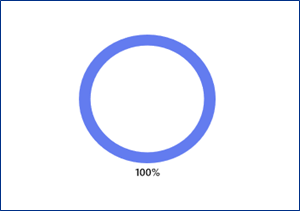
Since contributing to the pilot, are you able to view a UCP?
No Not sure
|
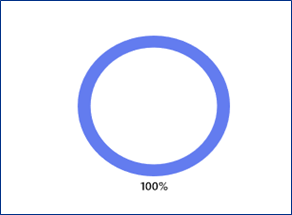
Complete/edit a UCP?
No Not sure
|
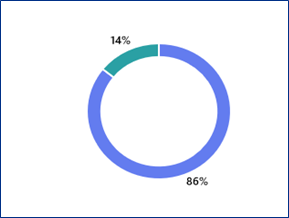
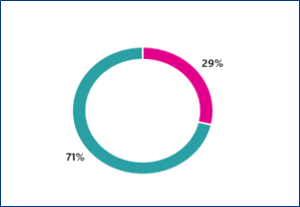
Create a UCP?
No Not sure
|
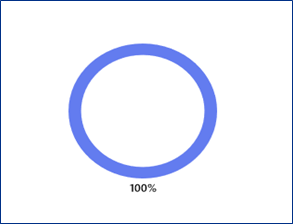
What was your experience of editing or completing the UCP?
Easy/Intuitive Difficult Not sure N/A, not completed any
|
Do you think the UCP will benefit your patients?
Yes No Somewhat Not sure
|
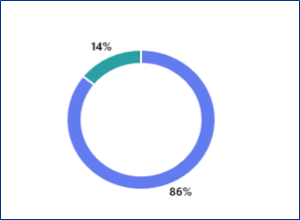
Does the UCP include enough information to replace the existing review template?
No Not sure
|
Could it be used as the shareable dementia care plan for London?
No Maybe |