Analogue to digital
The NHS is becoming more digitally accessible, with technology at the heart of how we deliver faster, more efficient and more personalised care.
Services across the capital are leading the way in delivering the Government’s shift from analogue to digital healthcare, using technology to maximise clinical efficiency and provide better, more more personalised care for patients.
The NHS in London is already making strides to deliver the 10 Year Health Plan, to strengthen the health of the NHS for generations to come. Across London’s community and hospital settings, organisations are using innovative technology to free up staff time and improve patient care.
Dame Caroline Clarke, Regional Director of the NHS in London, said: “We have a clear ambition in London to use digital technology to transform the way we deliver care, so it is encouraging to see so many of London’s NHS services already making significant progress in delivering the 10 Year Plan’s vision.
“As we shift our focus from analogue to digital, I’m proud that London is home to some of the most innovative services, pioneering new ways of using technology to deliver high quality and accessible care for everyone.”
Explore how services across London are evolving to improve outcomes, enhance access and strengthen care in the places people live.
Overview
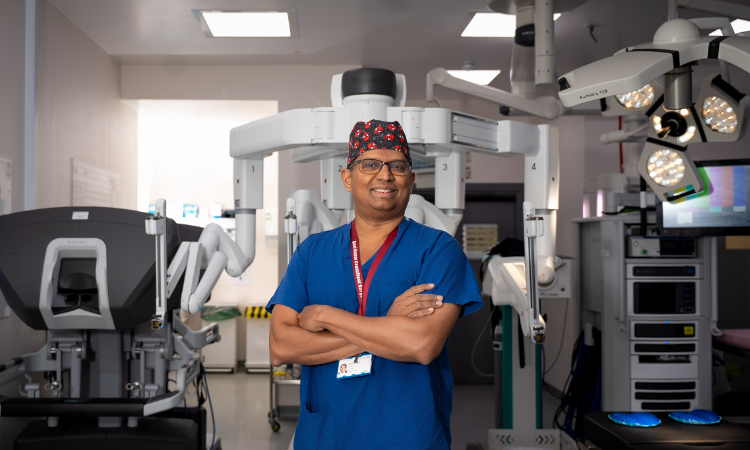
King’s College Hospital NHS Foundation Trust has reached a significant milestone, completing 1,000 robotic-assisted surgeries in just over two years. This achievement demonstrates how advanced surgical technology can help reduce waiting times and improve patient outcomes.
The challenge
Like many NHS hospitals, King’s faced pressure to treat patients quickly while maintaining high standards of care. Traditional open and laparoscopic (keyhole) surgery, while effective, can limit the number of procedures surgeons can perform in a day. Some patients, particularly those with obesity, also face additional challenges with conventional surgical approaches.
The solution
King’s College Hospital introduced a surgical robot, funded by King’s College Hospital Charity. The robot works alongside surgeons rather than replacing them. Surgeons sit at a special console and control robotic instruments that precisely replicate their hand movements.
The technology offers several advantages over traditional methods:
- A 3D immersive view with nine times the magnification of laparoscopic surgery
- Real-time guidance showing the location of tiny nerves and blood vessels
- More precise instrument control, particularly beneficial for patients with obesity
- Greater accuracy when suturing after procedures
The results
The introduction of robotic surgery has delivered measurable improvements for both patients and the hospital.
For patients:
- Reduced post-operative pain
- Faster recovery times
- Shorter hospital stays, with many patients going home within 24 hours
- Fewer complications, including less risk of post-operative bleeding
- Access to surgery for some patients whose health conditions previously made operations difficult
For the hospital:
- Increased surgical capacity, with some surgeons now completing four or five cases per list compared to two previously
- Shorter waiting times for patients awaiting procedures
Procedures performed
The robot is currently used for a range of operations including bariatric (weight loss) surgery, hernia repairs and gall bladder removals.
Looking ahead
Following this success, King’s hopes to extend access to robotic-assisted surgery to more surgical teams, allowing even more patients to benefit from the technology.
Find out more on the King’s College Hospital NHS Foundation trust website.
Overview
Barking, Havering and Redbridge University Hospitals NHS Trust has embarked on a major digital transformation to improve patient safety and enhance the quality of care. By introducing an Electronic Patient Record (EPR) system, the Trust is reducing reliance on paper forms and ensuring that all essential patient information—such as medications, test results, and allergies—is stored securely in one digital record. This initiative is designed to cut down errors, free up clinician time, and allow staff to focus more on patients.
Challenge
Transitioning from paper-based systems to digital records is a significant change. The Trust acknowledges that the move may be “bumpy” at first, with some patients experiencing delays during the initial rollout. However, the long-term benefits of streamlined processes and improved safety are expected to outweigh these short-term challenges.
Impact
- More time with patients: Clinicians spend less time on paperwork and more time delivering care.
- Streamlined workflows: Digital forms and automated data entry simplify processes across departments.
- Faster access to information: Test results, imaging, and patient notes can be retrieved quickly and securely.
- Improved safety: Clinicians have a complete view of patient records, reducing duplication and errors.
Matthew Trainer, Chief Executive of the Trust, explained:
“Rolling out electronic patient records at our trust will improve safety and patient experience. Our clinicians will be able to see a patient’s notes, scan, and test results in one place, including when they have been seen in different hospitals in north east London. This will reduce errors and should mean patients don’t have to repeat themselves as often.”
Read the full story on the Barking and Dagenham Post or visit the BHRUHT website.
Overview
South West London Integrated Care Board has digitally revolutionised its high-cost drugs platform to systematically collect real-world patient outcome data. By automating data processes and enabling outcome-based digital audits, the pioneering work allows SWL to standardise prescribing practices, reduce variation, optimise medicines value and improve patient care across multiple specialties.
Challenge
High-cost drugs are expensive and patient responses vary. Existing systems lacked timely, system-wide evidence on which patients benefit most, making it difficult to target treatments and inform commissioning decisions.
Solution
- Digital transformation of HCD data platform and real-world data generation: shifted from prior approval to a live digital clinical audit tool supporting system-wide medicines optimisation, enabling outcome-based audits which support evidence-informed commissioning decisions.
- Automation: automated data validation and auto-approval of forms reduce manual checks and errors, enabling faster patient access to treatment.
- Data quality: validated disease scores and calculated fields improve data accuracy and reduce duplication in form filling.
- Multi-trust MDT model: facilitates peer review for complex cases, reducing variation and improving clinical equity.
- Cost savings and ROI: delivers savings, return on investment, and reduces staffing needs.
- Improved governance and benchmarking: supports consistent pathway implementation and identifies practice variation.
Impact
- Better clinical decisions – system-wide real-world outcome audits guide optimal treatment choices, improve equity, reduce variation, and support evidence-based prescribing in line with NICE guidance.
- Smarter use of resources – repurposing the data platform as a live audit tool maximises existing infrastructure for system-wide optimisation. Commissioners use real outcomes to focus funding and allowing a move towards value-based contracts.
- Efficiency and oversight: automation reduces duplication and manual tasks, speeds up pharmacist screening, and enables easier digital audits—strengthening oversight, governance, and patient safety.
- Cost avoidance: data-driven HCD treatment choices ensure use of the most clinically appropriate options.
Patient and clinician benefits
- Patients: consistent access to the most clinically appropriate and cost-effective high-cost drugs through real-world data tracking and reduced treatment variation.
- Clinicians: benefit from automated data validation, reduced manual entries, and enhanced decision-making via system-wide audits and multi-Trust MDTs, supporting evidence-informed care.
Next steps
Explore wider NHS adoption and link high-cost drugs clinical data with hospital and primary care activity data. This will help assess the impact of high-cost drugs use on e.g. hospital attendances and identify potential health inequalities.
Overview
Moorfields Eye Hospital took part in a world-first trial of the PRIMA electronic retinal implant, which helped people with geographic atrophy (advanced dry age-related macular degeneration) regain the ability to read letters, numbers and words.
Challenge
Geographic atrophy destroys central vision, leaving only peripheral sight and making everyday tasks such as reading prescriptions, recognising labels and doing crosswords impossible. Patients lose independence and struggle with daily living.
Solution
The PRIMA system uses a tiny 2 mm by 2 mm implant placed under the central retina, paired with augmented-reality glasses that contain a camera. A small processor converts camera images into infrared signals that stimulate the implant. Around a month after surgery clinicians activate the device and provide intensive rehabilitation to help patients interpret the new visual signals.
Impact
In the multi‑site trial of 38 patients, 84% were able to read letters, numbers and words while using PRIMA, with many reading multiple lines on a vision chart when previously they could not see the chart at all. Patients regained everyday abilities such as reading prescriptions, doing crosswords and reading product labels, improving independence and quality of life.
Patient experience
Participants described the results as ‘life-changing’. Simple tasks that were once impossible became possible again with practice and rehabilitation. Patients reported excitement when the device was first switched on and steady improvement over time as they learned to interpret the device’s signals.
Clinical perspective and next steps
Surgeons at Moorfields see this as a paradigm shift in artificial vision. Developers are pursuing regulatory approval. If approved, the technology will be considered for wider availability on the NHS by NICE.
The tiny 2mm by 2mm chip which was implanted into the eyes of patients on the trial (Science Corporation/PA)
Read more on the Moorfields Eye Hospital NHS Foundation Trust website.
Media coverage: Sky News, BBC, The Telegraph, The Guardian, The Standard.
 Overview
Overview
Lewisham and Greenwich NHS Trust (LGT) is piloting the use of artificial intelligence to support pharmacy teams at Queen Elizabeth Hospital, with the aim of improving efficiency and patient safety. This early-stage initiative is designed to test how AI can augment staff by analysing dispensing and usage data to spot patterns, optimise stock placement, and reduce routine manual work.
Challenge
Pharmacy workflows involve complex decisions about what medicines are needed, where they should be stored, and when stock must be replenished. Seasonal surges and ward-specific demands make it hard for staff to predict needs, increasing the risk of delays, stock shortages, or unnecessary handling.
Solution
- Automation and data analysis: Medication is dispensed by a robot and administered by clinicians while AI analyses usage data to highlight trends and risks.
- Targeted stock placement: The system identifies where supplies should be located, for example, ensuring nebulisers are available on the respiratory ward during winter flu season.
- Staff-centred design: The AI supports pharmacists and technicians rather than replacing them, taking on repetitive tasks so staff can focus on clinical decision-making and patient care.
Impact
- Greater efficiency: Workflows are streamlined as AI recommends optimal storage and replenishment, cutting time spent on manual checking and transport.
- Improved safety: Early detection of usage patterns reduces the risk of stockouts and helps ensure the right medicines are available where and when they are needed.
- Workforce development: Staff are being trained in AI use and upskilled to take on higher-value roles that focus on clinical support, education, and patient-facing tasks
Rachel Knight, Chief Pharmacist at the Trust, said: “Understanding the intricate detail of what we’re dispensing, to who and where it needs to be, is really challenging,” she explained. AI can identify patterns that pharmacists could not manually detect, showing where medicines should be stored so they are ready for use. It makes our whole workflow more efficient and it also makes it a lot safer for the patients.”
“I knew that it was going to be really pivotal over the next 5, 10, 15 years and I didn’t feel that in my role as a leader, I was able to lead my team effectively through that.”
Zeinab Hussain, the Trust’s Digital Health Leader, emphasised that AI is not there to take jobs. “It can take over some of those mundane repetitive tasks,” she said. “If it can help us to detect risks sooner, then really that’s just going to help us with better outcomes in the long term. There’s plenty of work to do in the NHS, so there’s absolutely no concern around us losing staff, but actually it’s about upskilling them to do different roles within the organisation.”
Next steps
The Trust will continue training teams, monitor outcomes as AI-driven recommendations are adopted, and scale learnings across services where data-driven stock management and automation can improve care and safety.
Read more on the Lewisham and Greenwich NHS Trust website
See BBC coverage here
Overview
Lewisham and Greenwich NHS Trust became the first NHS trust to make pre-operative assessment forms available through the NHS App, streamlining the patient pathway and enabling remote clinical review. The trust has used the Document and Questionnaire Management (DQM) tool from DrDoctor since January 2025 and launched NHS App access to those forms on 15 September 2025.
Challenge
Pre-operative assessments traditionally relied on in-clinic or telephone collection of patient information, creating delays, administrative burden, and fragmented records. Clinicians needed a single, reliable place to view pre-op details while patients wanted a simpler, more convenient way to complete required forms.
Solution
- Technology: DQM tool from DrDoctor integrated into the NHS App.
- Deployment: Forms available to patients via NHS App.
- Functionality: Patients complete pre-operative assessments at home; staff review responses remotely and store results within the digital patient record.
Implementation and partnerships
The DQM tool was developed collaboratively by Moorfields Eye Hospital NHS Foundation Trust, DrDoctor, and NHS England and launched in April 2025.
Lewisham and Greenwich NHS Trust adopted DQM in January 2025 and extended functionality into the NHS App in September 2025. Clinical leadership at Lewisham and Greenwich and Moorfields, plus DrDoctor and national bodies, coordinated pilots, workflows, and user experience design.
Impact
- Patient convenience: Patients can complete assessments at home through the NHS App, reducing travel and time spent in hospital settings.
- Clinical efficiency: Staff can review assessments remotely, saving administrative time and enabling faster decision making.
- Data consolidation: Pre-operative details are gathered into a single digital location, reducing duplication and improving information quality.
- System readiness: The rollout supports national plans to expand DQM, symptom trackers, and patient involvement tools across the NHS App, positioning trusts to use the app as a consistent digital front door to care.
Dr Mehool Patel, chief medical officer at Lewisham and Greenwich NHS Trust, said: “We are delighted to be the first NHS trust to roll out these features after the successful pilot at Moorfields. We’re at a turning point for the NHS, where we can either integrate digital tools to streamline operations and ultimately improve patient care, or otherwise fall behind. Partnering with DrDoctor, we’re able to see a future where full integration with the NHS App is possible, and we can provide our patients with the best and smoothest experience.”
Dilani Siriwardena, deputy medical director and NHS London clinical director for ophthalmology at Moorfields Eye Hospital NHS FT, added: “We’re extremely proud to have launched an industry-first with DrDoctor and NHSE, bringing pre-op assessment digital forms to the forefront of NHS innovation. The time saved for clinicians and patients alike, as well as having a patient’s preoperative details in one digital home, is invaluable.”
Tom Whicher, chief executive and co-founder of DrDoctor, said: “It’s a lot to ask of dedicated NHS teams to implement big changes while continuing to prioritise patient care day in and day out. We’re lucky to be working with brave trusts like LGT and Moorfields who are ready to innovate and embrace a new type of NHS. These partnerships give me confidence that we’ll see a stronger healthcare system in the future through the use of tools that reduce resource waste and help integration across services.”
Next steps
Trusts across the country are expected to adopt wider DQM use within the NHS App, including symptom trackers and patient involvement tools. Lewisham and Greenwich NHS Trust’s early adoption provides a practical template for scaling pre-operative digital workflows nationally.
Media coverage: Find out more on the Digital Health website.
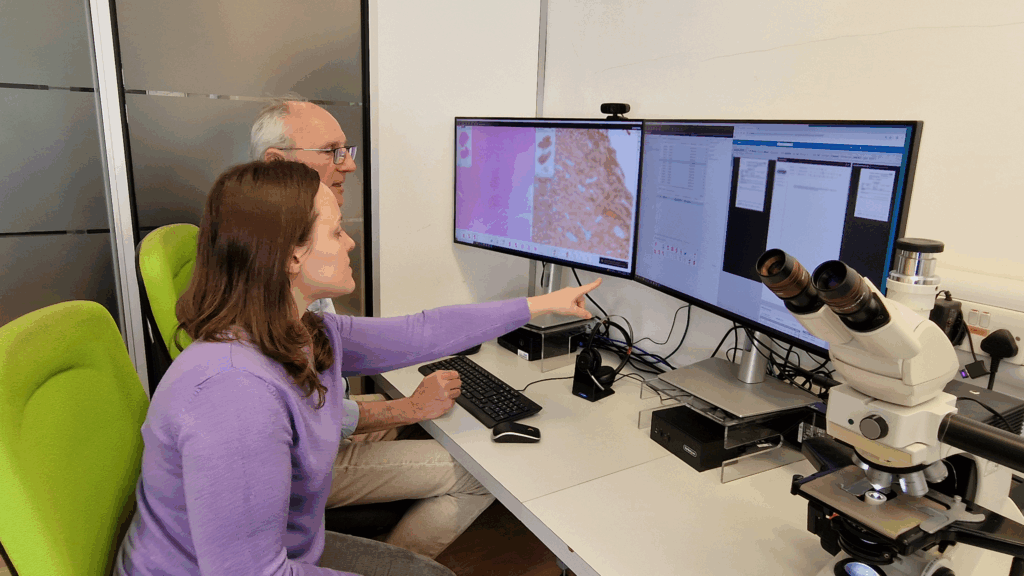
Overview
University College London Hospitals NHS Foundation Trust (UCLH) has gone live with digital pathology as part of a coordinated North Central London programme alongside Royal Free London and Whittington Health. The move replaces traditional glass-slide workflows with high-resolution digital images, supporting the NHS ambition to shift “from analogue to digital” and modernise diagnostic services.
Challenge
Traditional glass-slide workflows required physical transport, manual handling, and local review, creating delays for specialist opinions and risks of slide damage or loss. These constraints limited flexibility for pathologists, slowed turnaround times, and constrained opportunities for cross-site collaboration, training, and research.
Solution and implementation
- Technology adopted: Slide scanning devices capture high-resolution digital images for review on medical-grade screens. Integration with Epic ensures continuity in reporting while access to national networks like NPIC enables collaboration with subspecialty experts and supports training across trusts.
- Deployment approach: A coordinated, multi-trust rollout across NCL enabled shared expertise and aligned workflows. The collaboration involves UCLH and Royal Free London (both part of the joint venture partnership with The Doctors Laboratory which forms Health Services Laboratories), Whittington Health, and the National Pathology Imaging Cooperative (NPIC) based at Leeds Teaching Hospitals NHS Trust.
- Early uptake: Within weeks of go-live, digital images supported diagnosis and reporting in nearly 70% of histopathology cases at UCLH, demonstrating rapid clinician adoption.
Impact
- Faster specialist review: Instant image sharing enables quicker second opinions and specialist input, reducing delays to treatment for complex or urgent cases.
- Improved resilience and flexibility: In a future development, pathologists will be able to access and report cases remotely, supporting home reporting and flexible working patterns.
- Reduced risk and admin burden: Eliminating routine slide transport reduces risk of damage or loss and cuts down manual handling and administrative tasks.
- Enhanced opportunities for education and research: Consolidated digital archives facilitate training, multidisciplinary review, and future AI-based diagnostic tools.
- Expected outcome: Shorter turnaround times for test results and improved patient care through faster, more accurate diagnostics.
Dr Charles House, medical director, medicine board and clinical SRO for the programme at UCLH, said: “A shift from analogue to digital is central to the government’s ambitions for NHS reform, aiming to improve efficiency, patient experience, and outcomes. Digital pathology will ensure NCL is at the forefront of digital innovation in pathology services.
By working together, we’re improving diagnostic services for patients and creating a more flexible, connected environment for our staff.”
Professor Manuel Rodriguez-Justo, digital pathology lead for cellular pathology at UCLH, said: “The digital pathology transformation programme will change histopathology practice, strengthening diagnostic accuracy and opening a huge opportunity for application of AI platforms in diagnosis, education and research”.
Professor Sebastian Brandner, clinical lead for neuropathology at Queen Square, added: “We are excited about the addition of neuropathology services to this programme later this year. Digital pathology is a major step forward for all pathology services. It will give our teams more flexibility, resilience, and access to a national network for training and collaboration.”
Next steps
The next stage of the programme will see digital pathology rolled out for Neuropathology at Queen Square, alongside the introduction of home reporting. These developments will support ongoing integration of digital tools and prepare pathology services for AI-enabled workflows.
Find out more on the UCLH website.
Guy’s and St Thomas’ NHS Foundation Trust is leading the way in robotic surgery, operating the UK’s largest robotic surgery centre. Each year, the Trust performs around 800 lung operations using advanced robotic technology to remove all or part of a diseased lung – improving patient outcomes and helping to reduce waiting times.
Earlier this year, Royal Brompton Hospital, part of Guy’s and St Thomas, successfully completed its first robotic-assisted lung surgery using the cutting-edge da Vinci Xi surgical system. This marked a significant milestone in the Trust’s thoracic surgery programme.
The da Vinci Xi system allows surgeons to control robotic arms to make tiny, precise incisions. This minimally invasive approach offers several benefits:
- Reduced post-operative pain
- Faster recovery times
- Shorter hospital stays
The introduction of robotic-assisted surgery is expected to enhance surgical efficiency, enabling the thoracic team at Royal Brompton to treat more patients each year.
Mr Simon Jordan, Consultant Thoracic Surgeon, commented: “This is a transformative moment for our thoracic surgery programme at Royal Brompton Hospital. We hope to improve patient outcomes and increase the number of patients we can treat.”
Robotics is also used across six other specialities including urology, gastrointestinal and transplant surgery. Since the first da Vinci system was installed in 2004, over 12,000 patients have benefitted from robotic-assisted procedures at the Trust.
Mr Routledge, a leading surgeon who uses robotic assistance in 99% of his procedures, said: “Patients are usually comfortable with robotic surgery once they understand it. Some imagine AI robots performing the entire operation – but that’s still science fiction.”
Read more:
- NHS robot surgery revolution ‘will help cut waiting times’ – The Express
- NHS robot surgery revolution ‘will help cut waiting times’ | UK | News | Express.co.uk
(Image: Four robotic arms are controlled by the surgeons with high precision – Jonathan Buckmaster)
Barking, Havering and Redbridge University Hospitals NHS Trust have installed two new robot dispensers to help patients get their medicines from their pharmacy quicker and more efficiently.
Once a dispenser requests a certain medicine, the robots send it directly to them. The dispenser would then label, and double check it against the prescription before it is given to the patient.
Later this year the team are also introducing electronic prescribing, meaning the pharmacy team can request medication from anywhere in the hospital, rather than going to collect paper prescriptions on our wards.
Read more on the Barking, Havering and Redbridge University Hospitals NHS Trust website.
Medical drone in-flight (Credit: Apian and Wing)
Urgent blood samples are being transported across London – using drones. Transporting samples for high-risk patients between Guy’s Hospital and St Thomas’ Hospital can take more than 30 minutes by road. Now, using high-tech drones, this can be achieved in less than two minutes.
The partnership between Guy’s and St Thomas’ NHS Foundation Trust, Apian and Wing has helped clinicians achieve quicker test results, enabling them to provide the best possible care – and get patients home sooner.
This is just one powerful example of how digital innovation in healthcare is directly improving outcomes for patients.
Read more on the Guy’s and St Thomas’ NHS Foundation Trust website.
 Using a robot to dispense medication has created a smoother and more efficient process for patients and pharmacists at Junction Pharmacy in Brixton.
Using a robot to dispense medication has created a smoother and more efficient process for patients and pharmacists at Junction Pharmacy in Brixton.
The robot provides greater efficiency and accuracy for by automatically dispensing medications and managing stock, allowing staff to focus on providing patient care.
Bhaveen Patel, Superintendent Pharmacist at Junction Pharmacy, said: “We have been here for just over 20 years now and this robot has been a game-changer.
“It has helped us to streamline our workflow. We have become more efficient, and our staff have more time to focus on their patient facing roles.”
Pharmacists have also been able to deliver additional services, including immunisations and vaccinations on-site helping to reduce GP and hospital waiting lists for these services.
Caroline Clarke, Regional Director for the NHS in London, said: “As we shift our focus from analogue to digital, I’m proud that London is home to some of the most innovative services, pioneering new ways of using technology to deliver high quality and accessible care for everyone.”
Read our press release on Digital innovation boosting NHS productivity in London.
A London-wide study led by led by Great Ormond Street Hospital’s Innovation Unit, GOSH DRIVE, found that ambient voice technology can reduce admin burden for clinicians improve the quality of face-to-face interactions between clinicians and patients.
Thanks to the automated note taking, clinicians can give their full attention to their patients without risking the quality of their notes or letters.
Dr Maaike Kusters, Paediatric Immunology Consultant, who took part in the trial at GOSH said: “The patients I see in my clinics have very complex medical conditions and it’s so important to make sure I capture what we discuss in our appointments accurately, but often this means I am typing rather than looking directly at my patient and their family.
“Using the AI tool meant I could sit closer to them face-to-face and really focus on what they were sharing with me, without compromising on the quality of documentation.”
Following this early success, the team have expanded the programme to include 9 NHS sites across London.
Over 17,000 patient encounters were evaluated across a diverse range of sites including hospitals, GP practices, mental health services and ambulance teams.
Key findings include:
- 23.5% more time spent directly with patients
- 8.15% reduction in total appointment time
- 35% reduction in clinician overwhelm from notetaking
- results from A&E showed particularly impressive results with 13.4% increase in patients seen per shift, with economic modelling showing millions of pounds worth of cost benefits from unlocked activity if scaled.
Dr Shankar Sridharan, Chief Clinical Information Officer at GOSH said: “This trial is significant as it shows the NHS can lead the way in safely adopting AI. Innovation can’t happen in isolation and by working collaboratively to test this technology across London – from hospitals to ambulances – we’ve proven it can work at scale and make a real difference for both patients and clinicians.”
The research has shaped NHS England’s national guidance on AI-enabled scribing, contributed to the Government’s 10-year Health Plan, and informed the creation of the NHS T.E.S.T. Framework for evaluating AI in healthcare.
Read more on the Great Ormond Street Hospital for Children NHS Foundation Trust website.
See how AI is giving clinicians more face-to-face time with patients
Barking, Havering and Redbridge University Hospitals NHS Trust have performed over 500 robotic operations for conditions including prolapse, heavy periods and incontinence, providing patients with quicker recovery times and better outcomes.
A typical robotic surgery lasts between one and two hours depending on how complex the condition is. The surgeon operates from a console and controls the robot, supported by an assistant.
Compared to traditional laparoscopic surgery, the robotic method offers greater precision for surgeons, especially for more complex cases.
Roopa Nair, our Clinical Director for Women’s Health and Lead for Robotic Gynaecology, said: “It was really heartening to see the interest in women’s health, and being able to offer this service locally means women no longer need to travel elsewhere. It’s encouraging to have the support of our local MP and mayor and it shows their commitment to advancing care for women.”
Read more on the Barking, Havering and Redbridge University Hospitals NHS Trust website.
Experts at King’s College Hospital and King’s College London are using robot radiotherapy to improve patients’ experience while also reducing cost. The new robot system treats wet neovascular age-related macular degeneration (AMD) by administering a one-off, minimally invasive dose of radiation, followed by patients’ routine treatment with injections into their eye.
The results found that patients who had the robotic radiotherapy required fewer injections to control their disease compared to standard treatment.
Read more on the King’s College Hospital NHS Foundation Trusts website.
A new video messaging app has launched at King’s College Hospital and Princess Royal University Hospital (PRUH) is helping families receive regular updates of their premature babies.
The app, allows staff on neonatal intensive care units at King’s and the PRUH to send regular photo and video updates securely to families, allowing them to see play and therapy sessions, baths and feeding times. Parents and families can also use the app to ask questions and receive important updates about their baby’s progress.
Dr Anusha Arasu, Consultant in Neonatal Medicine at King’s College Hospital NHS Foundation Trust, said: “A stay on a neonatal unit can be one of the most stressful times for a family, but we can now support parents to be more involved, and more connected to their baby’s care, as well as making a positive impact in delivering family centred care, even when they are not able to be at hospital. The app not only allows us to share photographs and updates with parents, but helps to reduce separation anxiety and allows the whole family to create and build an emotional bond with their baby.”
Jade has been using the app to receive updates on her twin daughters Tennesse and Tallulah, who were born prematurely at 32 weeks. She said: “It has been really hard to leave my girls for any amount of time. Seeing photos of them both doing well is a joy and gives extra reassurance.”
Read more on the King’s College Hospital NHS Foundation Trust website.
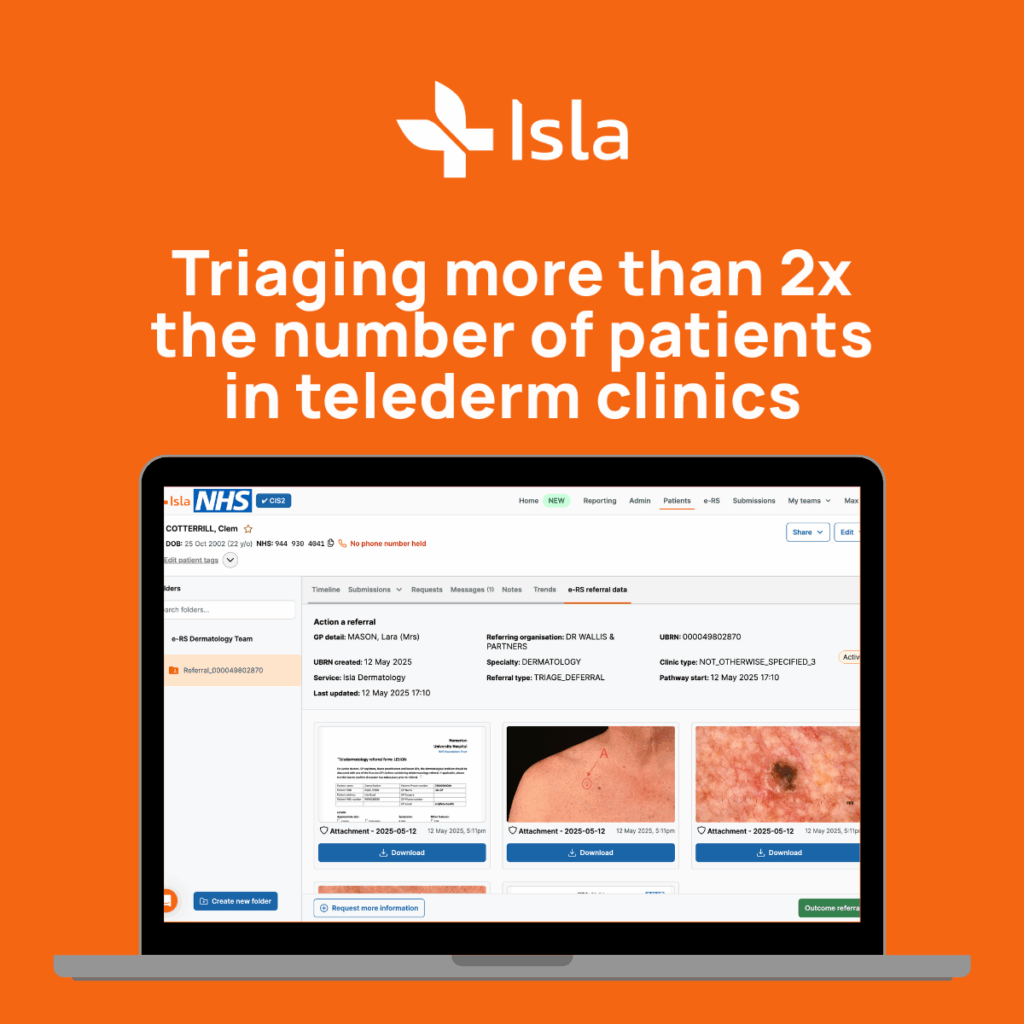
Homerton Healthcare NHS Foundation Trust are reviewing twice as many referrals per clinic, thanks to a new digital pathway for urgent suspected skin cancer.
Isla’s digital pathway supports faster and more confident decision-making by allowing GPs to capture high-quality images and clinical information from patients. Those images and forms are sent securely to Homerton for review through the NHS e-Referral Service (e-RS), with digital consent replacing paper-based processes and everything saved directly into the patient’s record.
For patients this means quicker responses and fewer delays. For clinicians, it means less admin, fewer duplications, and a clearer picture at the point of triage.
Angela Wong, Chief Medical Officer at the North East London Cancer Alliance, said:“Our top priorities as a cancer alliance are to deliver faster diagnostic results, detect cancer at an earlier and more treatable stage, and tackle health inequalities across our communities.
“By adopting ISLA’s digital platform for suspected skin cancer, we’re taking a significant step forward in achieving these goals. This innovation will help strengthen our position as one of the leading cancer alliances in the country.”
Find out more on the North East London cancer Alliance website.
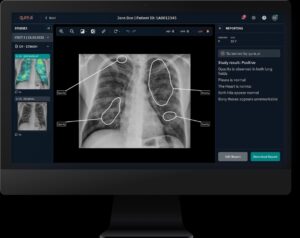
The North East London Cancer Alliance is leading a pioneering initiative to integrate Artificial Intelligence (AI) into cancer diagnostic pathways, aiming to deliver faster and more accurate results for patients.
In collaboration with Barts Health NHS Trust, Barking, Havering and Redbridge University Hospitals NHS Trust, and Homerton Healthcare NHS Foundation Trust, the project focuses on reducing the wait time for chest X-ray results. For scans with significant findings, turnaround times are expected to fall from three weeks to just three days.
By using AI to prioritise and flag potential cancers earlier, clinicians can take quicker action and patients can begin treatment sooner. This not only supports earlier diagnosis and improved outcomes, but also helps reduce pressure on radiology teams by streamlining reporting processes.
Oliver Hawkins, Senior Project Manager for North East London Cancer Alliance, says: “It has been great working with Qure.ai and Sectra to deliver an AI-driven solution aimed at revolutionising diagnostic pathways in north east London. This provides patients with faster access to crucial diagnostic tests and improves overall healthcare delivery.”
West London NHS Trust community nurses are using AI tools to monitor, treat and escalate woundcare in the community.
The implementation of the Minuteful for Wound (MfW) AI digital wound management solution, means that clinicians can receive immediate support from colleagues, who can review images remotely and provide real-time advice. For managers, the system offers the ability to generate detailed reports on healing rates, improvements, deteriorations, and overall progress, enabling them to monitor outcomes more effectively and ensure better care delivery.
A matron from the continence and tissue viability team said: “Using the app, our teams can now see wounds in real time and offer accurate clinical advice straight away. AI will never replace clinical judgment, but this tool enhances it—it’s transforming care delivery!”
Since implementing the MfW AI technology in July 2022, the programme has:
- Treated 8,605 wound and supported the care of more than 3,457 patients ensuring more consistent management, timely intervention, and seamless patient experience throughout the care journey.
- Avoided 29 in-person visits by using the ‘senior feedback’ feature that was launched in January 2025.
- Saved 5.30 minutes per consultation
- Carried out 64,599 assessments
The West London NHS Trust/Healthy.io collaboration was highly commended in the HTN AI and Data Awards 2025 for its work on the implementation of this solution.
 The Royal Free London is the first NHS trust in the country to introduce the Magneto laser – a new, advanced machine that removes kidney stones with greater speed and precision.
The Royal Free London is the first NHS trust in the country to introduce the Magneto laser – a new, advanced machine that removes kidney stones with greater speed and precision.
This technology offers improved control for surgeons, allowing them to break down kidney stones into fine dust without displacing them during the procedure. By doing so, it reduces the risk of larger fragments remaining, which can lead to repeat treatments.
Traditional holmium laser treatments often left larger residual fragments, requiring some patients to undergo additional procedures.
The introduction of the Magneto laser marks a significant step forward in patient care, helping to streamline treatment and reduce the likelihood of complications.
Leye Ajayi, clinical service lead for urology, said: “The most significant thing is that the Magneto machine gives you control and much more power while offering you treatment options and efficiency. The high-power pulse modulation gives the surgeon different settings and allows for individualised stone treatment, so we can break the stones into fragments, into small popcorn pieces or into dust.
“Because it’s so powerful, we can laser larger stones in one sitting and reduce the need for second completion procedures for patients, which they often would have with the standard machine.”
Read more on the Royal Free London NHS Foundation Trust website.
Chelsea and Westminster Hospital NHS Foundation Trust is harnessing cutting-edge digital technology to transform skin cancer care, using global-first autonomous AI technology to identify harmless (benign) skin lesions without the need for dermatologist review.
The AI system, known as DERM and developed by Skin Analytics, uses high-quality dermoscopic imaging to assess skin moles and lesions. With an accuracy rate of 97% for detecting skin cancer and 99.96% for ruling out melanoma, DERM performs at a level comparable to specialist clinicians.
Patients with benign results can now be discharged on the same day, reducing anxiety and providing quicker reassurance. By safely identifying these cases, the Trust aims to free up more than 30% of urgent skin cancer appointments, helping prioritise those most in need of further investigation or treatment.
Read more on the Chelsea and Westminster Hospital NHS Foundation Trust website.
Read more about the teledermatology service as featured in The Standard and The Times.
Digital innovation is reshaping the way community pharmacies operate—bringing measurable improvements in efficiency, staff wellbeing, and patient outcomes.
In South East London, one community pharmacy is leading the way by integrating advanced technologies into daily practice. These innovations are streamlining operations, empowering pharmacy teams, and enhancing the quality of care delivered to local residents.
Key innovations driving transformation:
- AI-powered Patient Medication Record (PMR) system: This NHS-accredited system enables 98% paperless dispensing. It performs clinical safety checks in seconds, helping pharmacists identify risks early and improve patient safety.
- Integrated dispensing robot: Fully connected to the PMR system, this robot enhances accuracy, speed, and dispensing volume, significantly reducing manual workload.
- E-retrieval system: Patients receive text or email notifications when their prescriptions are ready. The system also supports Real-Time Exemption Checker (RTEC) functionality at the point of collection, improving convenience and compliance.
- Ambient voice technology pilot: This innovation captures and summarises consultations, allowing pharmacists to focus more on patient interaction and care delivery.
- AI-driven clinical service templates: Using trusted sources such as NICE’s Clinical Knowledge Summaries, these templates guide consultations and generate PDF summaries for patients, supporting consistent and high-quality care.
These innovations underscore the potential for scalable digital solutions to enhance pharmacy services and deliver better outcomes for patients and communities alike.
UCLH and University College London (UCL) have developed a digital decision-making app, MENO.pause to help clinicians manage menopause symptoms in the best way for individual patients’ health conditions. The project has been supported in part by the North Central London Cancer Alliance Innovation Fund.
The app uses the most up-to-date national and international guidelines from the National Institute for Health and Excellence (NICE), British Menopause Society (BMS) and the British Gynaecological Cancer Society (BGCS) to assist healthcare professionals in GP surgeries and hospitals with providing high-quality, evidence-based treatment options for patients. This includes patients who have undergone cancer treatment or who have a high genetic risk of cancer.
Dr Shibani Nicum, honorary medical oncologist at UCLH and associate professor of oncology UCL, founder and project lead for MENO.pause, said: “We are committed to providing the highest quality menopause care across the country and are delighted to have launched the MENO.pause app, which transforms national menopause guidance into clear, step-by-step decision-making support.
Read more on the University College London Hospitals NHS Foundation Trust.