A supporting document to the 2025/26 NHS Payment Scheme
1. Introduction
Community services are often defined by what they are not. Although services in different organisations may share a name, they frequently have different professional definitions and modes of delivery across England. The development of community currencies presents an opportunity to focus on needs-based systems of service design, delivery, and payment.
Development of community currencies began in 2017 and was subsequently published by NHS England in 2019 (A New Approach To Supporting Community Healthcare Funding). Five distinct patient groups were identified and defined through discussions with the clinical leadership in NHS England and other stakeholders.
Since April 2020, currency development was reviewed, due in part to the COVID-19 pandemic and the impact that this had on testing. Through this review, a refreshed scheme of work was produced, in line with policy in a post-COVID context. As such, the original five currency models have been further developed and expanded to reflect progress in the sector and national priorities.
The community currencies programme of work now contains the following seven currency models, which are explained in detail in this document:
- Adult Frailty (see Section 2.1)
- Adult Last Year of Life (see Section 2.2)
- Adult Long-Term Conditions (see Section 2.3)
- Adult Short-Term Interventions (see Section 2.4)
- Children and Young People with Disabilities or Long-Term Conditions (see Section 3.2)
- Children and Young People – Shorter Term Interventions (see Section 3.3)
- Children and Young People – End of Life Care (see Section 3.4)
These Community Currency Models are patient segmentation tools that allow providers and systems to plan, fund, benchmark and improve their services in a more evidence-based way. Currency models are a key lever for achieving parity of esteem with the acute sector, with better outcomes reporting and robust costing to demonstrate value for money and improve the quality of care for patients. The currency models aim to support system-based collaborative working based on national policy ambitions, creating a common understanding of care provision and providing a standardised evidence-base which can support effective and equitable funding models.
Development is based on a number of key principles:
Currency models should be developed to support an understanding of the value of care delivery.
This is achieved by embedding intelligence in three parts:
- Currency models which identify patients within a population grouping, then segment based on the needs and complexity of the patient population.
- Provide an understanding of the resource and activity that is provided to support these needs.
- Offer an understanding of the quality/outcome of care through a validated outcome measure.
Through an understanding of these three elements, we can better understand the value of care, and consider the impact of changes to care provision, such as moving care into the community, or shifting resources to be proactive instead of reactive.
Currency models should place the patent at the centre.
Focus should be on understanding the needs of the patient and, where relevant, their carers and family, as well as the effects of their environment. This should also include a wider understanding of patient needs that are beyond the control of community services, such as their other physical or mental health conditions.
Currency models should be driven by available data wherever possible.
Models should avoid adding to data burden and be built focussing on data that already exists, and is required for submission to a national secondary use data set. Where this is not possible, data requirements should align with national policy direction and support greater intelligence for decision making.
Currency models should segment based on needs and complexity. Iterative development steps should be followed to support the sector to implement models at pace, and see value from their use.
This will mean that some models will need to be developed and applied in small steps, while others may be able to see faster-paced implementation.
The Community Currency Models have been developed with the input of working groups led by clinicians, finance and data teams and subject-matter experts. NHS England will continue working to develop granular patient-level currency models.
In 2025/26, we want providers to implement the currencies set out within this guidance and begin to use the currency models as part of planning and delivering services, benchmarking and as an evidence base for commissioning discussions. The models support equity across a system as a standardised language for collaboration. We will continue to develop these currency models with the support of the sector, as well as building and refining useful tools to embed the models in day-to-day operations.
During 2025/26 we will continue to engage the sector and work with stakeholders. We would like to work closely with systems as they implement the models. To be kept up to date with this work, or to learn more about how we could work together, please join our FutureNHS workspace.
1.1 What is a Currency?
A currency is a way of grouping patients or care activities into units that are clinically similar and have broadly similar resource needs and costs. Each unit of currency must be evidence-based, analytically identifiable and clinically meaningful. The currency must be rooted to the care the patient receives and be practical to implement.
Currencies can take different forms across the health sector. For example, they can be based on specific activity or the time period in which a patient would be treated for a condition. One example of an activity-based currency is an appendectomy carried out on an adult patient with a complications or comorbidities score of zero. The resources used to perform the procedure (staff, equipment, location and consumables such as dressings and drugs) are similar for different patients, so this type of appendectomy can be defined as a unit of currency. Another example of how a currency can work is through a year of care payment for patients who have cystic fibrosis. The complexity of the patient is banded into a number of groups which are linked to a payment for their year of care.
Currency is often confused with a price, however these two terms are not interchangeable. A currency refers to grouping healthcare activities into units of similar resource and clinical need. A price refers to a value assigned to a unit of currency or bundled package of care as part of a funding mechanism. This guidance focusses on a currency model.
The currency models for community care are developed to be needs based models which place the patient at the centre and aim to support a holistic view of their needs.
Further information can be found in the ‘An Introductory Guide to Currencies’ document, available on FutureNHS.
1.2 Aim of Introducing Currency Models
Currency models have been developed for many services, predominantly in the acute sector. There has been a long-term ambition to develop consistent currency models for the community sector, building on the varied care provided in the community and the personalised services developed to support local populations.
Community services lie at the heart of the vision for delivering the NHS Long Term Plan, the currency model aims to support better planning, benchmarking, and funding models to achieve this vision. Lord Darzi’s independent investigation highlights that the NHS is facing a range of challenges. The use of community currencies can support a better understanding of current provision and support planning towards the three fundamental shifts set out by Government:
- from hospital to community care
- from analogue to digital
- from treating sickness to preventing it
A key objective of developing community currency models is to ensure there is support for parity of services and various provider types, by creating standards for data and currency models which will support cross system working and collaboration.
Community currency models will:
- Support a standardised understanding of the patient population, by:
- Standardising data collection processes.
- Developing national data for use for wide range of uses.
- Provide a scalable resource (see Appendix 1) which uses standardised data for multiple purposes, by:
- Creating consistency in understanding data for planning and benchmarking.
- Links to other currency models to provide a holistic understanding of patient need and complexity.
- Support payment and commissioning, by:
- Creating an evidence base for payment, moving away from block contracting.
- Supporting future planning, commissioning and service design based on population need.
- Providing a basis for costing care provision.
1.3 Benefits of Introducing Currency Models
1.3.1 Understanding Patient Need and Complexity
The implementation of currency models has the potential to benefit clinical teams in several ways, from understanding their patient population to anticipating demand and adapting their services accordingly, to using consistent assessment metrics.
At a patient level, the consistent use of standardised language and assessments allows the consistent mapping of a patients journey or trajectory over time. These models provide a method to track a patient’s journey, identify current need and begin to anticipate their future care requirements.
Currency models encourage the collection of standardised information such as patient, referral, and assessment data. Collecting and submitting standardised data allows providers to be speaking the same language when it comes to their patient cohorts, allowing a shared understanding of a patient’s complexity across services.
1.3.2 Commissioning Effective Care
Currency models should support the commissioning process and be compatible with current and future payment systems. As providers are moving towards a blended payment model, currencies can be used as an evidence base. With the evolution of payment systems, currency models can support approaches such as population-based budgets, personal health budgets, and payment linked to patient outcomes. Alongside this, with an increased focus on collecting high-quality data, commissioners can benchmark between providers and use this to inform future payment arrangements.
Community currency models will provide a common and standardised language for all, meaning that they can be used by all providers across a system. When linked with outcomes this will provide a view of the overall value of care provision, as a comparison of need, provision, and experience. Tracking this information over time will provide a wealth of information to inform commissioning decisions and supports evidence-based commissioning.
1.3.3 System Planning
As we continue the shift towards mature system working, improving joined up care for patients is key. Improved and connected data from the voluntary, community and social enterprise sector would allow better system level planning, ensuring patients receive the care they need in the right setting. Integrated care systems (ICSs) can use the standardised patient, referral and assessment data to better understand their patient cohorts, allowing for a population health management approach to care provision.
A population-based approach will support systems to identify the complexity and therefore need of their populations. Understanding the complexity of patients, their families and carers will support planning based on resource requirements. This provides the opportunity to identify areas with high resource requirements, a data-based method of planning for resource allocation, and to support integrated multi-disciplinary team working which will support patients to access the most appropriate care in the right setting.
As data quality improves across regions, systems will have better access to information to evidence the need for investment and equity across all aspects of healthcare funded by the NHS. Future services can be planned using this evidence and the nuances across system footprints can be considered as part of the planning process.
The sharing of consistent currency data will also allow benchmarking across systems and provider collaboratives. Benchmarking in turn has the potential to identify opportunities for sharing best practice between providers and opening up conversations that could be used to inform improvements across all long-term condition care within a system or beyond.
1.3.4 Flow to National Systems
The community currencies and support the standardisation of underlying data which will be used across national teams. Based on the available data, national teams have the means to better understand defined population groups at a national level. They would also have the ability to segment the population accordingly to analyse underlying trends in health and health inequalities across regions. This will allow national teams to influence national policy to improve outcomes for their patient populations.
Currency data at a national level will allow national teams to gain an understanding of the resources required for patient populations. From this, national teams can provide support to systems to apportion allocations across secondary care to ensure funding can be utilised effectively and to help develop more detailed, evidence-based fixed payments as part of their contracts.
2. Adult Currency Models
2.1 The Frailty Currency Model
The Frailty Currency Model is a population-based currency model which places the patient at the centre. The model is designed to stratify the needs of patients into categories and structure regular assessments of patients to understand their progress and trajectory. The model aims to provide a consistent approach to understanding the delivery of high-quality care for patients living with frailty.
The Frailty model has three key components:
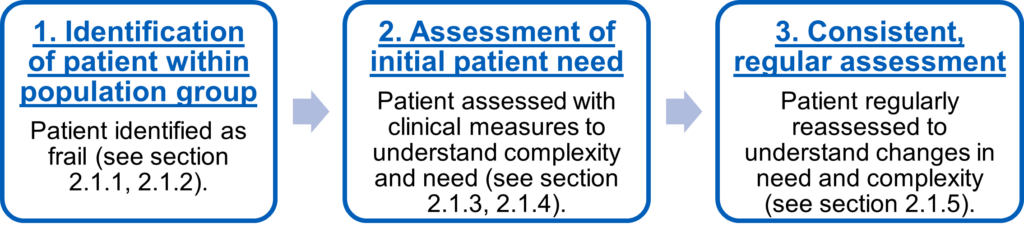
2.1.1 Defining the Population
The first step in using a currency model is to define the patients which are expected to form the population group. Frailty can be considered as a long-term health condition characterised by loss of physical, emotional and cognitive resilience as a result of the accumulation of multiple health deficits. Frailty is progressive, typically erodes functional, cognitive and/or emotional reserves and increases vulnerability to sudden loss of independence and adverse health outcomes following a comparatively minor stressor event such as an acute infection or injury. While severe frailty can be comparatively easy to recognise and diagnose, lesser degrees of frailty may be more difficult to differentiate from normal ageing.
People living with severe frailty frequently use services across health and social care and are particularly vulnerable to adverse outcomes such as unplanned admissions to hospital, care home admission, developing a new disability or death. For some, these adverse outcomes could be avoided through proactive identification, timely holistic assessment (such as Comprehensive Geriatric assessment), personalised care planning and targeted support and interventions delivered through Integrated neighbourhood teams in community.
To help find people who could benefit most from proactive care, local areas should use evidence-based risk prediction tools and clinical validation, supplemented with local knowledge.
2.1.2 Identifying Patients
Frailty can be identified either by assessing those who present to health and care services, or on a population basis, through risk stratification tools where a more systematic approach is taken to proactively identifying the population cohort most at risk of health deterioration. Patients can be identified using the Electronic Frailty Index (eFI) or other appropriate risk stratification tools which use routine health record data to automatically calculate a score which can identify whether a person is likely to be fit (not frail) or living with mild, moderate or severe frailty or other risk stratification tools could be used to identify population cohorts that may be living with frailty at a primary care level. When the eFI identifies an individual who may be living with frailty, direct clinical validation through assessment and judgment should be applied to confirm a diagnosis. Clinical validation tools could be used for this (eg, a Clinical Frailty Scale such as the Rockwood frailty scale).
However, there are limitations associated with the eFI tool, as it has the potential to miss a percentage of older people living with frailty because it relies on numbers of completed admissions and so may not identify patients with underlying risk of adverse health outcomes prior to admission. GPs are mandated to consider eFI for all patients over the age of 65 but it should be recognised that frailty can be present in those under the age of 65, especially in areas of deprivation.
It is also important to acknowledge that not all frailty diagnoses are identified in a primary care setting. Other methods of identification can be through hospital admissions or through A&E. An example of this would be a patient who would have been admitted to A&E due to a fall against which a clinician could attribute a frailty diagnosis. Patients with frailty can also be identified through hospital admissions for other conditions and receive a frailty diagnosis as part of a wider set of conditions.
Early identification coupled with targeted support can help older people living with frailty to stay well and live independently for as long as possible.
Effective identification of people living with frailty should be done as part of a multi-disciplinary approach in primary care with the three aims of:
- Identifying individuals aged over 65 years who are living with frailty, and the degree of their condition (mild, moderate, severe).
- Identifying an individual from within the primary care team who will coordinate frailty care for those people who are living with the condition.
- Identifying the principle needs of the person living with frailty and selecting the most appropriate support, care, and interventions to meet those needs. This is likely to require holistic and comprehensive assessment -, personalised care and support planning to promote self-management where feasible, co-ordinated multi-professional interventions to address the person’s range of needs – to include issues such as social isolation and loneliness, and social care and support to meet care needs.
The eFI is a useful screening tool to understand the population cohort of those patients with frailty, however the Clinical Frailty Scale (CFS) allows clinicians to provide a clinical diagnosis and track the trajectory of the patient. Consistent use of these measures, along with local sharing of data will support the effective segmentation of patient groups and tracking of effective care.
2.1.3 Diagnose and assess frailty using the Clinical Frailty Scale
The CFS tool has been validated to assess frailty and optimise quality of life in adults over 65 years quickly and simply in a clinical setting. It requires data collection by observing the patient, mobilising, and inquiring about their habitual physical activity and ability. Assessment includes whether the patient can independently perform tasks such as bathing, dressing, housework, going upstairs, going out alone, going shopping, taking care of finances, taking medications, and preparing meals. A person with a score greater than four is considered frail.
The CFS can be found in Appendix 2.
In addition, frailty verification could be undertaken within appropriate clinics, e.g. flu/shingles vaccine clinics, chronic disease clinics. CFS can also be completed by community nurses/community matrons, or appropriate allied health professionals and fed back to the practice. It should be noted that a diagnosis of frailty requires clinical judgement and cannot be assumed on the basis of the eFI or any other scoring mechanism alone.
The CFS can also be used to score patients with dementia. Generally, the severity of dementia would correspond to the degree of frailty:
- Mild dementia – Patients with mild dementia can have common symptoms such as forgetting the details of a recent event, though remembering the event itself, repeating the same question / story and social withdrawal.
- Moderate dementia – Patients with moderate dementia would have their most recent memory impaired, though they can recall past life events well. They can manage aspects of personal care with prompting.
- Severe dementia – Patients cannot manage personal care without help.
- Very severe dementia – Patients or often bedfast and many are virtually mute.
2.1.4 A Proactive Care Approach
The Frailty currency model is supported by the development of the Proactive Care guidance. The guidance is intended for systems to use when designing and delivering proactive care. The target population for proactive care are those patients who are moderately or severely frail. Systems can adopt the proactive care framework alongside the Frailty currency model to ensure systems can adopt best practice when providing the care for this population cohort. As data for this population improves over time, systems can consider implementing outcome measures at a place or system level linked to the variable or outcome-based element of the blended payment model.
A proactive care approach across a system will support seamless transfer of care for patients across systems and services as required by patient need. A common understanding will also transfer with the patient, enabling a better understanding of need which can be grouped based on specific demographics to ensure positive outcomes for patients. Acknowledging that a patient with frailty may enter a number of services in a non-linear way as their needs fluctuate, having consistent CFS assessments will allow for a more consistent hand over when that does occur.
The sharing of a consistent complexity measure through the Clinical Frailty Score will also allow benchmarking across care provider collaboratives. Benchmarking in turn has the potential to identify opportunities for sharing best practice between providers and opening up conversations that could be used to inform improvements across all proactive care within a system or beyond. Tracking the needs of patients can be done across traditional boundaries, facilitating a consistent understanding of patients’ needs and how they react to intervention. This methodology can be used across all forms of care, including virtual wards to develop intelligence and understand the value of care provision.
2.1.5 Deriving the Frailty Currency Model
The use of the Clinical Frailty Scale allows a patient’s frailty to be tracked over a period of time to understand the level of resource they may require to manage their level of physical health for as long as possible. The time between the first and follow-up assessment determines the currency unit for that period of time and also indicates the trajectory of a patient’s frailty. Clinicians should review the CFS score of a patient based on a reasonable timescale to ensure their frailty trajectory is being tracked accordingly and the care plan can be adjusted to support the patient to stay well as long as possible.
The twelve currency units below reflect the changes in the updated CFS model as the four broad categories are Very Mild, Mild, Moderate, and Severe frailty. From currency units 1 – 9, the units are based on the initial assessment and follow-up assessment to fit into a subcategory of Recoverable, Stable, or Progressive. Units 10 – 12 differ, as there is an understanding that patients with severe frailty move towards end stage frailty where palliative and end of life care will be considered. Subsequent assessments will allow further currency units to be derived which would allow tracking the trajectory of a patient to be possible.
|
Currency |
Currency |
Clinical Frailty Scale |
|
CAF01A |
Very Mild – Recoverable |
(CFS = 4 at T0 and <4 at T) |
|
CAF01B |
Very Mild – Stable |
(CFS = 4 at T0 and at T) |
|
CAF01C |
Very Mild – Progressive |
(CFS = 4 at T0 and >4 at T) |
|
CAF02A |
Mild – Recoverable |
(CFS = 5 at T0 and <5 at T) |
|
CAF02B |
Mild – Stable |
(CFS = 5 at T0 and at T) |
|
CAF02C |
Mild – Progressive |
(CFS = 5 at T0 and >5 at T) |
|
CAF03A |
Moderate – Recoverable |
(CFS = 6 at T0 and <6 at T) |
|
CAF03B |
Moderate – Stable |
(CFS = 6 at T0 and at T) |
|
CAF03C |
Moderate – Progressive |
(CFS = 6 at T0 and >6 at T) |
|
CAF04A |
Severe – Stable |
(CFS = 7+ at T0 and 7 at T) |
|
CAF04B |
Severe – Progressive |
(CFS = 7+ at T0 and 8 at T) |
|
CAF04C |
Severe – End Stage Frailty |
(CFS = 7+ at T0 and 9 at T) |
T zero = At the start
T = timescale for re-assessment, to be agreed locally
In practice, if a patient with an initial CFS score of 6 and a follow-up score of 7, the currency would assign the patient to ‘Moderate – Progressive’ which covers the period from the initial assessment to the follow-up assessment. If the subsequent CFS score was eight, then the time between the second and third assessment would be categorised as ‘Severe – Progressive’.
A case study which demonstrates the currency model in practice can be found on FutureNHS.
2.1.6 Key data items
Identification of the population
These data items primarily identify the patient as part of the currency model population. The identification is linked to the primary diagnosis of the patient. Where the primary diagnosis is Frailty, or a level of frailty.
The following SNOMED CT codes can be used to identify a frail patient –
- Frailty – 248279007
- Mild Frailty – 925791000000100
- Moderate Frailty – 925831000000107
- Severe Frailty – 925861000000102
Patients could also be identified through other data items such as team type, service or with the existence of a valid clinical frailty scale score.
Segmenting the population
Patients are segmented based on the score of the Clinical Frailty Scale. The CFS scale maps the trajectory of the patient through their support. It is recommended that the clinical frailty scale is assessed during the first contact after referral, then when there is a material change in the patient’s frailty level. As a minimum, the patient should be assessed on a regular, locally agreed timeframe, for example, every three months.
Clinical Frailty Scale SNOMED CT code – 763264000
For more information on data requirements, please see Section 4.
2.2 The Adult Last Year of Life Currency Model
The Last Year of Life (LYOL) Currency Model is a population-based currency model which places the patient at the centre. The model is designed to stratify the needs of patients into categories based on their own needs, but also their environment, and the needs of carers and those important to them. The model aims to provide a consistent approach to understanding the delivery of high-quality palliative and end of life care.
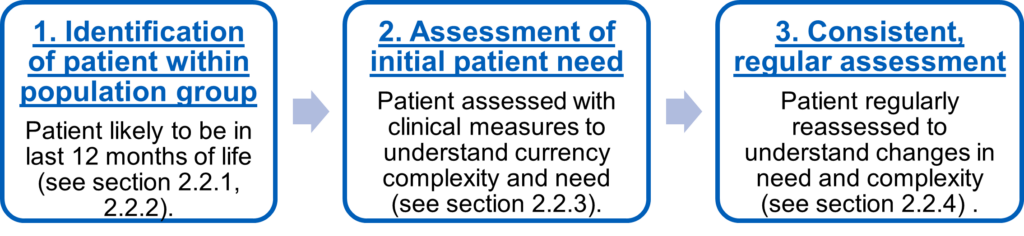
The LYOL model has three key components:
- Identification of patient within population group
- Assessment of initial patient need
- Consistent and regular assessment of needs as part of a patient’s journey
The Last Year of Life currency model is underpinned by the Palliative and End of Life Care (PEoLC) Commissioning and Investment Framework. Alongside this guidance, a tool has been developed to support systems to evaluate their current contracting arrangements. This will assist in:
- Providing clarity on the PEoLC services that are provided (not commissioned) and by whom.
- Inform future planning regarding contractual arrangements between provider and commissioner.
ICBs which have a detailed understanding of their current arrangements will be in a stronger position to identify future solutions to improve access, quality, and sustainability. The assessment tool is designed to structure an understanding of the current funding and service make up locally, to act as a starting point for future, evidence-based funding decisions. assess against the commissioning and investment framework. The framework itself was co-produced with a range of stakeholders. The framework aims to:
- Support ICBs as they identify and address any gaps in commissioning arrangements for palliative and end of life care and in meeting their legal duties.
- Classify palliative and end of life key services into commissioning categories with the intention of simplifying the process of agreeing commissioning responsibilities at a local level, and as a result, progress service transformation to improve access, quality, and sustainability of PEoLC services.
The PEoLC guidance can be found on Future NHS Palliative Care Network, users can request access via the Future NHS platform.
2.2.1 Defining the Population
For the Last Year of Life currency model, the population is defined as those adults identified as likely to be in the last 12 months of life and receiving palliative and/or end of life care. It is accepted that as this patient group covers a range of conditions and multi-morbidities and different methods for identification may be used dependent on local services and patient choice. A patient can be identified if they have a progressive disease, and as a consequence of that disease, the patient’s clinician would not be surprised if the patient were to die within 12 months. It is accepted that due to the variable nature of progression, a patient could live longer than 12 months whilst receiving palliative and end of life care, this would not exclude the person or their care from this population.
2.2.2 Identifying Patients
The NICE’s guidance on end-of-life care for adults recommends using a systematic approach to identify adults likely to be in the last 12 months of life. A systematic approach ensures identification is made in a timely manner, using tools such as the Gold Standards Framework Proactive Identification Guidance (PIG), Supportive and Palliative Care Indicators Tool (SPICT), EARLY Toolkit, Amber care bundle, PRADA (Proactive Risk-Based and Data-Driven Assessment of Patients at the End of Life).
Timely recognition also helps health and social care practitioners to begin personalised care and support planning conversations, including advance care planning, provide the care needed, and to support patient’s preferences for where they would like to be cared for and die.
Patients can be identified locally through patient records and with data shared from other providers. Other currency models will also provide standardised data which will support an understanding of a patient’s trajectory and support earlier interventions where feasible to do so.
2.2.3 Assessing the Needs of Patients
Once a patient has been identified, clinically validated needs assessments are used to understand the needs and complexity of the patient, their carers, those important to them, and their environment.
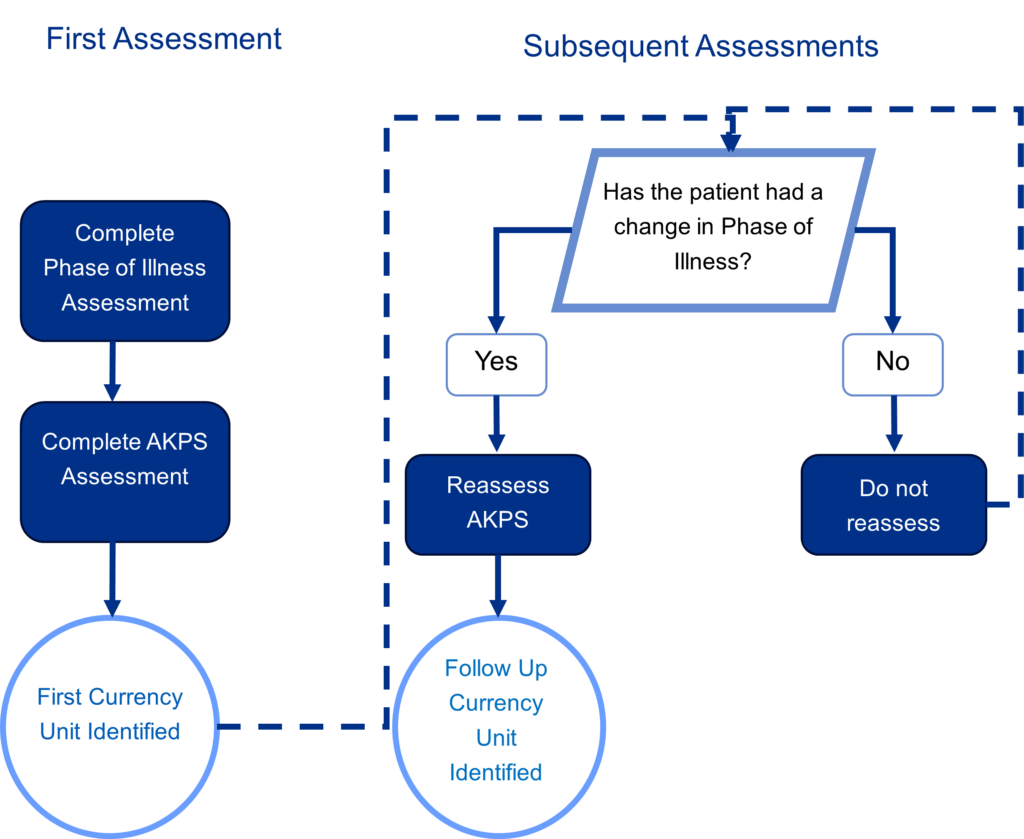
The LYOL currency model combines the Phase of Illness model (PoI) and Australian-modified Karnofsky performance scale (AKPS) to segment based on needs and complexity.
What is Palliative Phase of Illness?
Palliative Phase of Illness is a clinically validated assessment methodology which describes the urgency of care needs for a patient receiving palliative care. The model provides a holistic view of needs and complexity, as it assesses the needs of the patient, those important to them, carers, and the patient’s environment.
The Phase of Illness assessment model can be found in Appendix 2.
How often should Phase of Illness be assessed and recorded?
Phase of illness should be assessed on referral and then when there is a clinical change reflecting a move to a different phase of illness, or when a patient moves care setting. A change to the patient’s phase of illness should be recorded. At this point, assessing the patient based on the AKPS is recommended to understand the patient’s needs and complexity.
An example of the application of Phase of Illness – a patient who has been identified as likely to be in the last 12 months of life but has an agreed plan of care suited to their needs, along with their family or carer situation being stable would be assessed and placed in the ‘Stable’ category. Following a rapid increase in severity of a current problem, and difficulties with carer support which impacts their daily care, the patient’s care plan would be reassessed leading to an ‘Unstable’ phase of illness. At a later date, changes to the care plan have had a positive effect, the patient is reassessed as ‘stable’.
A case study which demonstrates the currency model in practice can be found on FutureNHS.
What is the Australian-modified Karnofsky performance scale?
Australian-modified Karnofsky performance scale (known as AKPS) is a measure of the patient’s functional status or ability to perform their activities of daily living. The measure has been clinically validated to work with both cancer and non-cancer patients.
AKPS is scored by clinical staff, and offers a 11-point scale, from 100% (representing full physical function) down to 0% (when the patient has died) in steps of 10%. It is based on observations of a patient’s ability to perform common tasks relating to activity, work, and self- care. Lower numbers indicate a reduced functional status.
The Australian-modified Karnofsky performance scale and scoring examples can be found in Appendix 2.
How to measure AKPS
AKPS should be measured at first assessment, when the palliative Phase of Illness Outcome Measure score changes, and at end of an episode of care, this includes patient discharge or death.
An episode of care ends when a patient moves setting, for example from hospital or hospice to home or vice versa. It also occurs when a patient dies.
When unsure of the score, it is helpful to consider the following questions:
- Have there been any changes today with the patient’s ability to undertake activities of daily living?
- Is the patient requiring more physical care today?
- How much time is the patient actually spending in bed?
An example of the application of AKPS
A patient has started an episode of care has had their Phase of illness assessed and has been assigned to the ‘Stable’. The patient is also assessed based on their ability to undertake their daily activities. As the patient can perform their usual daily tasks with effort but also shows some sign of disease, their initial AKPS score would be 80%.
Following a change in their Phase of Illness category to ‘Unstable’, the patient should be reassessed for the AKPS score. As they now require more assistance whilst managing their personal care, they will be scored at 60%.
Understanding Phase of Illness and AKPS
The Hull York Medical School have developed several resources found here which is useful in understanding various outcome measures including AKPS and Phase of Illness.
At a patient level, the consistent use of standardised assessments allows the consistent mapping of a patients journey or trajectory over time. The Phase of Illness and AKPS assessment measures used in the Last Year of Life currency provide an understanding of a patient’s current wellbeing and the complexity of their care needs. The model supports an ability to track a patient’s journey, identify current need and begin to anticipate their future care needs.
As with individual patients, the use of consistent Phase of Illness and AKPS data can be scaled up to give clinical teams an overview of their whole patient cohort. A detailed population overview allows clinicians to identify the resource required for patients with varying complexities, but also establish best practice where clinical interventions can be identified to keep patients healthy as long as possible.
A flow diagram of the assessment process can be found in Appendix 3.
2.2.4 Deriving the LYOL Currency Model
The combination of phase of illness and AKPS, segments patients into specific needs and complexity-based groups for patients identified as in the last 12 months of life. Phase of illness is used as the basis for understanding the care plan of a patient, followed by the use of AKPS which assesses the mobility and functional status of the patient. The combination of these metrics provides an understanding of overall need and complexity and indicates the level of resource usage throughout a patient’s care.
The ‘Stable’, ‘Unstable, and ‘Deteriorating’ phases of illness are linked to AKPS scores as resource usage will vary dependent on the patient’s functional status. AKPS functional status is not used within the ‘dying’ and ‘deceased’ phases. The ‘Deceased’ currency unit is in place to identify bereavement support for those close to the patient as illustrated in the phase of illness model.
A patient within the Last Year of Life population would be allocated to one of the currency units detailed below:
|
Currency |
Phase of |
AKPS |
|
CAE01A |
Stable |
High |
|
CAE01B |
Stable |
Medium |
|
CAE01C |
Stable |
Low |
|
CAE02A |
Unstable |
High |
|
CAE02B |
Unstable |
Medium |
|
CAE02C |
Unstable |
Low |
|
CAE03A |
Deteriorating |
High |
|
CAE03B |
Deteriorating |
Medium |
|
CAE03C |
Deteriorating |
Low |
|
CAE04Z |
Dying |
- |
|
CAE05Z |
Deceased |
- |
A case study example which illustrates when a patient would be identified as likely to be in the last 12 months of life, and how the assessment metrics would lead to currency units can be found on FutureNHS.
How can the derived currency units be used?
Palliative and end of life care providers are shifting towards a more collaborative approach across regions and systems, improving joined up care for patients. Improved and connected data from the voluntary, community and social enterprise sector would allow system level planning, ensuring patients receive the care they need in the right setting, providing care in the home, or in the community.
A collaborative palliative and end of life care approach across a system will support seamless transfer of care for patients across systems and services as required by patient need. A common understanding will also transfer with the patient, enabling a better understanding of need which can be grouped based on specific demographics to ensure positive outcomes for patients.
The sharing of consistent complexity measures such as Phase of Illness and AKPS will also allow benchmarking across care provider collaboratives. Benchmarking in turn has the potential to identify opportunities for sharing best practice between providers and opening up conversations that could be used to inform improvements across all palliative and end of life care within a system or beyond.
2.2.5 Key data items
Identification of the population
These data items primarily identify the patient as part of the currency model population. The identification can be linked to the primary diagnosis of the patient. Where the primary diagnosis is an illness which indicates a patient is towards the end of life. A patient could also be identified through and End of Life Data Flag, or the existence of end of life related assessment coding.
Segmenting the population
Patients are segmented based on the scores of the Phase of Illness and Australian-modified Karnofsky Performance Scale. The Phase of Illness score maps the trajectory of the patient based on their care plan towards the end of life. The AKPS supports the PoI by measuring the functional status of a patient and therefore can derive the needs of a patient. It is recommended that the PoI and AKPS are assessed during the first contact after referral, and then when there is a change in the patient’s care plan. For the purposes of the currency model AKPS should only be reassessed if there is a change in PoI.
Phase of Illness SNOMED CT code – 1092801000000106
Australian-modified Karnofsky Performance Scale SNOMED CT code – 901541000000107
For more information on data requirements, please see Section 4.
2.3 The Long-Term Conditions Currency Model
2.3.1 Defining the Long-Term Conditions Currency Population
In May 2023, the Payment Development team at NHS England brought together a group of experts to form a working group for the purposes of defining the parameters of a currency model for those with a long-term condition.
The group recommended that development should focus on a population defined as, ‘A Long-Term Physical Health Condition (also known as a Chronic Condition) is a health problem that requires ongoing management over a period of years or decades and is one that cannot currently be cured but can be controlled with the use of medication and/or other therapies’.
As part of this population, it was recognised that patients will be present across multiple currency areas and that this needed to be understood as part of the development of the model. The whole patient approach of currency development takes this into account, accepting that the only way to understand the needs of a patient, is to bring together their needs across all their conditions, including physical and mental health. The currency aims to support this approach.
The model also takes into account that some patients will move into adult services with an existing long-term condition. Through this period, we should recognise the additional complexity of transitioning into adult services and the impact on resources to ensure that this process is managed well.
Multiple Long-Term Conditions / Multimorbidity
The Academy of Medical Sciences defines multimorbidity as:
The co-existence of two or more chronic conditions, each one of which is either:
- A physical non-communicable disease of long duration, such as a cardiovascular disease or cancer.
- A mental health condition of long duration, such as a mood disorder or dementia.
- An infectious disease of long duration, such as HIV or hepatitis C.
Multimorbidity is an expanding health challenge across the globe with the number of individuals living with more than one chronic condition increasing. Individuals with multiple long-term conditions (also known as multimorbidity), have been shown to have poorer health related quality of life, poorer physical function, greater psychological needs, greater use of healthcare resources and higher mortality than those with just one or no long-term conditions.
In 2025, we will consider the applicability of considering multimorbidity within the Long-Term Conditions currency model based on three distinct groups suggested by the NHS England Prevention Programme Board:
- Those with single conditions who are at high risk of developing other long-term conditions – with a focus on proactive prevention and lifestyle interventions in primary and community care. This includes interventions to reduce risk factors such as generic such as weight loss, increased physical activity and smoking cessation
- Those that are non-frail and living with multimorbidity – with a focus on management through primary and community care or if this has moved towards the ‘tipping point’, secondary care/specialist care outreach e.g:
- Lifestyle interventions in community settings
- Some coordination of treatment e.g. medication reviews
- Those that are frail and are living with multimorbidity – with a focus for this group (who have moved past the tipping point and which may include a proportion of younger people especially those that have associated substance abuse, although the group is predominantly older patients) can include a combination of good/extended primary care and specialist support e.g. more comprehensive care provided by specialist such as a geriatrician.
The consistent identification of patients with each long-term condition along with the presence of multimorbidity will allow clinical teams to plan for individual care. A collaborative approach for populations with long term conditions across a system can support seamless transfers of care for patients across systems and services as required by patient need.
2.3.2 Deriving the Long-Term Conditions Currency Model
Development of the Long-Term Conditions Currency Model will continue throughout 2025/2026 building on previous steps taken to define the long-term conditions population for the purposes of the currency model.
To move forward with the development of this currency model, high quality data submissions are required for a number of key items. These include patient identifiable data, referral, and assessment data. Most importantly, the consistent collection and reporting of high-quality patient diagnosis data is vital in identifying the patient population which will fall under the Long-Term Conditions community currency model.
The ask for 2025/26 is for a focus on identifying patients receiving care for a long-term condition, record this locally, and submit the data as part of national submissions. This data will be used initially to form a single currency unit for 2025/26, as set out within the Community Currencies Grouping Methodology on FutureNHS.
We would invite providers and systems to work alongside us in the year ahead to develop a long-term conditions currency. If you would like to get involved, please contact us via the Currencies FutureNHS Platform.
For more information on data requirements, please see Section 4.
2.4 The Short-Term Interventions Currency Model
2.4.1 Defining the Short-Term Conditions Currency Population
The Short-Term Interventions model seeks to identify individuals that are accessing community services but fall outside of those clearly defined currency groups. These patients will often be receiving short courses of support or treatment, often without an existing long-term condition. Examples could include a course of physiotherapy or re-ablement. This currency model is in development.
2.4.2 Data Collection
Throughout 2024/2025 we will work towards increasing the flow of consistent high quality community data. This will allow is to begin to identify the patient populations which will form the Short-Term Interventions currency grouping. We aim to improve collections of the following data items:
- Local Patient Identifiable Data
- Patient Referral and Assessment Data Items
- Primary Diagnosis (to identify the presence or absence of a long-term condition)
- Care Activity data such as the Community Care Activity Type data item (e.g Assessment, Clinical Intervention, Multidisciplinary Team Review)
These data items are a starting point for providers to build upon and will be expanded as there is an uptake in the effective use of community currencies. We intend to use the lack of identification of a long-term condition as a flag for the individual to be segmented into the Short Term Interventions population. This is dependent upon community data sets having a high level of completeness and including the accurate recording of long term conditions.
2.4.3 Complexity
Once this population can be reliably identified and defined, the Payment Team will continue to consider complexity measures that could be used to segment the Short-Term Interventions population.
Pervious methods identified have included Patient Activation Measure and Needs & Provision & Complexity Scale We continue to investigate the appropriateness of each measure and remain vigilant for alternative complexity measures for consideration.
3. Children and Young People Currency Models
3.1 Understanding the needs of Children and Young People
The Children & Young People’s (CYP) currency models began as a single model, considering the needs of children and young people with disabilities. To ensure we understand the varied needs for the population, Children & Young People’s currency development has now been divided into three streams:
- Children and Young People with Disabilities and/or Long-Term Conditions
- Children and Young People – Shorter Term Interventions
- Children and Young People – End of Life Support
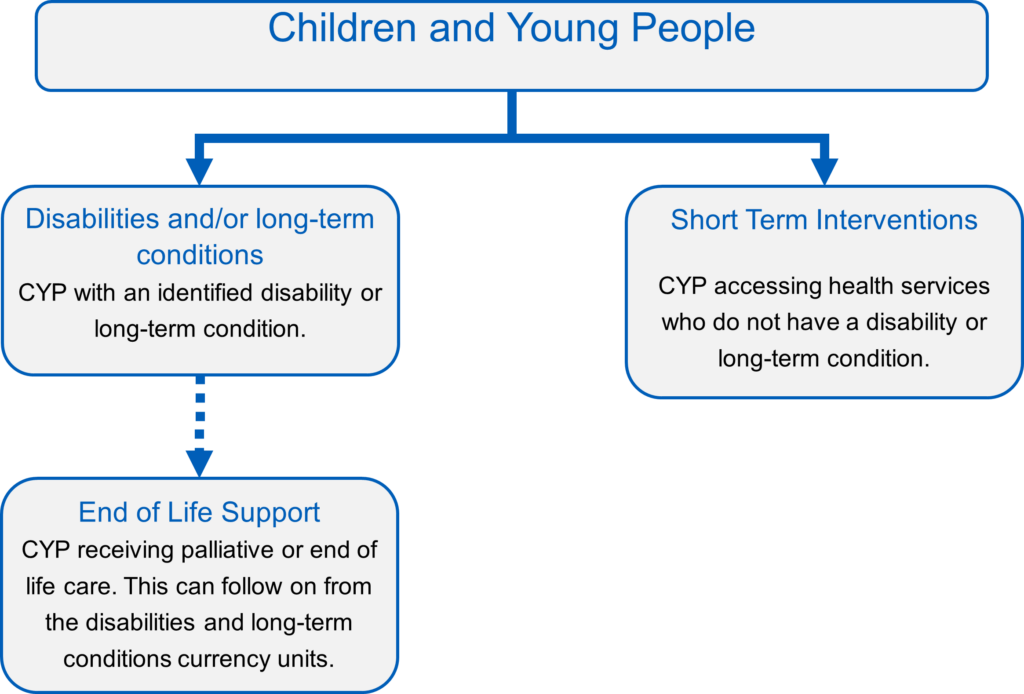
3.2 Children and young people with disabilities or long-term conditions
3.2.1 Key Definitions
The first step within our currency model is to identify our population. We do this using relevant definitions which can be supported using patient level data.
For the Children and young people with disabilities or long-term conditions currency we use two definitions, with an individual needing to meet at least one of these definitions for inclusion within the model.
Children with a disability definition
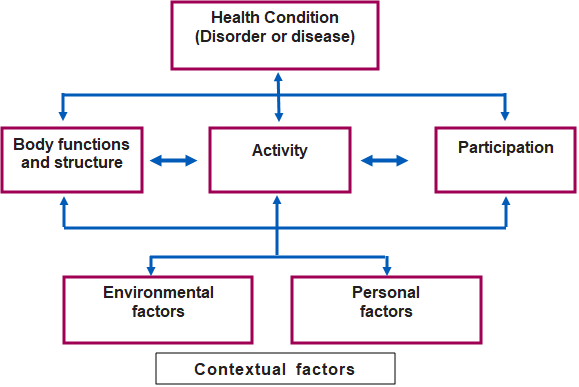
For children within this group we use the World Health Organisation of disability, “An umbrella term, covering impairments, activity limitations, and participation restrictions. An impairment is a problem in body function or structure; an activity limitation is a difficulty encountered by an individual in executing a task or action; while a participation restriction is a problem experienced by an individual in involvement in life situations.”
This brings together the ‘medical model’ of disability, which considers health conditions, body structure and function, with the ‘social model’ of disability, which considers aspects of the wider environment that can be disabling, such as physical factors and peoples’ attitudes.
Children with a long-term condition definition
For this group, our development group agreed that a combination of definitions was needed:
Firstly, The Department of Health definition of Long Term Condition, “A long-term condition (LTC) is a condition that cannot, at present, be cured but is controlled by medication and/or other treatment/therapies. LTCs are not just a health issue they can have a significant impact on a person’s ability to work and live a full life”.
Secondly, The Royal College of Paediatrics and Child Health comments: “Many long-term conditions develop during childhood; these children are more likely to develop mental health conditions and should be supported to navigate the transition from child into adult health services”. With the examples given of asthma, epilepsy, diabetes, cancer and disability / additional learning needs.
Finally, the Task Group added that many organisations also refer to a condition lasting more than a period of 12 months as an indicator that it may be a long-term condition. Therefore, we will also make reference to conditions that are “likely to last more than 12 months”.
Disabilities and long-term conditions can affect anyone at any time and can vary over time. These definitions include all children and young people with special educational needs and may be better understood as the interaction between different factors, as shown in Appendix 4.
3.2.2 The Currency Model
The Children & Young People with Disabilities or Long-Term Conditions currency model is based on work led by Dr Karen Horridge previously based at South Tyneside and Sunderland NHS Foundation Trust and previous Chair of the British Academy of Childhood Disability (BACD). This work was designed to expose variation in how the health needs of children and young people are described, and thus variation in how their health needs were being met. This work is critical for addressing the variation identified, to achieve the best possible outcomes for all children and young people.
The Royal College for Paediatrics and Child Health (RCPCH) have co-ordinated with speciality groups to develop a comprehensive terminology set for Children and Young People. RCPCH recruited a vast range of subspecialty leads, each tasked with compiling a list of needs and terminology that would be relevant to their specialty. These subgroups of terms were pulled together and compiled into the comprehensive expanded needs terminology set. Work is ongoing with NHS terminology specialists to ensure that every term identified has a corresponding SNOMED CT code.
Through collecting data about the multi-faceted needs of patients at the point of care, Dr Karen Horridge and colleagues’ research also led to the development of a Disabilities Complexity Scale. The Disabilities Complexity Scale identifies four needs categories which have a significant impact on the level of care and support required:
- Underlying health conditions
- Family reported needs
- Technology dependencies
- The need for round the clock care
The Children and Young People’s Needs Currency Model uses the number of needs identified through the paediatric terminology set in conjunction with the identification of needs assigned to one of the additional four disabilities complexity categories set as basis for the currency model:
|
Currency Units |
Level of Needs |
Disability Complexity Categories | ||
|
CCD01Z |
Low |
C – F | ||
|
CCD02A |
Medium |
C – F | ||
|
CCD02B |
Medium |
C – F – T | ||
|
CCD02C |
Medium |
C – F – R | ||
|
CCD02D |
Medium |
C – F – T – R | ||
|
CCD03A |
High |
C – F | ||
|
CCD03B |
High |
C – F – T | ||
|
CCD03C |
High |
C – F – R | ||
|
CCD03D |
High |
C – F – T – R | ||
|
Needs are defined in the Paediatric Needs Terminology Set – SNOMED-CT Codes | ||||
|
C = Health Condition |
|
T = Technology dependencies | ||
|
F = Family Reported Needs |
R = Round the clock care | |||
The level of need will be based on the overall number of recorded needs for the child or young person. Initial findings concluded that the number of needs that determined that differentiated between the low, medium and high level of need was 1-4, 5-10 and 11+ needs respectively. Following the expansion of the paediatric terminology set from 300 terms to over 3000, we will consider these boundaries again in 2025/26.
Tracking the comprehensive list of needs that a child or young person has, would allow for a more joined up approach to their care, where all providers will be able to access the same base information about the patient at the outset. Using the number of needs that a child or young person has in conjunction with the additional four listed complexity factors, allows the cohort of patients to be segmented into currency groups. The comprehensive list of needs will be inclusive of their social care, educational and mental health needs, allowing for a truly holistic view of the child or young person. This could be used to give an indication of the amount or type of resource that the child or young person may need throughout their care.
The paediatric terminology set includes a full subset of mental health needs. While CYP mental health services have their own currency, this will ensure that individuals with both physical and mental health needs are having their complete set of needs considered when seen in a physical health setting. Once again, the CYP currency models allow for standardised information to be shared across boundaries.
Similarly to the subset of mental health needs, there is also a small set of needs that would be used to identify a young person who is going through a transition process from a children’s to an adult’s service. Three SNOMED-CT codes are featured in the paediatric terminology set:
- Preparation for transition from children’s into adult care services. Used to identify young people who are being prepared for a transition into an adult service, including education on how to manage their own care.
- In transition from children’s into adult care service. Used to identify young people who’s care is being transferred between services.
- Destination support post transition from children’s into adult care services. Used to identify young people who’s care has transferred but are in receipt of post-transfer support
These codes will help to identify the number of young people who may require temporary additional support as they complete their transitions. It is important to note that these codes do not have to be used in a linear fashion. It may be that a young person has had an unsuccessful transfer of care and may need a little extra support. As such, they may flow through the preparation, transfer and destination support codes but then back to the preparation code once again.
As with individual patients, the use of consistent needs and complexity data can be scaled up to give clinical teams an overview of their whole patient cohort. A detailed population overview allows clinicians to identify the resource required for patients with varying complexities, but also establish best practice where clinical interventions can be identified to keep patients healthy as long as possible.
3.3 Children and young people – Shorter Term Interventions
The Children and Young People – Shorter Term Interventions currency model aims to identify child or young people who may be receiving care without an underlying long-term condition or disability.
Initial development work with experts, clinicians and national policy colleagues has indicated that the needs and complexity of a patient could be understood in a similar way to the Long Term Conditions and Disabilities model, by understanding the overall needs as identified by the patient, their family, carers and clinicians.
During 2025/26, we intend on developing this model and would welcome support from the sector in this process. If you would like to get involved, please contact us via FutureNHS. For implementation in 2025/26, we ask providers to ensure they collect related data which will help to ensure we understand patients that have underlying long term conditions or disabilities, and also focus on currency related data which will support the currency development process.
More information can be found within the Grouping Methodology on FutureNHS.
3.4 Children and Young People – End of Life Support
The third currency model for children and young people centres around children and young people who require end of life care and support. A full subset of needs has been included in the paediatric terminology set for end-of-life care. However, it has been recognised that a move towards a fully implemented needs-based model for children’s end of life care would require large scale change, especially for the vast number of smaller, independent providers who support children and young people. As such, the children and young people’s currency model has been designed in line with the adult’s end of life care currency model.
3.4.1 Phase of Illness
What is Palliative Phase of Illness?
Palliative Phase of Illness is a clinically validated assessment methodology which describes the urgency of care needs for a patient receiving palliative care. The model provides a holistic view of needs and complexity, as it assesses the needs of the patient, those important to them, carers, and the patient’s environment.
A breakdown of the categories in the Phase of Illness metric can be found in the Appendix 2.
How often should Phase of Illness be assessed and recorded?
Phase of illness should be assessed on referral and then when there is a clinical change reflecting a move to a different phase of illness, or when a patient moves care setting. A change to the patient’s phase of illness should be recorded. At this point, assessing the patient based on the AKPS is recommended to understand the patient’s needs and complexity.
How will Phase of Illness be used?
Phase of illness is an essential data item and is a dynamic assessment measure of the clinical stability of a patient. We would expect phase of illness to be assessed on referral, with secondary assessments when there is a clinical change reflecting a move to a different phase of illness, or when a patient moves care setting.
A change in phase of illness could signify a change in resource requirement. For example, a child or young person who has been consistently stable, may acquire an infection which causes their phase of illness to change to unstable. This will signify an additional requirement for support until the infection is under control and the patient returns to stable, or further support is required, and the child or young person moves to deteriorating.
The currency model for Children and Young People 0 End of Life Care is as follows:
Currency Unit | Phase of Illness |
|
CCE01Z |
Stable |
|
CCE02Z |
Unstable |
|
CCE03Z |
Deteriorating |
|
CCE04Z |
Dying |
|
CCE05Z |
Deceased |
3.4.2 Key Data Items
Identifying the Population
Ensuring completeness of key data fields will support better allocation of patients into the correct currency. This is set out in the Grouping Methodology shared on NHS Futures. We can also identify patients with key assessment data items and using data flags within national data sets.
Paediatric Terminology Set
The Paediatric Terminology Set will be published for use shortly on the NHS England Website.
4. Collecting and Submitting Currency-related Data
The NHS Long Term Plan supports the movement of services from acute to community settings where it will enable patients to have better options, support, and ensuring joined-up care is provided in the optimal care setting. However, there remain barriers to quality data available at regional and national levels to support these aims. The NHS Community Health Services Data Plan, published in April 2024, sets out plans to address this. The development of currency models will act as a supportive tool which can be applied at differing levels using consistent data.
Community currency models are designed to use existing data wherever possible, and therefore avoiding additional data burden. In some cases, subtle changes in the way data is collected on the front line will be required. Clinicians may need to move away or supplement narrative-based record keeping with the use of pre-defined fields for diagnosis and clinical assessments to ensure key assessment metrics can be captured consistently. This would allow teams, providers, and systems to use key data without extensive manipulation of local data and view consistent outputs from a single source.
The key focus of improving data should be at the point where it is entered into electronic records. The provision of correct and consistent data at this stage allows the data to be used throughout the organisation with minimal manipulation or coding, thus reducing data burden.
Data collected from the front line can be used for various purposes. The currency models are driven by data which clinicians can use to gain an understanding of the quality of care and how that can impact on patient outcomes in their last stage of life as the metrics track the care plan and functionality of patients. When currency models can be collated at a system level, the complexity of a patient can be tracked throughout their episode of care, across services and settings. Developing data sharing agreements within systems will enable wider comparisons and reduce duplicated data collection.
High quality standardised information should also be provided to relevant national data sets as set out in respective data standards. High quality national data supports effective decision making, policy planning and funding decisions. National data can also support wider benchmarking and analysis of service provision and best practice.
4.1 Community Services Data Set (CSDS)
The Community Services Data Set (CSDS) is a national secondary uses data set which re-uses clinical and operational data for purposes other than direct patient care. The CSDS Information Standard Notice Sets out submission expectations for providers of publicly funded Community Services. More information can be accessed here.
4.2 Community Faster Data Flows (FDF)
The FDF Programme (Faster Data Flows) aims to provide timely high-quality data to support decision making by implementing an automated, record-level daily data collection. It seeks to reduce the reporting burden on providers by enabling rationalisation of current data collections from NHS England and ICBs.
A phased approach to onboarding all CHS providers to Community FDF commenced in August 2024. Providers will flow a core specification of data into the Federated Data Platform (FDP) where it will be available to participating providers and their ICBs. All data items needed to segment into currency models are included with this core specification.
Community FDF will give a rapid view of any DQ issues, enabling providers to identify quickly where action needs to be taken and correct this data at source.
Decisions about the future of current national collections, including the CSDS, have not yet been made and providers continue to be legally mandated to submit to the CSDS. By May 2025, NHS England will review existing community datasets to inform decisions and plans regarding potential transition to automated, daily data flows.
Further information and guidance on Community FDF can be found on FutureNHS.
4.3 Data Definitions
The NHS Data Dictionary sets out national definitions for the extraction of community data about children and adults including:
- personal and demographic
- social and personal circumstances
- care event and screening activity
- diagnoses, including long-term conditions and disabilities
- scored assessments
Using nationally agreed terms and definitions supports system working and benchmarking, ensuring comparability. Combined with the use of SNOMED CT, this will facilitate quality data to be collected by clinicians and for this data to move seamlessly through local system to be used by systems and in community data collections without need for additional manipulation or coding. All data items needed to segment into currency models are included within national data.
5. Appendices
Appendix 1 – Grouping data for analysis
Table 4
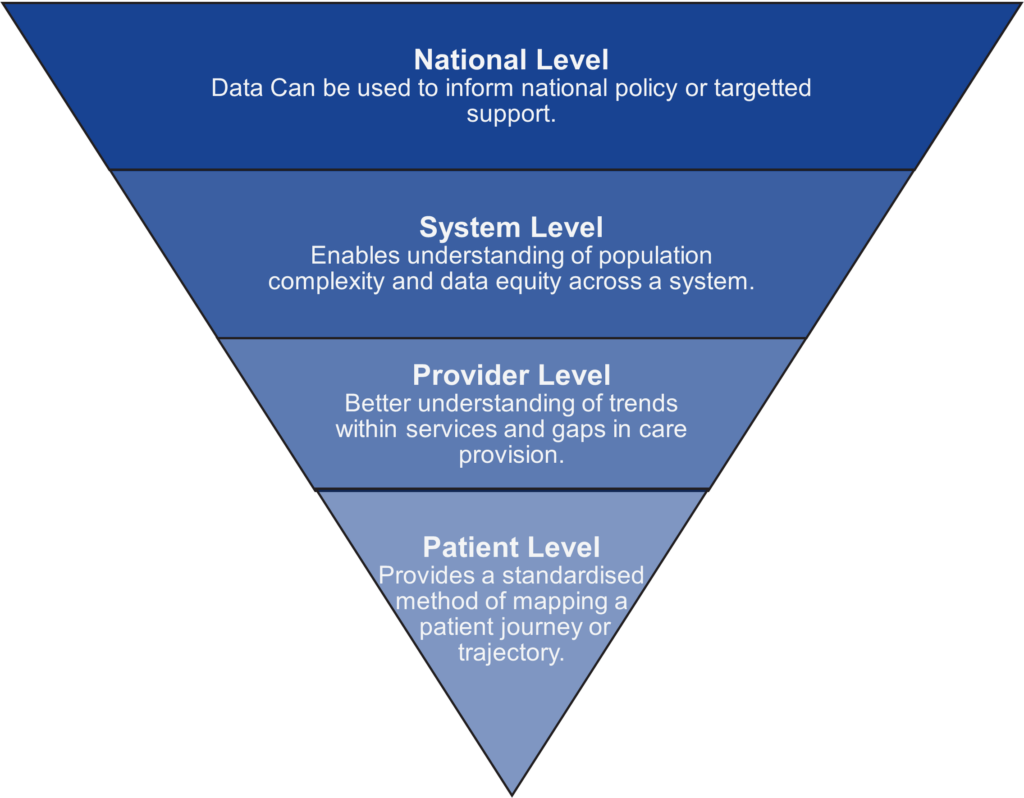
|
Patient Level | · Allows the identification of patient need using consistent language, using standardised SNOMED-CT coded data. · Provides a mechanism for consistent complexity assessment language to be applied for patients moving between providers and/or services. · Provides a standardised method of mapping a patient journey or trajectory over time. |
|
Provider Level | · Provides an understanding of the local patient population and complexity of this population, supporting a population health management approach · Supports a better understanding of trends within a service, and specific gaps in care provision · Provides an understanding of the use of resources, and of patients with complex, multi-faceted needs · Provides standardised data which supports conversations with other providers and commissioners · Ensures independent and community providers have data which is comparable with acute providers. |
|
ICS Level | · Enables an understanding of population complexity which will facilitate decision making on allocation of resources across an ICS footprint · Using standardised, high quality data is the cornerstone of collaborative working, ensuring we understand consistent terms across boundaries. · Data equity across a system, evidences the need for investment and equity in all parts of the system · Provides a mechanism to support evidence based commissioning |
|
National Level | · Provides an understanding of local and national issues and overall changes in data over time. · Data can be used to support national policy or targeted support. Knowing we are using the same terminology supports data sharing, ensuring there is confidence in the data received. · Provides a methodology to support the Government’s three fundamental shifts following the Darzi report: From hospital to community care, from analogue to digital & from treating sickness to prevention |
Community currency models have been designed to work at the varying levels based on stakeholders need to ensure planning and decision making can be made using high quality information. The currency model scales data collected by patient facing colleagues to meet the varied needs of the system.
Fig. 1 How can data be grouped for various uses
Appendix 2 – Assessment Details
Clinical Frailty Scale
|
1 |
Very Fit |
People who are robust, active, energetic, and motivated. They commonly exercise regularly and are among the fittest for their age. |
|
2 |
Well |
People who have no active disease symptoms but are less fit than category one. Often, they exercise or are very active occasionally, e.g. seasonally. |
|
3 |
Managing Well | People whose medical problems are well controlled but are not regularly active beyond routine walking. |
|
4 |
Living with Very Mild Frailty |
Previously “Vulnerable,” this category marks early transition from complete independence. While not dependant on others for daily help, often symptoms limit activities. A common complaint is being “slowed up”, and/or being tired during the day. |
|
5 |
Living with Mild Frailty | These people often have more evident slowing, and need help in high order IADLS (finances, transportation, heavy housework, medications). Typically, mild frailty progressively impairs shopping and walking outside alone, meal preparation, medication, and housework. |
|
6 |
Living with Moderate Frailty |
People who need help with all outside activities and with keeping house. Inside, they often have problems with stairs, need help bathing and might need minimal assistance (cuing, standby) with dressing). |
|
7 |
Living with Severe Frailty |
Completely dependent for personal care, from whatever cause (Physical or cognitive). Even so, they seem stable and not at high risk of dying (within – 6 months). |
|
8 |
Living with very Severe Frailty |
Completely dependent for personal care and approaching the end of life. Typically, they could not recover even from a minor illness. |
|
9 |
Terminally Ill |
Approaching the end of life. This category applies to people with a life expectancy <6 months, who are not otherwise evidently frail. |
Phase of Illness Model
Table 1 table defines the attributes of each phase of illness, reflecting the patient’s needs, the needs of those important to them and carers, and the circumstances of their environment:
1. Stable If all symptoms and concerns are controlled or managed, and no review is required (unless something changes) | ||
|
Start of Phase |
End of Phase |
Example |
Patient problems and symptoms are adequately controlled by established plan of care and · Further interventions planned to maintain symptom control and quality of life, and · Family/carer situation is relatively stable, and no new issues are apparent |
The needs of the patient and or family/ carer increase, requiring changes to the existing care plan (i.e. the patient is now unstable, deteriorating or terminal) | Symptoms and other concerns are well controlled and stable. Carers and those important to the patient are aware of how to access support in the event of change. All controlled and not causing any concerns (patient and/or those important to the patient) |
2. Unstable If urgent, unexpected symptoms or issues which need intervention quickly (usually that day) | ||
|
Start of Phase |
End of Phase |
Example |
An urgent change in the plan of care or emergency treatment is required because: · Patient experiences a new problem that was not anticipated in the existing plan of care · Patient experiences a rapid increase in the severity of a current problem· Those important to the person/carers’ experience changes which impact on patient care | · The new care plan is in place, it has been reviewed and no further changes to the care plan are required. This does not necessarily mean that the symptom/ crisis has fully resolved but there is a clear diagnosis and plan of care (i.e. the patient is now stable or deteriorating), and/or Death is likely within days (i.e. patient is now terminal) |
Symptoms and overall condition need regular review because they are unpredictable and at risk of worsening quickly. Informal carers need additional support as condition is unpredictable. Urgent and unexpected issues (patient and/or those important to the person) |
3. Deteriorating There are gradual and more expected symptoms or issues which need regular but not urgent review and assessment. (Note that this is not the same as a ‘deteriorating patient’ or ‘deteriorating illness’, it has quite a different meaning here. Think of the care plan, not the condition or illness) | ||
|
Start of Phase |
End of Phase |
Example |
The care plan is addressing anticipated needs but requires periodic review because: · Patient’s overall function is declining · Patient experiences an anticipated and gradual worsening of existing problem · Patient experiences a new but anticipated problem · Those important to the person/carers experience gradual worsening distress that is anticipated but impacts on the patient care | Patient condition plateaus (i.e. patient is now stable) or: · An urgent change in the care plan or emergency treatment is required and/or · Family/ carers experience a sudden change in their situation that impacts on patient care, and requires urgent intervention (i.e. patient is now unstable) orDeath is likely within days (i.e. patient is now terminal) | Symptoms and overall condition are gradually worsening, but in an anticipated way. Informal carers may need pre-emptive support to facilitate on-going care Gradual and expected issues (patient and/or those important to the patient)
|
4. Dying If the patient is expected to die in the next few days, the care plan will be addressing end of life needs. | ||
|
Start of Phase |
End of Phase |
Example |
· Death is likely within days | · Patient dies or Patient condition changes and death is no longer likely within days (i.e. patient is now stable, or deteriorating) | Prognosis is assessed to be hours or days Review and re-assessment is frequent (daily or more than daily contact) |
5. Deceased The patient has died, after-death care is being provided to those important to the patient. | |
|
Start of Phase |
End of Phase |
|
Patient has died – bereavement care provided to family/carer is documented in the deceased patient’s clinical record. |
Once initial bereavement care and signposting has been provided. |
It is important to note:
- The first four Phases of Illness can occur in any order and may vary in duration.
- Patients may move between Phases in any sequence and the Phases do not last any set length of time.
- Phase of Illness relates to the plan of care, rather than the illness as demonstrated in Table 2.
- A patient may have two or more phases in any episode of care.
- The ‘stable’, ‘unstable’ and ‘deteriorating’ phases are not reliant on stage of disease or prognosis and may occur at any point in the illness trajectory, and in any order.
- Deteriorating phase is not the same as ‘a deteriorating patient’ as used in acute care. Its meaning here is related to the plan of care as above. ‘Dying’ Phase takes precedence over any other Phase.
Australian-modified Karnofsky performance scale (AKPS)
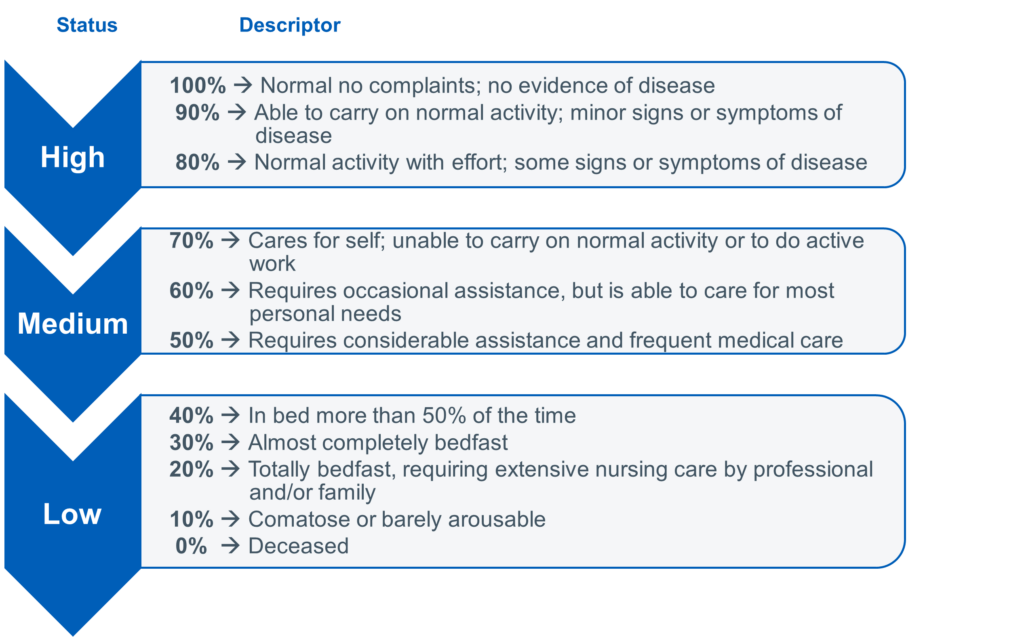
Following are examples of the most common scores with examples of use:
- The score of 70% indicates the patient being able to care for self, but unable to maintain normal activity. An example is being unable to maintain work or usual daily activities at home.
- The score of 60% indicates the patient cares for themselves the majority of the time, but occasionally needs some assistance. An example is a patient needing some help with daily activities.
- A score of 50% indicates that the patient needs help frequently. An example is the patient needing considerable help with mobility and personal care.
- A score of 40% indicates that the patient is in bed over half of the time because of functional impairment due to their illness.
- Scores of 30%, 20% and 10% indicate further reductions in levels of functioning.
Clinicians should record 0% at the time of death, so that the degree of change in functional status over the last days of life can be understood. This helps to understand how much change has occurred and what an individual patient and family have had to address in terms of change in functional status.
Appendix 3 – LYOL Assessment Flow Diagram
Appendix 4 – CYP contextual factors of disability diagram