Introduction
- This document is Annex C of the 2025/26 NHS Payment Scheme (NHSPS).
- This document describes best practice tariffs (BPTs) and gives detailed guidance on the implementation and eligibility criteria for each BPT.
Overview of best practice tariffs
- A BPT is usually a price that is designed to incentivise quality and cost-effective care. In the 2025/26 NHSPS, BPTs also form part of the aligned payment and incentive (API) and activity-based payment mechanisms (see ‘BPT pricing structure’ below).
- The first BPTs were introduced in 2010/11 following Lord Darzi’s 2008 review of the NHS, High quality care for all. The service areas covered by BPTs are:
- high impact (ie high volumes, significant variation in practice, or significant impact on patient outcomes)
- supported by a strong evidence base and clinical consensus on what constitutes best practice.
- The aim of BPTs is to reduce unwarranted variation in clinical quality and spread best practice. BPTs may introduce an alternative currency, including a description of activities that are associated with good patient outcomes.
- BPTs provide an incentive to move from usual care to best practice by creating a price differential between agreed best practice and usual care.
- Each BPT is different, tailored to the characteristics of clinical best practice for a patient condition and to the availability and quality of data. However, many BPTs share similar objectives, such as:
- avoiding unnecessary admissions
- delivering care in appropriate settings
- promoting provider quality accreditation
- improving quality of care.
- When they were initially introduced, BPT prices were paid, for activity meeting the criteria, as part of the ‘Payment by Results’ activity-based payment approach. This continued with the National Tariff. However, following the introduction of the aligned payment and incentive (API) blended payment in 2021/22, the operation of BPTs was repurposed so that they could be used in practice more effectively. This involved BPTs being part of the API variable element, adjusting payments to reflect actual levels of BPT achievement. BPTs continue to form part of the NHS Payment Scheme, both in connection with the calculation of the API and where unit prices are payable.
- For the 2025/26 NHSPS, there are two categories of BPT:
- Annual BPT – value of expected BPT achievement to be included in API fixed element, with annual adjustments as part of planning to reflect actual achievement.
- Elective activity BPT – for BPTs related to elective activity, to be transacted on an activity basis as part of API variable element or activity-based payment mechanism.
- The spinal surgery BPT operates as an elective activity BPT but should also be treated as an annual BPT for non-elective activity.
- Where we have nationally flowing data, we will publish data on BPTs and will work with systems partners to enable this.
- We will be evaluating the BPT changes and will take the findings into consideration for future payment schemes.
BPT pricing structure
- Some BPTs relate to specific healthcare resource groups (HRGs) while others are more detailed and relate to a subset of activity within an HRG (sub-HRG). The BPTs that are set at a more detailed level are identified by BPT ‘flags’ (listed in Annex A) and relate to a subset of activity covered by the high-level HRG. This document should be read in conjunction with Annex A.
- Table 1 summarises some key terms used about BPTs.
Table 1: Summary of terms used
|
Term used |
Description |
|
Conventional price |
The price that would apply if there were not a BPT or for activity covered by the HRG unrelated to the BPT (where set at sub-HRG level). |
|
BPT price |
The price paid for activity where the requirement(s) of the BPT are achieved. This will normally be higher than the conventional price. |
|
Base price |
The price paid for activity where the requirement(s) of the BPT are not achieved. This will normally be lower than the conventional price. |
|
Conditional top-up payment |
This is the difference between the BPT price and base price. For BPTs where SUS+ automates the base price, this is the amount to be added as a local adjustment where the BPT requirement(s) are met. For BPTs where SUS+ automates the BPT price, this is the amount to recover as a local adjustment where the BPT requirement(s) are not met. |
- For the purposes of validation, we do not generally specify achievement periods in the BPTs. Unless specified, achievement periods should be locally agreed, taking into account the availability of data and local reconciliation timescales and recognising achievement in a timely manner to ensure that improvements in care are appropriately incentivised.
- Long-stay payments apply to all relevant BPTs. The short stay emergency adjustment (SSEM) may apply to BPTs that are in part or in whole related to emergency care.
Short-stay emergency adjustments (SSEM) and BPTs
- The short-stay emergency adjustment (SSEM) is a mechanism for adjusting the price that would otherwise be payable for short-stay emergency spells (less than two days) where a longer length of stay would generally be expected.
- The adjustment should be made to unit prices used for activity where the aligned payment and incentive approach does not apply.
- The adjusted price is based on rules concerning the average length of stay for the HRG: the higher the average length of stay, the lower the price. These adjustments are set out in Annex D.
- For BPTs, the SSEM adjustment is not universally applicable because it only applies to diagnostic-driven HRGs. It does not apply, for example, when the BPT’s purpose is to reduce length of stay.
- Table 2 clarifies when the SSEM applies and how the adjustment is to be applied in each case.
Table 2: Application of SSEM
|
Best practice tariff |
SSEM applicable |
SUS+ applied |
Local adjustment required |
|
Adult asthma |
Yes |
To base price |
To conditional top-up |
|
Emergency laparotomy |
No – procedure driven |
n/a |
n/a |
|
COPD |
Yes |
To base price |
To conditional top-up |
|
NSTEMI |
No – procedure driven |
n/a |
n/a |
|
Acute stroke care |
No – policy exempt |
n/a |
n/a |
|
Diabetic ketoacidosis or hypoglycaemia |
Yes |
To base price |
To conditional top-up |
|
Fragility hip and femoral fracture |
No – policy exempt |
n/a |
n/a |
|
Heart failure |
Yes |
To base price |
To conditional top-up |
|
Primary hip and knee replacement outcomes |
No – procedure driven |
n/a |
n/a |
- Providers and commissioners should take the application of SSEM into account when agreeing local data flows and reconciliation processes. Where applicable, any local adjustment should be made at the same rate as the core spell (as defined in Annex A).
- The rest of this document gives detailed guidance on each BPT. The elective activity BPTs are presented first, then the annual BPTs.
Elective activity BPTs
- Right Procedure Right Place (Section 1)
- Endoscopy procedures (Section 2)
- Pleural effusion (Section 3)
- Primary hip and knee replacement (Section 4)
- Rapid colorectal diagnostic pathway (Section 5)
- Spinal surgery (Section 6)
Detailed guidance on Annual BPTs starts from Section 7.
1. Right Procedure Right Place
Purpose
- The Right Procedure Right Place (RPRP) BPT aims to support the movement of suitable procedures from day case (or elective) to outpatient, in order to drive efficiency and productivity and to reduce costs.
- The Getting it Right First Time (GIRFT) RPRP initiative initially promoted a “day case by default” approach. More recently, there has been a growing focus on movement of suitable procedures from day case to outpatient. This approach is often appropriate for less invasive procedures that require a less resource-intensive approach, for example, taking place in a treatment room rather than requiring a surgical theatre environment.
- This approach has the potential to deliver efficiencies by freeing up capacity in operating theatres. It can lead to cost savings for both providers, due to anticipated lower underlying costs when performing these procedures on an outpatient basis, and the NHS, by equalising prices for day case/elective and outpatient, which removes financial barriers to treating patients on an outpatient basis.
Design and criteria
- The RPRP BPT will apply to the procedure codes and healthcare reference groups (HRGs) listed in the Table 3.
- BPT prices will apply for procedures that group to the listed HRGs, whether they are recorded as outpatient or day case/elective. These prices are set by assessing British Association of Day Surgery (BADS) target ratios for outpatient/day case and calculating an equalised price for day case, elective and outpatient settings. The prices are set out in Annex A.
Table 3: RPRP procedures and HRGs
|
HRG |
OPCS |
Description |
|
JC43C: Minor skin procedures |
S081 |
Curettage and cauterisation of lesion of skin of head or neck |
|
S083 |
Curettage of lesion of skin of head or neck NEC | |
|
S131 |
Punch biopsy of lesion of skin of head or neck | |
|
S132 |
Punch biopsy of lesion of skin NEC | |
|
S141 |
Shave biopsy of lesion of skin of head or neck | |
|
S142 |
Shave biopsy of lesion of skin NEC | |
|
S148 |
Other specified shave biopsy of skin | |
|
S149 |
Unspecified shave biopsy of skin | |
|
S151 |
Biopsy of lesion of skin of head or neck NEC | |
|
S152 |
Biopsy of lesion of skin NEC | |
|
S158 |
Other specified other biopsy of skin | |
|
S159 |
Unspecified other biopsy of skin | |
|
BZ86B: Intermediate Vitreous Retinal Procedures, 19 years and over, with CC Score 0-1 |
C794 |
Injection into vitreous body NEC |
|
HN45A: Minor hand procedures for non-trauma, 19 years and over |
A651 |
Carpal tunnel release |
|
LB77Z: Transperineal Template Biopsy of Prostate
|
M702 |
Perineal needle biopsy of prostate |
|
CA66A: Excision or Biopsy of Lesion of Mouth, 19 years and over |
F241 |
Biopsy of lesion of tongue |
|
F421 |
Biopsy of lesion of mouth NEC | |
|
MA23Z: Minimal Lower Genital Tract Procedures |
Q014 |
Large loop excision of transformation zone |
Operational
- SUS+ will automate payment of the BPT price for all eligible activity (i.e. the OPCS codes and linked HRGs set out in Table 3).
2. Endoscopy procedures
Purpose
- The aim of this BPT is to provide a financial incentive to promote improved and consistent standards across endoscopy services.
- Award of accreditation by the Joint Advisory Group on GI Endoscopy (JAG) provides assurance that an endoscopy service is delivering high-quality, safe and effective care for patients, as well as supporting the endoscopy workforce and providing a suitable training environment. Eligibility for accreditation requires satisfactory scores in the Global Rating Scale and is awarded after submission of written evidence and a site visit by a professional team of peer assessors.
Design and criteria
- The BPT applies to adults only for elective endoscopic procedures in all NHS providers (including community organisations) and independent sector providers. The BPT will apply at the HRG level to all relevant day-case, elective and outpatient procedure activity that has a unit price.
- For the BPT, JAG provides three levels of site accreditation, shown in Table 4 below.
Table 4: JAG accreditation levels
|
Level |
Description |
|
Level 1 |
Units have met the necessary standard for full JAG accreditation or the unit is undergoing a reaccreditation assessment |
|
Level 2 |
Units have been assessed as improvements required or are in a period of accreditation award deferral. However, they have provided evidence to JAG of progress in addressing issues and will be reassessed within a specified timeframe |
|
Level 3 |
Units have been assessed as not meeting the minimum standard, are not accredited, and units undergoing assessment (not currently accredited) or are not participating in the JAG accreditation scheme, |
- Only providers achieving level 1 accreditation will be reimbursed at the full BPT rate. Providers at level 2 will receive a price 2.5% below the BPT level and providers at level 3 will receive a price 5% below the BPT level.
- The status of providers is defined by JAG, available on its website, and updated monthly.
Operational
- Providers should agree the BPT price based on the JAG accredited centres across organisations. Where centres have had a change in accreditation throughout the year, there should be a shift in payment to reflect their new status.
- Information on the JAG website is at site rather than organisation level. Where a provider has sites of mixed status, commissioners must apply the BPT at site level where they are able to do so. Otherwise, organisations will need to agree the appropriate reduction that reflects the service provision across the provider. If agreement cannot be reached, we suggest that the fixed payment is reduced in proportion to the number of sites that are not engaged.
- Where providers do not attain level 1 accreditation, commissioner expenditure will reduce. We expect commissioners will engage with providers to improve services and adherence to JAG standards.
3. Pleural effusion
Purpose
- People with a pleural effusion will often present acutely to A&E services with breathlessness. A chest drain can be used to remove the blood, pus or fluid from the pleural cavity. It is a common procedure, but when not inserted properly the drain may puncture major organs such as heart, lungs, liver and spleen. Therefore, all patients, apart from those in extremis, should have such a drain placed under ultrasound control as specified by the British Thoracic Society (BTS) guidelines.
- Historically, many patients presenting at A&E with a pleural effusion were admitted to wait for drain placement by imaging departments. This unnecessarily increased length of stay and delayed the patient’s journey as the pleural effusion was not managed by a pleural disease expert.
- The aim of this BPT is to incentivise a shift in activity away from non-elective admissions to pleural effusions being performed on an elective basis under ultrasound control.
Design and criteria
- This is achieved by setting the price for elective admissions relatively higher than the non-elective price, creating a financial incentive for the management of patients on a day-case basis. In setting the BPT, we have assumed that 50% of current admissions to DZ16N are suitable for management on a day-case basis (either YD04Z or YD05Z). These figures are based on assessment using expert clinical opinion. The remaining admissions are unsuitable for day-case management because of complications or comorbidities.
- The BTS guidelines stipulate that pleural effusion should be performed using bedside ultrasound guidance when determining the best site for aspiration and/or biopsy.
- The BTS guidelines also recommend that pleural procedures should not be done out of hours except in an emergency. Complications of most surgical procedures are higher when performed after midnight. Most pleural procedures do not need to be performed as an emergency and therefore should not be carried out overnight except in the case of significant respiratory or cardiovascular compromise. In certain circumstances, a pleural aspiration of 500 to 1000 mL may be safer than a chest drain.
- The BPT applies only to adults with undiagnosed unilateral pleural effusions.
Operational
- The price for an elective day case applies at the HRG level. SUS+ will automate payment where the spell meets these criteria:
- patient aged 19 or older
- elective admission method (11, 12 or 13)
- HRG codes YD04Z and YD05Z.
- We anticipate that some patients will need to be admitted immediately to an acute medical unit to relieve breathlessness before being discharged with a booked day-case appointment. This approach will ensure we do not disqualify providers from receiving the BPT where they deliver care in line with the best practice criteria.
- As with other BPTs designed to incentivise a shift in activity between settings, this BPT is made up of a pair of prices that create a financial incentive, without costing commissioners more. This is achieved by:
- departing from the conventional pricing structure, with the price for the elective care setting higher than the non-elective price
- decreasing the absolute level of prices for both settings to reflect the lower cost of providing a greater proportion of care in the elective setting.
4. Primary hip and knee replacement outcomes
Purpose
- In 2017/19 we amended the outlier criteria requirement for the primary hip and knee replacement outcomes BPT.
- The purpose of the BPT is to link payment to the outcomes that are important to the patient. The aim is to reduce the unexplained variation between providers in the outcomes reported by patients.
Design and criteria
- The criteria are:
- the provider not having an average health gain significantly below the national average
- the provider adhering to the following data submission standards:
- a minimum patient reported outcome measures (PROMs) participation rate of 50%
- a minimum NJR compliance rate of 85%
- the NJR unknown consent rate below 15%.
- hip replacements for patients aged 70 or over:
- the provider uses cemented or hybrid prostheses for at least 80% of patients.
- The criteria were informed by the 2015 GIRFT national review of adult elective orthopaedic services in England.
- In relation to the last criteria, where orthopaedic units can use NJR data to demonstrate that the outcomes from this group of patients receiving uncemented hip replacements are better than the cemented or hybrid prostheses, commissioners and providers can agree a local variation to permit payment of the full BPT prices.
- By ‘better outcomes’, our expectation is that providers not achieving the target may receive the full BPT price if their three-year revision rate for uncemented prostheses for patients aged 70 or over is lower than the national three-year revision rate expected for this age group for cemented and hybrid prostheses nationally. We will look to provide further supporting guidance in-year if this is needed to assist implementation.
- Providers also will not receive the BPT if they are:
- below the lower 99.8% control limit based on the most recently published data
- below the lower 95% control limit based on the most recently published previous two years’ data.
- When the BPT was introduced in 2014/15, the minimum thresholds for data submissions were intentionally set lower than the ones providers should aspire to. This was intended to allow providers time to adopt mechanisms to improve submission rates. In response to this, in 2016/17 the thresholds for NJR compliance and consent were increased.
- The data necessary to measure adherence to the payment criteria, along with further information relating to both collections, are available from:
- PROMs https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/patient-reported-outcome-measures-proms
- NJR njrcentre.org.uk/njrcentre/default.aspx
Operational
- SUS+ will automate payment of the BPT price for all eligible activity.
- Commissioners will need to monitor PROMs and NJR publications to determine whether providers are complying with the payment criteria. Where this is not the case, commissioners should manually recover to the base (non-best practice) price until an improvement is shown in the published data and the BPT requirements are met.
- The aim of the BPT is to improve patient outcomes and it should not be seen as a way for commissioners to reduce funding. Therefore, before adjusting payment, it is expected commissioners will discuss the data with providers and support any action to improve outcomes.
Patient reported outcome measures (PROMs)
- PROMs assess the quality of care delivered to NHS patients from the patient perspective. Information is collected about a patient’s health status (or health-related quality of life) before surgery and again six months after the procedure, with any change in health state attributed to the intervention. For this BPT, changes in health state are assessed using the casemix-adjusted condition-specific Oxford Hip Score and Oxford Knee Score for primary joint replacements only.
- Providers’ average health gain is presented as a funnel plot and compared with the national average of all providers in England (see Figure 1). The funnel plot indicates whether a provider’s health gain is statistically significantly different from the national average. According to the PROMs publication, providers are outliers if they are:
- below the lower 95% significance level labelled ‘alerts’
- below the 99.8% significance level labelled ‘alarms’.
Figure 1: Example of PROMs provider score comparison
(adapted from the provider score comparison tool)
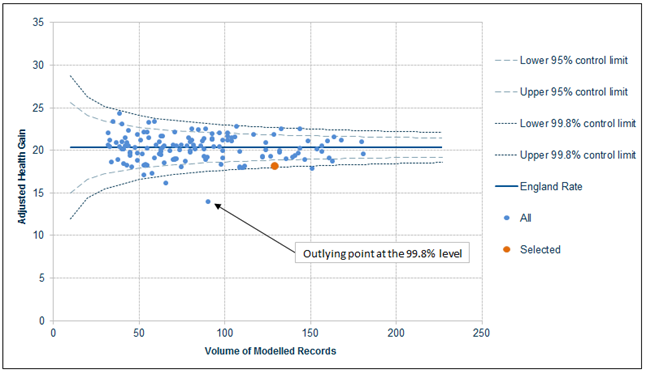
- Whether identified as an outlier or not, all providers should work to achieve the best possible outcomes. Outliers are identified relative to the national average, which may change as the data is updated throughout the year.
- To make the comparisons between providers’ outcomes meaningful, a procedure-specific casemix adjustment is applied to the PROMs data before inclusion in the funnel plot. These specific adjustments are based on statistical models that predict expected outcomes based on patient characteristics and other factors beyond providers’ control. This allows more accurate comparisons between the average outcomes achieved by different providers. It also means that providers cannot improve their relative position by selecting patients of a particular type as it is the difference between actual and expected health gain that matters, not simply the absolute health gain.
- Further information on the casemix adjustment methodology is published by NHS England.
- The method of identifying outliers only works when providers have a minimum of 30 completed questionnaires. When this is not the case, payment of the BPT is based on providers meeting the data submission requirements of best practice.
- The first of these is that providers achieve a minimum PROMs participation rate. This rate is calculated as the number of preoperative PROMs questionnaires completed, relative to the number of eligible HES spells.
- The PROMs publication also reports other outcome and data submission statistics for primary hip and knee replacements, including EQ5D Index, EQ5D VAS and linkage, issue and response rates. While not a condition of this BPT, these may be considered as evidence of good practice.
- PROMs data are updated on a cumulative basis, meaning the data becomes more complete over the year. Because the postoperative questionnaire is not sent out until six months after surgery, compliance with the BPT will need to be assessed against the latest available data at the time of payment. Organisation-level data are made available each quarter (typically in February, May, August and November). Data is provisional until a final annual publication is released each year, but for the BPT the provisional data should be used.
- In some instances, the latest participation figures will relate to a different period from the outcome measure, as postoperative questionnaires are not sent out until six months after surgery and so are subject to a greater delay. Published outcomes will also be subject to a lag while questionnaires are completed, returned and processed.
National Joint Registry
- In addition to PROMs outcome and participation, payment of this BPT is conditional on data submitted to NJR.
- NJR is part of the National Clinical Audits and Patient Outcomes Programme. It aims to improve patient care by collecting information about joint replacement prostheses and surgical techniques to provide an early warning of issues related to patient safety. Providers are required to upload information to the registry after joint replacement, which NJR uses to support quality improvements and best practice through its monitoring and reporting of the outcomes achieved by different prostheses, surgeons and providers. Data published in the NJR annual report also supports choice and policy decisions.
- Payment of the BPT is conditional on providers meeting minimum thresholds regarding two aspects of the NJR data:
- compliance – measured as procedures uploaded relative to the number of eligible spells recorded in HES
- consent – measured as the proportion of uploaded procedures for which patient consent was not requested or is unknown.
- As with the PROMs data, there is a short lag between procedures and data being made available through NJR publications. Therefore, commissioners should base compliance on the latest available data at the time of payment.
- Although independent sector providers do submit data to NJR, it has no way of cross-checking compliance as it has no comparator for private (non-NHS) activity – unlike for NHS providers, where NJR can check against HES. This is an area NJR is working on. However, until there is a solution, this criterion would not apply for the purposes of the BPT. You should continue to seek assurance from the provider that it is submitting relevant information to NJR.
Data quality
- Participation in the data collections is included to improve the data quality and the accuracy with which outcomes are reported. PROMs participation rates may be improved by distributing the preoperative questionnaires in a structured and organised way. Integrating the process into the general preoperative assessment routine is a good way to help ensure high coverage. Providers may also work with their individual supplier who delivers and collects the questionnaires to find a solution that meets their individual needs.
- PROMs participation rates for a few providers may be greater than 100%. This occurs where the number of PROMs questionnaires returned exceeds the activity recorded in HES. This can occur for a number of reasons: for example, where a provider administers the PROMs questionnaire but the procedure is either carried out at another provider due to subcontracting arrangements, or the procedure is not carried out at all due to unforeseen circumstances. Where this causes issues with assessing adherence to the best practice characteristics, providers and commissioners should reach local agreement on whether thresholds are met.
- While not a condition of this BPT, providers can do some things to improve the accuracy of their reported rates:
- Some providers choose to administer the preoperative PROMs questionnaire at a preassessment clinic before admission. This means that questionnaires may be received for cancelled operations for which there is no episode in HES. Administering questionnaires closer to or actually on the day of admission may reduce the chances of this happening.
- Clinical coding problems could mean that questionnaires cannot be linked to HES because of poor or incomplete clinical coding. Ensuring that all procedures are fully coded would help this.
- NJR compliance rates reflect the extent to which eligible hip and knee joint replacement procedures recorded in HES correspond to a record in NJR. These compliance rates may be reported as greater than 100% when the number of records uploaded to the NJR exceeds a provider’s activity recorded in HES. This may reflect inaccuracies in the coding of HES data or where activity is subcontracted to another provider, so that HES reports activity at the primary provider but the corresponding NJR record is recorded against the subcontracted provider.
- To improve NJR compliance, a provider must ensure that both NJR and HES data accurately reflect joint replacement activity undertaken within and on behalf of the organisation. Providers should work with their local NJR regional co-ordinator to address any issues in NJR compliance.
Improving outcomes
- Many factors affect patient outcomes, and the way in which improvements are achieved is for local determination. However, the following suggestions may be useful in supporting discussions between providers and commissioners when planning improvements.
- The headline PROMs scores can be broken into individual domain scores, and providers can request access to their own individual patient scores through NHS England. Providers might look at which questions they perform badly on to identify why they have been identified as an outlier.
- Individual patient outcomes may also be compared against patient records to check for complications in surgery or comorbidities that may not be accounted for in the casemix adjustment. It would also be sensible to check whether patients attended rehabilitation sessions once discharged from hospital.
- Reviewing the surgical techniques and prosthesis used against clinical guidelines and NJR best practice recommendations is another way in which providers may attempt to address poor outcomes. As well as the surgical procedure itself, outcomes can be improved by scrutinising the whole of the care pathway to ensure no other area is affecting outcomes.
- Providers may also choose to work collaboratively with those identified as having outcomes significantly above average, to learn from service design at other organisations. Alternatively, providers could conduct a clinical audit, a quality improvement process that seeks to improve patient care and outcomes through a systemic review of care against expected criteria.
Further considerations
- In some circumstances, providers may be unable to demonstrate that they meet all the criteria for the primary hip and knee replacement BPT, but it would be inappropriate for them not to receive the full BPT price. These are:
- when recent improvements in patient outcomes are not yet reflected in the nationally available data
- when providers have identified why they are an outlier on patient-reported outcome measures (PROMs) scores and have a credible improvement plan in place, the impact of which is not yet known
- when a provider has a particularly complex casemix that is not yet appropriately taken into account in the casemix adjustment in PROMs.
- Commissioners should pay the full BPT if a provider can show that any of these circumstances apply. The rationale for this is explained below.
Recent improvements
- Because of the lag between collecting and publishing data, recent improvements in patient outcomes may not show in the latest available data. In these circumstances, providers will need to provide other types of evidence to support a claim that their outcomes have improved since the published data was collected.
Planned improvements
- Where providers have identified shortcomings with their service and can show evidence of a credible improvement plan, commissioners must continue to pay the full BPT. This is necessary to mitigate the risk of deteriorating outcomes among providers not meeting the payment criteria.
- In this situation, the payment would be a time-limited agreement. Published data would need to show improvements for BPT-level payment to continue.
- There are many factors that may affect patient outcomes, and it is for local providers and commissioners to decide how to achieve improvements. However, these suggestions may be useful:
- Headline PROMs scores can be broken down into individual domain scores. If required, providers can also request access to individual patient scores through NHS England. Providers might look at the questions on which they score badly to see why they are an outlier: for example, those relating to pain management.
- Individual patient outcomes might also be compared with patient records to check for complications in surgery or comorbidities that may not be accounted for in the formal casemix adjustment. It would also be sensible to check whether patients attended rehabilitation sessions after being discharged from hospital.
- Reviewing the surgical techniques and prostheses used against clinical guidelines and National Joint Registry recommendations is another way providers might try to address poor outcomes. As well as improving the surgical procedure itself, providers could scrutinise the whole care pathway to improve patient outcomes by ensuring that weakness in another area is not affecting patient outcomes after surgery.
- Providers may also choose to collaborate with others that have outcomes significantly above average to learn from their service design. Alternatively, they might do a clinical audit. This is a quality improvement process that seeks to improve patient care and outcomes through a systemic review of care against expected criteria.
Casemix
- Providers that have a particularly complex casemix and cannot show they meet the best practice criteria may request that the commissioner pays the full BPT. Although the PROMs results are adjusted for casemix, a small number of providers may face an exceptionally complex casemix that is not fully or appropriately accounted for. These providers will therefore be identified as outliers in the PROMs publications. Commissioners are likely to be aware of such cases already and must agree to pay the full BPT. We anticipate that any such agreement will only be valid until the casemix adjustment in PROMs better reflects the complexity of the provider’s casemix.
5. Rapid colorectal diagnostic pathway
Purpose
- Straight-to-test (STT) pathways can improve access to testing, enabling earlier diagnosis and treatment, and improve patient outcomes. They involve clinical assessment and triage over the phone, before further investigation, rather than patients having to attend an outpatient appointment before their investigation is booked.
- Pathways differ from direct access services. Direct access to diagnostics is an arrangement where a GP managing a patient’s ongoing care can refer them directly to secondary care for a diagnostic test or procedure. The GP will use the results of the test to inform their decision-making around the patient’s continuing care. Direct referrals from primary care to diagnostic services in secondary care do not start a referral-to-treatment (RTT) clock, unless an escalation mechanism has been agreed locally.
- The Accelerate, Coordinate, Evaluate (ACE) Programme 2017 report found good evidence that STT pathways are more efficient in reducing diagnostic and treatment waiting times and result in improved patient and GP experience. The following key findings and implications have been recognised by the colorectal projects in developing their STT pathway approach:
- shortened diagnostic intervals
- outpatient appointment impact
- improving operational pathway management and quality
- improving patient and GP referral experience
- improving performance management.
Design and criteria
- The BPT payment will be conditional on delivering the rapid colorectal diagnostic pathway and based on an annual provider-level self-assessment.
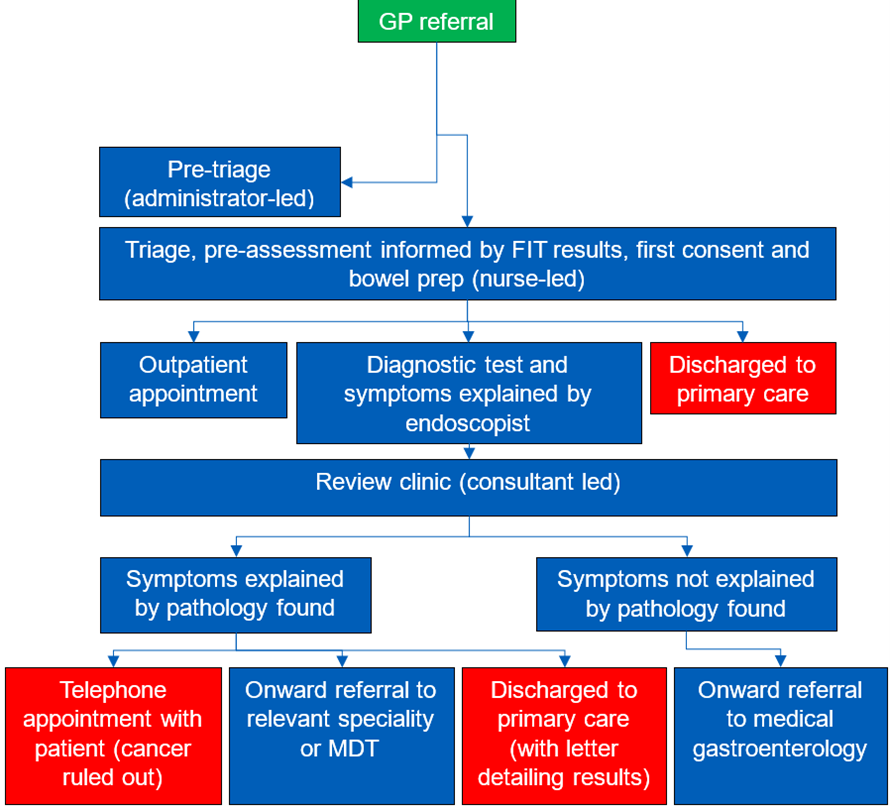
- The pathway should ideally include:
- an administrative assessment, in advance or combined with the ‘triage’ appointment, to maximise benefit of the appointment, confirm bloods have been taken, a FIT test result is available (and if not it should be ordered to inform next steps on the pathway) and to reduce missed appointments (did not attends – DNAs)
- support for patients through their pathway with (as far as possible) a single point of contact sending SMS/email appointment reminders. This may be delivered by pathway navigator roles or existing members of the care team, with the approach tailored to suit the pathway. The role may include co-ordination of appointments and providing information/ guidance about each part of the diagnostic process, as well as an overall timeline to patients and carers.
- The STT pathway offering diagnostic tests to patients without an initial outpatient appointment should follow this guidance:
- The GP refers the patient onto the two-week referral pathway or six-week diagnostic pathway.
- The provider contacts the patient via a triage process, aided by an algorithm, to decide the most appropriate test. It is important that a FIT result is included in this algorithm. It is recommended that primary care is responsible for completing the FIT test prior to referral and where the FIT test result is <10ug/gm and there are no concerning symptoms, the patient is not referred (other than for patients with an anal/rectal mass or anal ulceration which are exemptions for FIT testing). Wherever a referral is made, the FIT result should be included on the referral form. This is in line with BSG/ ACPGBI guidance.
- If the approach is not suitable for the patient, the triage hub would discuss this with the patient and book a referral for an outpatient appointment.
- The STT pathway should end with either:
- telephone appointment with the patient to inform them they are no longer being investigated for potential cancer (for example if the FIT result is negative (<10) and no other concerning symptoms have been identified
- onward referral to medical gastroenterology
- onward referral to other relevant speciality or MDT
- discharge back to GP care (with letter detailing what has been found and what, if any, management needs to be planned).
- An example, BPT-compliant, STT pathway is set out in Figure 2.
Figure 2: Example STT pathway
- The self-assessment should be based on achieving all the following characteristics:
- STT-dedicated nurses in post – nursing team, minimum of two at band 6 (competent to consent and book diagnostics) or band 7 who meet recommended competencies. They do not need to be two whole-time equivalents and should be combined with other appropriate roles.
- Evidence-based investigation algorithms in place, which include FIT, agreed by the consultant team.
- Evidence that the FIT result is being used to inform the onward pathway including removal of patients from the STT pathway where the patient has a FIT negative result (<10) and no further concerning symptoms.
- Evidence of primary care and patient group liaison with pathway development.
- Strong clinical leadership – the STT service needs to be led by a nominated consultant (colorectal surgeon/gastroenterologist/consultant nurse).
- Pathway supported by systems allowing active tracking of referrals and collection of outcome data.
- 28-day faster diagnosis standard
- Demonstrable reduction in outpatient clinic requirements for patients on the pathway.
- Availability to commissioners of outcome data from the pathway.
- Plans in place to ensure sufficient endoscopy capacity to deliver pathway.
- Development of an STT standard operating procedure.
- The ‘triage’ element of the pathway should be a single appointment which:
- combines triage and preassessment
- includes assessment of fitness and arrangements for bowel prep
- is virtual (such as on the telephone or video call) but with direct patient discussion
- undertakes first stage consent
- ensures sufficient time is allocated in job plan
- uses FIT to help determine next steps for the patient
- is supported by the nominated consultant and undertaken by either a band 6 nurse competent to consent and book mpMRI or a band 7 nurse
- documents the discussion including agreed outputs which are available to the wider clinical team.
- Consultant-led virtual review clinic (after diagnostic test) before endoscopic, radiological and histology results conveyed to GP and patient within 28 days and in an appropriate patient-centred fashion.
Operational
- For trusts to deliver an STT pathway, we recommend that providers and commissioners agree a payment structure reflecting the benefits of the pathway while taking into account any savings from a reduction in the delivery of outpatient services.
- In addition to the self-assessment, commissioners may request evidence to prove that providers have met the criteria set out above.
- Providers and commissioners should agree a local price, which providers receive for applicable activity based on locally agreed data flows and supporting information.
- If a provider can prove they have put procedures in place and have met the criteria part way through the year, they could be reassessed and the agreed local price paid from that point onwards.
6. Spinal surgery
Purpose
- In 2019/20 we introduced a BPT to improve the proportion of spinal surgery cases entered into the British Association of Spinal Surgeons (BASS) British Spine Registry (BSR).
- This BPT aims to support meaningful comparison and analysis of spinal surgery and help to reduce variation in the treatment and outcomes for patients.
- ‘Spinal surgery’ is used to describe a wide range of operations. In England, approximately 7,600 spinal procedures are done annually on a heterogeneous cohort of patients.
- As this BPT applies to both elective activity and non-elective, providers and commissioners will need to agree to incorporate the BPT payments into the fixed payment for non-elective activity, but continue to operate the BPT on a quarterly basis on actual volumes of activity delivered for elective services.
Design and criteria
- For the relevant list of HRGs that fall within the scope of the BPT, as described in Annex A, there are two prices: a base price and a BPT conditional top-up payment. The base price is set at 90% of the BPT price.
- To qualify for the BPT, the provider must achieve a 50% case ascertainment rate for applicable procedures recorded in the BSR. The intent is to increase the case ascertainment rate to 80% and over in future years.
Operational
- The BPT price is made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price is payable for all activity irrespective of whether the provider has met best practice characteristics. For elective activity, the BPT conditional top-up price is payable only if the provider meets the 50% case ascertainment rate.
- The BPT conditional top-up payment applies at the HRG level for all relevant admissions. The base price is generated by the grouper and SUS+, where the spell meets these criteria:
- all admissions (including day case)
- HRG from the list in Annex A.
- Where satisfied that providers have achieved the best practice criteria, commissioners should manually adjust the base price by applying the BPT conditional top-up payment.
- Provider compliance data will be available within Arden & GEM CSU’s GEMIMA and NCDR data portals, which will produce a report quarterly showing the provider-level achievement against the BPT criteria. This will be available to both commissioners and providers. Commissioners should use the data portals to measure whether providers have achieved the BPT for each quarter. To enable accurate reporting and payment, providers should ensure their data is submitted to BSR in a timely manner and at least within four weeks of the end of the quarter. Please note: quarters will not be updated after the four-week period ends (ie when Q2 is reported, Q1 will not be updated).
- Achievement is measured at provider, not patient, level. Reports at provider level will be published on a quarterly basis. Achievement will thus be measured within each quarterly reporting period, via the quarterly reports. Therefore, providers that achieve the BPT are eligible to receive the BPT from every commissioner that has a patient admitted (for the listed HRGs in Annex A) during the reporting period. Providers that do not achieve the criteria will not be eligible for the BPT conditional top-up and will only be able to claim the base price for all activity within the period.
Annual BPTs
- Acute stoke care (Section 7)
- Adult renal dialysis (Section 8)
- Adult asthma – aged 19 and over (Section 9)
- Chronic obstructive pulmonary disease (Section 10)
- Diabetic ketoacidosis or hypoglycaemia (Section 11)
- Early inflammatory arthritis (Section 12)
- Emergency laparotomy (Section 13)
- Fragility hip and femur fracture (Section 14)
- Heart failure (Section 15)
- Major trauma (Section 16)
- Non-ST segment elevation myocardial infarction (Section 17)
- Paediatric diabetes (Section 18)
- Paediatric epilepsy (Section 19)
- Parkinson’s disease (Section 20)
- Referral of appropriate post-myocardial infarction (STEMI) patients to cardiac rehabilitation (Section 21)
7. Acute stroke care
Purpose
- Patients presenting with symptoms of stroke need to be assessed rapidly and treated in an acute stroke unit by a multidisciplinary clinical team. The team will fully assess, manage and respond to complex care needs, including planning and delivering rehabilitation from the moment the patient enters hospital to maximise their potential for recovery. The acute stroke care BPT is designed to generate improvements in clinical quality in the acute part of the patient pathway. It does so by incentivising key components of clinical practice set out in the National Stroke Strategy, National Institute for Health and Care Excellence (NICE) clinical guideline CG68 Stroke and transient ischaemic attack in over 16s: diagnosis and initial management, the NICE quality standard for stroke QS2 and the NICE technology appraisal TA990.
Design and criteria of the BPT
- The Royal College of Physicians has published a national clinical guideline for stroke. Recommendation 3.4.1b of its stroke guidance (fifth edition, 2016) states: “Patients with suspected acute stroke should receive brain imaging urgently and at most within 1 hour of arrival at hospital.” This supports the changes made to the Level 2 criteria for 2020/21.
- In 2019/20 we clarified the reporting requirements for the criteria of patients who must be seen by a consultant with stroke specialist skills within 14 hours of admission, setting out how this is reported in the Sentinel Stroke National Audit Programme (SSNAP).
- This design provides additional funding per patient to meet the anticipated costs of delivering best practice and creates an incentive for providers to deliver best practice care.
- In 2020/21 we amended the Level 2 criteria so that it is aligned with the urgent care standards being trialled.
- In 2025/26 we amended the level 3 criteria so that it is aligned with the updated NICE recommendation to use the least expensive option of the available treatments (including tenecteplase and alteplase).
- The BPT is made up of three conditional payment levels:
- Level 1: Patients admitted directly (defined as within four hours of arrival in hospital) to an acute stroke unit, or similar facility where the patient can expect to receive the service described in quality marker 9 of the National Stroke Strategy, either by the ambulance service, from A&E or via brain imaging; they must not be admitted directly to a medical assessment unit. Patients must be assessed by a consultant with stroke specialist skills, at the bedside, by telemedicine or by telephone with access to picture archiving and communication system (PACS) imaging within 14 hours of admission. As SSNAP only measures the time of first admission to a stroke unit, not the time of admission to hospital, for the purposes of the BPT we define ‘admission to hospital’ for stroke patients as ‘clock start’. The patients must then spend most of their stay in the acute stroke unit. (‘Most’ is defined as greater than or equal to 90% of the patient’s stay within the spell grouping to HRGs AA35A, AA35B, AA35C, AA35D, AA35E, AA35F).
- Level 2: Both initial brain imaging and assessment by a stroke specialist (ie stroke specialist doctors, nurses and physician associates at trust Medical Director discretion) takes place within one hour of patient arrival at hospital (including A&E period of care). Initial imaging and assessment could be undertaken by telemedicine or telephone, but we would expect it to be limited to groups such as experienced registrars close to gaining consultant status or experienced stroke nurse consultants. If, within one hour of arrival at hospital, an assessment is undertaken by a consultant with stroke specialist skills at the bedside, by telemedicine or telephone then this will also meet the assessment element of Level 1. For the purposes of the BPT, reporting times are not defined but access to skilled radiological and clinical interpretation must be available 24 hours a day, seven days a week to provide timely reporting of brain imaging.
- Level 3: Patients are assessed for thrombolysis, receiving alteplase or tenecteplase if clinically indicated in accordance with the NICE technology appraisals TA264 (alteplase) and TA990 (tenecteplase). The additional payment covers the cost of the drugs, the additional cost of nurse input and the cost of the follow-on brain scan.
Operational
- The base price is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 19 or over (on admission)
- non-elective admission
- HRG from the list in Annex A.
- Of the three best practice payment levels, SUS+ will only apply the price for alteplase or tenecteplase when OPCS-4 code X833 (fibrinolytic drugs) is coded to create an unbundled HRG XD07Z (fibrinolytic drugs band 1) from AA35A to AA35F. For the other two best practice payment levels, organisations will need to agree local reporting and payment processes. Providers that meet all three BPT levels via local datasets will need to provide assurance to commissioners that they are not coding to OPCS-4 code X833 as well and receive payment twice. There are a variety of approaches being used locally to support reimbursement for the use of alteplase or tenecteplase.
- SSNAP is the single source of stroke data nationally. It is a useful source of information and support for organisations in establishing these processes, including validation of BPT achievement. Contribution to national clinical audits should be considered a characteristic of best practice for providers of high quality stroke care, although it is not a criterion for the BPT.
- Commissioners will be aware of different models for delivering high quality stroke care. While a few hyperacute units have been identified to admit all acute stroke patients, other units will provide high quality stroke care but not qualify for the element of the BPT relating to timely scanning (nor the additional payment for thrombolysis) because they admit patients who are further along the stroke care pathway. However, all acute providers of stroke care should be able to meet the requirement of direct admission to a stroke unit and so qualify for the corresponding incentive payment.
- One BPT scenario is that patients are admitted directly to an acute stroke unit either by the ambulance service, from A&E or via brain imaging. To qualify, acute stroke units must meet all the markers of a quality service set out in the National Stroke Strategy quality marker 9. These markers are that:
- all stroke patients have prompt access to an acute stroke unit and spend most of their time in hospital in a stroke unit with high quality specialist care
- hyperacute stroke services provide, as a minimum, 24-hour access to brain imaging, expert interpretation and the opinion of a consultant stroke specialist, and thrombolysis is given to those who can benefit
- specialist neuro-intensivist care, including interventional neuroradiology or neurosurgery expertise, is rapidly available
- specialist nursing is available for monitoring patients
- appropriately qualified clinicians are available to address respiratory, swallowing, dietary and communication issues.
- Where a patient has been assessed in A&E and identified as suitable for mechanical thrombectomy treatment, they should be transferred without delay to a specialist centre for treatment. Where the specialist centre for mechanical thrombectomy is separate from the A&E department the patient was first seen, transfer will not trigger an AA35* HRG and so the spell of care will not be eligible for a BPT. Commissioners should ensure the A&E provider is properly funded as part of their fixed payment for the scan and alteplase or tenecteplase element of the pathway.
8. Adult renal dialysis
- This BPT covers haemodialysis, home haemodialysis and dialysis away from base only. However, for completeness Table 5 shows all the currencies for adult renal dialysis. The BPT only applies to adult patients with chronic kidney disease and not those with acute kidney injury (principally because acute renal failure is excluded from the scope of the National Renal Dataset for detailed data collection). For payment purposes, organisations should distinguish patients starting renal replacement therapy on chronic and acute dialysis on the basis of clinical judgement in the same way that they do for returns to the UK Renal Registry.
Table 5: Adult renal dialysis currencies
|
Dialysis modality and setting |
Basis of payment |
|
Haemodialysis |
Per session |
|
Home haemodialysis |
Per week |
|
Peritoneal dialysis and assisted automated peritoneal dialysis (aAPD) |
Per day |
|
Dialysis away from base |
Per session |
- Contribution to national clinical audits should be considered a characteristic of good practice for providers of high quality renal dialysis care, though it is not a BPT criterion.
Haemodialysis
- The aim of the BPT for haemodialysis is to encourage the adoption of clinical best practice for vascular access where there is clear clinical consensus, as described in these guidelines and standards:
- Renal Association guidelines – Vascular access for haemodialysis
- Vascular Society and Renal Association joint guidelines
- National Service Framework (NSF) for renal services (standard 3).
- The ideal form of vascular access should be safe and efficient and provide effective therapy. A native arteriovenous fistula is widely regarded as the optimal form of vascular access for patients undergoing haemodialysis. The presence of a mature arteriovenous fistula at the time of first haemodialysis reduces patient stress and minimises the risk of morbidity associated with temporary vascular access placement as well as the risk of infection.
- If an arteriovenous fistula cannot be fashioned, an acceptable alternative form of definitive access is an arteriovenous graft which involves surgically joining an artery and vein using an artificial graft, usually polytetrafluoroethylene.
- The advantages of a native arteriovenous fistula over other forms of access which risk infection and thrombotic complications are significant. Dialysis via a fistula will also provide the option of higher blood flows during the procedure, resulting in more efficient dialysis.
- The Renal Association guidelines state an audit standard of 85% of patients on haemodialysis receiving dialysis via a functioning arteriovenous fistula. The BPT is based on providers achieving a rate of 80%, although providers should continue to work towards the 85% rate.
- The BPT requires vascular access to be gained via a functioning arteriovenous fistula. Therefore, renal units will need to collaborate with surgical services to establish processes that facilitate timely referral for vascular access.
Home haemodialysis
- The aim of unit prices for home haemodialysis is to make home haemodialysis a real choice for patients. The BPT price and structure include incentives for both providers and commissioners to offer home haemodialysis to all patients who are suitable.
- The BPT price for home haemodialysis reflects a week of dialysis, irrespective of the number of dialysis sessions prescribed. Providers and commissioners should have sensible auditing arrangements to ensure that home haemodialysis is at least as effective as that provided in hospital.
- It is expected that the BPT price will cover the direct costs of dialysis as well as the associated set-up, removal and utility costs incurred by the provider (eg preparation of patients’ homes, equipment and training).
Dialysis away from base
- A review of funding for dialysis away from base found that there may be associated additional costs. However, because the reference costs include these additional costs, the BPT price should adequately fund, on average, providers dialysing a mix of regular and away-from-base patients. Nevertheless, in recognition of the importance to patients of being able to dialyse away from base, and given that some providers will have a significantly disproportionate mix of patients, local arrangements should be made to ensure provider API fixed payments are appropriate. These may be agreed as follows:
- For all patients who require haemodialysis away from base, providers may be paid the arteriovenous fistula or graft BPT price (applicable HRGs: LD05A, LD06A, LD07A and LD08A), with the local arrangements then providing for any additional payments.
- Commissioners have the flexibility to recognise the costs to providers who face significantly high proportions of patients who require dialysis away from base. The appropriate additional level of reimbursement and the proportion of dialysis away from base are for local agreement between commissioners and providers. As a guide, we would expect that a significant proportion of dialysis away from base is around 85% to 90% of a provider’s total activity.
Operational
- The unit prices in this document apply at HRG level. The HRGs and prices are set out in Annex A. Commissioners will validate this via local data flows.
- Patients with chronic kidney disease attending solely for a dialysis session are not required to be submitted as part of the admitted patient care or outpatient commissioning dataset (CDS) (in line with the processing adjustment) because the activity data is recorded in the National Renal Dataset (NRD) and reported locally. For patients attending solely for a dialysis session, any activity submitted to the CDS should not be used for payment purposes. Any activity submitted to SUS+ should derive LA97A (Same day dialysis admission or attendance, 19 years and over) and will generate a zero price.
- The HRGs are generated from data items in the NRD. Commissioners must include, as a minimum, the data items listed in Table 6 in information schedules of NHS contracts where these services are provided.
Table 6: National Renal Dataset fields
|
Area |
Field |
|
Renal care
| [1] renal treatment modality, eg haemodialysis, peritoneal dialysis [6] renal treatment supervision code, eg home, hospital |
|
Person observation | [75] blood test HBV surface antigen [77] blood test HCV antibody[79] blood test HIV Demographics[19] PCT organisation code (Commissioner code should now be recorded here) |
|
Dialysis
| [182] type of dialysis access, eg fistula [23] dialysis times per week |
|
Organisations will also need to derive:
| · a unique patient identifier · patient age (in years derived from date of session – date of birth) |
- The reporting process for renal dialysis will differ from other services. The data items defined in the NRD are not contained in the CDS and do not flow into SUS+. We therefore expect organisations to implement local reporting while we continue to work towards a national solution. The local payment grouper will support local processes in generating HRGs from the relevant data items extracted from local systems.
- The HRGs in sub-chapter LD are core HRGs.
- Reporting and reimbursement for acute kidney injury will need to be agreed locally as part of API fixed elements. Annex B of the 2025/26 NHSPS details the currencies for haemodialysis for acute kidney injury.
- If a patient with acute kidney injury requires dialysis while in hospital during an unrelated spell, the dialysis price is payable in addition to the price for the core spell.
- Due to the variation in funding and prescription practices across the country, the BPT price for renal dialysis is not for funding the following drugs:
- erythropoiesis-stimulating agents: darbepoetin alfa, epoetin alfa, beta (including methoxy polyethylene glycol-epoetin beta), theta and zeta
- drugs for mineral bone disorders: cinacalcet, sevelamer, lanthanum paracalcitol and sucroferric oxyhydroxide.
- Organisations should continue with current funding arrangements for these drugs when used in renal dialysis or outpatient attendances in nephrology (TFC 361). For all other uses, the relevant BPT prices reimburse the associated costs of the drugs.
- Patients with iron deficiency anaemia of chronic kidney disease will require iron supplementation. For patients on haemodialysis, the prices cover the costs of intravenous iron. For patients, either on peritoneal dialysis or otherwise, the costs will be reimbursed through the appropriate unit price, either in outpatients or admitted patient care, depending on the type of drug and method of administration (slow infusion or intravenous).
9. Adult asthma – aged 19 and over
Purpose
- Asthma is a disease characterised by recurrent attacks of breathlessness and wheezing, which vary in severity and frequency from person to person. In an individual, they may occur from hour to hour and day to day. This condition is due to inflammation of the air passages in the lungs and affects the sensitivity of the nerve endings in the airways so they become easily irritated. In an attack, the lining of the passages swell, causing the airways to narrow and reducing the flow of air in and out of the lungs.
- We have introduced the adult asthma BPT to improve the proportion of patients who receive specialist review of their care within 24 hours of emergency admission for asthma attack and who also receive a discharge bundle before leaving hospital. Respiratory specialist team members may be defined locally to include respiratory health professionals deemed competent at seeing and managing patients with acute asthma attacks.
- These staff members might include: respiratory consultant, respiratory trainee of ST3 or above, respiratory specialist nurse or asthma nurse.
- Specialist input has been shown to improve outcomes, as well as adherence to evidence-based care processes in managing adult asthma patients.
Design and criteria
- For the HRGs that fall in the scope of the BPT, as described in Annex A, there are two prices: a base price and a BPT price. The base price would be set at 90% of the BPT price.
- To qualify for the BPT, 50% of patients must receive specialist input within 24 hours of admission and a discharge bundle before discharge (that is, one patient needs to receive both care processes to achieve the criteria).
Operational
- The eligible HRGs for the BPT are made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price is payable for activity irrespective of meeting best practice characteristics.
- The BPT applies at the HRG level for all relevant non-elective admissions. The base price is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 19 or over (on admission)
- non-elective admissions
- HRG from the list in Annex A.
- Providers and commissioners should agree in advance whether they expect the BPT criteria to be achieved. They should then reflect the relevant BPT price uplift in their API fixed element.
- Compliance with the BPT criteria would be measured by the National Respiratory Audit Programme’s (NRAP) secondary care audit. The national audit maintains live charts which show the provider-level achievement against the BPT criteria, which will be available to both commissioners and providers. In agreeing payments, providers and commissioners must have regard to latest performance data noting inherent short-term variation in delivery.
- For the purposes of measuring compliance with the BPT, patients with a date of death recorded in the audit will be excluded. The definitions of ‘specialist review’ and ‘discharge bundle’ are the same as those used by the NRAP secondary care audit:
- Specialty review within 24hrs of admission – Respiratory team members, as agreed by the British Thoracic Society membership, may be defined locally to include respiratory health professionals deemed competent at seeing and managing patients with acute asthma attack. These staff members might include respiratory consultant, respiratory trainee of ST3 or above, respiratory specialist nurse/specific asthma nurse or physiotherapist.
- A discharge bundle is a group of evidence-based items that should be implemented/checked and verified on discharge from hospital. The adult asthma discharge bundle complies with the BTS asthma 4: asthma attack bundle 2024. The discharge bundle must include all the mandatory elements listed below:
- Medication review including:
- Maintenance medication reviewed and understood
- Adherence discussed
- Inhaler technique checked and optimised
- A personalised asthma action plan (PAAP) issued/reviewed
- Tobacco dependence advice, treatment and referral for current smokers
- A clinical review within 4 weeks of discharge.
- Medication review including:
- Evidence of the care bundle being delivered must be found in the case notes.
- While not currently a specified element of the discharge bundle, providers should review both preventer and reliever inhaler technique with consideration given to using the lowest environmental impact inhaler device.
10. Chronic obstructive pulmonary disease (COPD)
Purpose
- COPD is a long‑term respiratory condition characterised by airflow obstruction that is not fully reversible. People with COPD often have exacerbations, when there is rapid and sustained worsening of symptoms beyond their usual day‑to‑day variation.
- In 2017/19 we introduced the COPD BPT to improve the proportion of patients who receive specialist respiratory review within 24 hours of emergency admission for an exacerbation of COPD and who also receive a specified discharge bundle of evidence based interventions before leaving hospital.
- Specialist input has been shown to improve outcomes as well as the adherence to evidence-based care processes in managing COPD exacerbations. However, only 65% of people admitted to secondary care receive specialist input to their care within 24 hours of admission.
- Patients who receive discharge bundles are more likely to receive better care than those who do not receive discharge bundles. However, only 69% of providers report using discharge bundles.
Design and criteria
- For the relevant list of HRGs that fall in the scope of the BPT, as described in Annex A, there are two prices: a base price and a BPT price. The base price is set at 90% of the BPT price.
- To qualify for the BPT, 60% of patients must receive specialist input within 24 hours of admission and a discharge bundle before discharge (that is, one patient needs to receive both care processes to be a success against the criteria).
Operational
- The eligible HRGs for the BPT are made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price is payable for activity irrespective of meeting best practice characteristics.
- The BPT applies at the HRG level for all relevant non-elective admissions. The base price is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 19 or over (on admission)
- non-elective admissions
- HRG from the list in Annex A.
- Providers and commissioners should agree in advance whether they expect the BPT criteria to be achieved and to reflect the relevant BPT price uplift in their fixed element.
- Compliance with the BPT criteria is measured by the National Respiratory Audit Programme’s (NRAP) secondary care audit. The national audit maintains live run charts which show the provider-level achievement against the BPT criteria, which will be available to both commissioners and providers. In agreeing payments, providers and commissioners must have regard to latest performance data, noting inherent short-term variation in delivery.
- For the purposes of measuring compliance with the BPT, patients with a date of death recorded in the audit will be excluded. The definitions of ‘specialist review’ and ‘discharge bundle’ are the same as those used by the NRAP secondary care audit:
- Respiratory team members, as agreed by the British Thoracic Society membership, may be defined locally to include respiratory health professionals deemed competent at seeing and managing patients with acute exacerbation of COPD. These staff members might include respiratory consultant, respiratory trainee of ST3 or above, respiratory specialist nurse or physiotherapist, COPD nurse or qualified pharmacist.
- A discharge bundle is a group of evidence-based items that should be implemented/checked and verified on discharge from hospital. The discharge bundle must include all the following mandatory elements:
- Medication review including:
– Maintenance medication reviewed and understood
– Adherence discussed
– Inhaler technique checked and optimisted
- Provision of a a written or digital personalised self-management plan and where appropriate an emergency drug pack.
- Tobacco dependence advice, treatment and referral (where appropriate).
- Assessment of suitability for referral to pulmonary rehabilitation and referral where appropriate.
- Ensuring that appropriate follow up arrangements are in place prior to discharge.
- Evidence of the discharge bundle being delivered must be found in the case notes.
- While not currently a specified element of the discharge bundle, providers should review both preventer and reliever inhaler technique with consideration given to using the lowest environmental impact inhaler device.
11. Diabetic ketoacidosis or hypoglycaemia
Purpose
- Diabetic ketoacidosis remains a common and life-threatening complication of Type 1 diabetes. Errors in its management are not uncommon and are associated with significant morbidity and mortality. Admitting, treating and discharging patients with diabetic ketoacidosis or hypoglycaemia without involving a diabetes specialist team could compromise safe patient care.
- The aim of this BPT is to ensure the involvement of a diabetes specialist team and patient access to a structured education programme. The involvement of a diabetes specialist team shortens patient stay and improves safety; it should occur as soon as possible during the acute phase. The main benefit of a structured education programme is reduced admission rates.
- Specialists must also be involved in assessing the precipitating cause of diabetic ketoacidosis or hypoglycaemia, managing the condition, discharge and follow-up. This includes assessing the patient’s understanding of diabetes plus their attitudes and beliefs.
Design and criteria
- The BPT applies only to adults admitted as an emergency with diabetic ketoacidosis or hypoglycaemia. It is made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price is payable for all activity irrespective of whether it meets best practice. The BPT price is payable if the patient:
- is referred to the diabetes specialist team (DST) on admission, and seen within 24 hours by a DST member
- has an education review by a DST member before discharge
- is seen by a diabetologist or diabetic specialist nurse before discharge
- is discharged with a written care plan (which allows the person with diabetes to be actively involved in deciding, agreeing and taking responsibility for how their diabetes is managed) that is copied to their GP
- is offered access to structured education, with the first appointment scheduled to take place within three months of discharge.
- In some circumstances, not all elements of the education review by a DST member will apply (eg injection issues that would be irrelevant to people who are not taking insulin, such as those taking oral medication, and ketone monitoring that is only required for individuals with Type 1 diabetes). The review to include: usual glycaemic control; injection technique/blood glucose; monitoring/equipment/sites; discussion of sick day rules; assessment of the need for home ketone testing (blood or urinary) with education to enable this; and contact telephone numbers for the DST including out of hours.
- Access to structured education, and waiting lists for it, vary across the country. Structured education should be delivered in line with the Diabetes UK care recommendation, ‘Education of people with diabetes’. It is accepted that in some circumstances, structured education may not be appropriate for patients (for example, elderly people with dementia or living in care homes). Where this is the case, structured education can be excluded from the criteria.
- The BPT excludes reimbursement for the structured education so arrangements for this will need to be agreed locally. There is a treatment function code (TFC) for diabetic education services (TFC 920) against which organisations should record and cost activity.
- The evidence base and characteristics of best practice have been informed by and are in line with:
- NICE Diabetes in adults quality standard (2011); NICE clinical guideline
- NHS Institute for Innovation and Improvement’s Think Glucose Project; Diabetes UK and Joint British Diabetes Societies (JBDS) Inpatient Care Group guidance The management of diabetic ketoacidosis in adults
- Diabetes UK and JBDS Inpatient Care Group guidance The hospital management of hypoglycaemia in adults with diabetes mellitus.
Operational
- The BPT applies at the sub-HRG level (‘flag BP52’), and SUS+ will apply the base price to spells with a BPT flag only (the conventional price will otherwise be applied). SUS+ will not apply the conditional top-up payment, and compliance with the characteristics of best practice will need to be monitored and validated through local data flows. Where satisfied that providers have achieved the best practice criteria, commissioners should make manual adjustments to the base price by applying the conditional top-up payment.
- The BPT flag is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 19 or over (on admission)
- emergency admission method (codes 21–25, 2A, 2B, 2C, 2D [or 28 if the provider has not implemented CDS 6.2])
- a diagnosis from the list in Annex A
- one of the HRGs from the list in Annex A.
- Where providers are not expecting to meet best practice, commissioner expenditure will reduce as the base price is set below cost. We expect commissioners will engage with providers to improve services in order to meet best practice in future years. Where providers and commissioners have agreed an improvement plan, they may reflect best practice in their API fixed element.
- The base price is set at 85% of the conventional HRG price, with the conditional component equal to the remaining 15%.
12. Early inflammatory arthritis
Purpose
- The BPT’s aim is to ensure timely diagnosis and, where appropriate, start of therapy of patients with early inflammatory arthritis. The BPT has been developed with the British Society for Rheumatology and Arthritis Research UK and reflects NICE guideline NG100: Rheumatoid arthritis in adults: management and NICE quality standard 33.
- The Rheumatoid and Early Inflammatory Arthritis 2nd Annual Report 2016 highlights the ongoing variation in care across England and Wales.
- In 2019/20 we updated the BPT to link achievement to six standards of care reported through the national clinical audit for rheumatoid and early inflammatory arthritis. In 2025/26 this was reduced to five standards of care, in line with a change to the NICE guidelines to focus on timely initiation of treatment. For patients who receive care as set out in the BPT, the provider will be eligible for a single conditional top-up payment per patient.
Design and criteria
- The BPT applies only when care meets all five standards in Table 7 and applies to the first three months of care for newly referred patients.
Table 7: Early inflammatory arthritis BPT: six standards of care
|
BPT criteria | ||
|
1 |
Audit |
The patient must be enrolled in the audit within 3 weeks of diagnosis |
|
2 |
Drug therapy |
The patient must start disease-modifying antirheumatic drugs (DMARDs) within six weeks of referral |
|
3 |
Education |
The patient must be offered disease education within one month of diagnosis |
|
4 |
Disease outcomes |
The patient must have a documented disease activity score (DAS) by three months. This should be documented in the audit. |
|
5 |
Disease outcomes | The patient must have a documented patient reported outcome (PRO) by three months. This should be documented in the audit. |
|
Data upload to the national clinical audit must take place within four weeks of the specific time point for each criterion. | ||
- For patients with inflammatory arthritis, a decision to start DMARD therapy should almost always be possible within six weeks of GP referral where inflammatory synovitis is sustained at specialist review.
- Current classification criteria for early inflammatory arthritis do not specify a minimum duration of disease but do assign a single point (out of 10 possible) for duration of six weeks or more. The hypothetical case of a patient presenting to their GP on their first day of symptoms and being referred the same day would be quite exceptional given the insidious onset of symptoms. Even in that situation, there would be six weeks of joint inflammation by the time DMARD initiation is suggested.
- There are substantial proven benefits of DMARD initiation within 12 weeks of symptom onset. To enable this, GPs should continue to develop and follow local guidance for referral to ensure that patients with suspected early inflammatory arthritis are referred within a maximum of six weeks of symptom onset.
- Given that urgent, intensive DMARD treatment might potentially transform outcomes for people with inflammatory arthritis by inducing remission and preventing disability, as well as reducing the need for subsequent biological therapies, Arthritis Research UK and the British Society for Rheumatology support this suggested six-week timeframe for specialist review and initiation of DMARD therapy.
Operational
- The BPT aims to provide an incentive for timely treatment and cover additional costs related to audit compliance for the first three months of care only.
- The BPT is a single conditional top-up payment payable for each newly referred patient who receives all five characteristics of best practice.
- Where satisfied that providers have achieved the best practice criteria, commissioners should apply the conditional top-up payment for each newly referred patient who received all five standards of care.
- Compliance with the BPT criteria will be measured by the national clinical audit for early inflammatory arthritis. The national audit will produce at least a quarterly report, showing commissioner- and provider-level achievement levels (number of patients). This will be available to both commissioners and providers. In agreeing payments, providers and commissioners must have regard to latest performance data as well as any expected changes for the upcoming year.
- SUS+ will not apply the conditional top-up.
- Providers will not be able to claim the conditional top-up for patients who do not receive all five standards of care.
13. Emergency laparotomy
Purpose
- ‘Emergency laparotomy’ and ‘emergency bowel surgery’ are terms used to describe a wide range of emergency operations on the bowel. These may be performed for a variety of conditions, including those arising from complications of elective (planned) surgery. In England alone, approximately 30,000 emergency laparotomies are undertaken annually on a heterogeneous cohort of patients. Overall, 30-day mortality has fallen from 11.8% in 2013/14 to 8.7% in 2019/20. However, emergency laparotomy surgery remains high risk when compared to elective surgery, and outcomes have continued to vary according to the type of surgery performed and the circumstances in which it is performed.
- This BPT aims to improve the proportion of high-risk patients who receive both:
- a formal risk assessment before a decision is made to undertake surgery
- input by peri-operative teams experienced in the management of older patients
- All patients should have an assessment of their individual risk of death to allow clinicians to tailor their care and meet their individual needs. Assessment of risk also informs shared decision making. This should be clearly documented as having been discussed with the patient in their notes, and also recorded on the consent form. Failure to formally assess risk may result in them not receiving the care that they should. Assessment of risk should be performed using objective risk calculation tools (ie the NELA risk calculator). However, objective risk scores should be used to support clinical decision making that also takes into account other factors such as patient frailty and other pathology that may not be accounted for when calculating an objective risk score.
- Older patients may suffer from multi-morbidity and may be frail. Frailty is defined as a syndrome of physiological decline in older people which makes them particularly vulnerable to adverse outcomes and deterioration in physical health after major stressors such as emergency laparotomy. NELA data and other studies (eg Frailty in older patients undergoing emergency laparotomy. Results from the UK observational Emergency Laparotomy and Frailty (ELF) study) demonstrate that frail patients are vulnerable to complications and an increase in mortality above that predicted by current risk scores. It is important to note, however, that while frailty incidence increases with age, it is not an inevitable part of the ageing process and can also occur in younger patients. Current guidelines and standards support the input of geriatricians and multidisciplinary perioperative teams to target the specific requirements of frail and elderly patients. From April 2023, NELA has been asked by NHSE to report on trust performance in providing input by peri-operative teams experienced in the management of older patients.
- The Third Seventh Patient Report of the National Emergency Laparotomy Audit (NELA) shows that 85% of patients had a formal assessment of their risk of surgery before surgery was undertaken, and that 27% of patients 80 or over, or 65 and frail had an assessment by a consultant geriatrician. Although NELA has previously collected data on the proportion of patients with geriatrician input, from April 2023, NELA will be collecting data on the proportion of patients 80 or over, or 65 and frail, who receive who input by peri-operative teams experienced in the management of older patients.
Design and criteria
- For the relevant list of HRGs that fall in the scope of the BPT, as described in Annex A, there are two prices: a base price and a BPT price. The base price is set at 90% of the BPT price.
- As a precondition of accessing the BPT, providers must have agreed trust-wide multidisciplinary pathways of care in place, as defined by the audit. These must be recorded in the audit as evidence of compliance. The pathways will need to have been agreed by key multidisciplinary stakeholders within the provider involved in delivering care. These include emergency departments, elderly care, radiology, surgery, anaesthesia and critical care. As a minimum, these pathways should cover a diagnostic pathway for the acute abdomen (before a decision for surgery has been made) and a laparotomy pathway (at the point surgery is needed).
- The existing metrics of maintaining consultant presence and critical care admission are still considered best practice, but BPT performance will now focus on:
- risk assessment: proportion of all patients who receive a documented assessment of risk as part of the decision to operate on the patient (as defined by the audit). Target – 85% of all patients.
- peri-operative team input: proportion of patients 80 or over, or 65 and frail, who receive input by peri-operative teams experienced in the management of older patients. Target – 40% of these patients.
- Although not a condition of the BPT, providers and commissioners should monitor case ascertainment to ensure that participation in the audit is sufficient for activity captured and reported by NELA to be an adequate reflection of provider activity. The NELA project team has developed an algorithm that extracts cases that meet the NELA inclusion criteria from Hospital Episode Statistics (HES). HES is comprised of patient data coded by the hospital’s own coding team. Historical case ascertainment is calculated by applying this case inclusion algorithm to HES data. Case ascertainment can be monitored via the NELA website.
Operational
- The BPT is made up of two components: a base price and a BPT price. The base price applies to all activity irrespective of meeting best practice characteristics.
- The BPT payment applies at the HRG level for all relevant non-elective admissions. The base price is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 19 or over (on admission)
- non-elective admission (including transfers)
- HRG from the list in Annex A.
- Providers and commissioners should agree the payment based on expected performance for the year. Following the change in metrics for the BPT, if a provider is not meeting the 40% peri-operative input target they can agree to not deduct funding for the BPT providing there is a plan to work towards this target.
- Compliance with the BPT criteria will be measured by the NELA. The national audit will produce at least a quarterly report, showing the provider-level achievement against the BPT criteria, which will be available to both commissioners and providers. This will include the BPT’s conditional element.
- For the purposes of measuring compliance with the BPT, the definitions of ‘risk assessment’ and ‘input by perioperative teams’ are the same as those used by NELA.
- NELA measures achievement at provider, not patient, level. Therefore, providers’ achievement of the BPT will apply to every commissioner that has a patient admitted (for the listed HRGs in Annex A).
- In the rare event a provider has no qualifying cases in the qualifying period, for the purposes of the BPT the audit will report activity at zero and compliance at 100%. This ensures that the provider will continue to receive the conditional top-up on the basis of making resources available.
- Annex A sets out the base price and BPT price funding levels, per patient, which best practice should attract. Providers and commissioners are asked to agree their fixed element based on an assessment of likely activity levels as agreed as part of wider system planning and whether the provider is likely to deliver best practice.
- Where best practice is not delivered when the funding is made available in the fixed payment, this should be discussed and a plan put in place, or funding adjustments made, in the next financial year/planning process. No in-year payment adjustments should be made.
14. Fragility hip and femur fracture
Purpose
- For patients with a fragility hip or femoral fractures, care needs to be quickly and carefully organised to prepare them for surgery. The most positive outcomes can be achieved by quickly stabilising patients and ensuring that expert clinical teams respond to their frail conditions and complex needs. Equally, the care that these patients receive following surgery is just as important, because it is in the initial days following surgery that the greatest gains can be made in patient outcomes.
- The aim of the BPT is to promote hip and femoral fracture programmes that provide best practice in the care and secondary prevention of fragility hip and femur fractures in line with the clinical guideline and quality standard from NICE (CG124 and QS16). For 2017/19 we removed three measures relating to the joint admissions protocol, multidisciplinary teamworking and post-op abbreviated mental test and replaced them with three new measures (items e, f and g in the list below).
Design and criteria
- The BPT is made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price is payable for activity irrespective of whether the characteristics of best practice are met. The BPT price is payable only if all these characteristics are achieved:
- time to surgery from arrival in an emergency department, or – if an admitted patient – time of diagnosis to the start of anaesthesia, is within 36 hours
- assessment by a geriatrician (defined as consultant, non-consultant career grade (NCCG) or specialist trainee ST3+) in the perioperative period (within 72 hours of admission)
- fracture prevention assessments (falls and bone health)
- an admissions assessment using the 4AT screening tool performed before surgery and the score recorded in National Hip Fracture Database (NHFD); it is expected that a reduced abbreviated mental test score of 7 or below would trigger a dementia risk assessment by dementia-trained staff, the outcome of which would inform appropriate discharge and follow-up arrangements
- a nutritional assessment during the admission
- a repeat delirium assessment using the 4AT screening tool during the admission
- assessed by a physiotherapist the day of or day following surgery.
- This design provides additional per patient funding to meet the anticipated costs of delivering best practice and creates an incentive for providers to deliver best practice care.
Operational
- The base price and the BPT price apply at the sub-HRG level (‘flag BP01’). The BPT flag is generated by the grouper and SUS+, where the spell meets these criteria:
- patient aged 60 or older (on admission)
- emergency, or transfer admission method (admission codes 21-25, 2A, 2B, 2C, 2D [or 28 if the provider has not implemented CDS 6.2] and 81)
- a diagnosis and procedure code (in any position) from the list in Annex A
- HRG from the list in Annex A.
- SUS+ will apply the base price to spells with the BPT flag.
- Commissioners determine compliance with best practice using reports compiled from data submitted by providers to the NHFD. The report is available quarterly in line with the SUS+ reporting timetable: for example, the report for the April to June quarter will be available at the final reconciliation date. Before the final reconciliation point, providers will be given two weeks from the end of the quarter to input and edit any outstanding records. NHS England will then match the records to responsible commissioners, which will take a further two weeks. Once the commissioner data is uploaded, providers will be given another two weeks to correct any problems or omissions. The final data will therefore be available to commissioners six weeks after the end of the quarter.
- Payments should not be adjusted in year, but performance against the BPT criteria should be discussed quarterly and feed into discussions on the level of the fixed element for the following year. We would not expect a provider who is not meeting best practice criteria to regularly attract funding equivalent to best practice.
- Providers already have access to the NHFD through a lead clinician who is responsible for ensuring the quality and integrity of the data.
- Commissioners may receive reports of NHFD data in one of two ways:
- commissioners nominate a data representative with an NHS email account to register to access the NHFD website; aggregated (anonymised) provider-level data will be provided in tabular, online reports
- NHS England, through its Data Services for Commissioners Regional Offices (DSCROs), will support the provision of data and analysis to underpin and provide evidence for best practice payments and validation with SUS+. The exact process should be negotiated locally.
- NHFD is currently the only source of data relevant to the BPT criteria collected on a regular basis, with professional clinical oversight. Further information on best practice is available from the NHFD website including advice on:
- improving clinical care and secondary prevention
- service organisation
- how to make a case for the posts and resources necessary for the delivery of high quality, cost-effective care.
- The pricing approach is designed to incentivise a change in practice and provide additional funding to adequately fund the costs of best practice.
Persistence with bone treatment after discharge
- We recommend that providers collect information on persistence with bone treatment after discharge.
- Many patients who have a hip or femoral fractures require some form of medication to reduce the risk of further fractures. Current practice should ensure that patients are assessed, and treatment started or recommended, in hospital, but it is well recognised that long-term compliance is poor and patients often do not take the tablets. Telephone follow-up is effective and significantly increases the rate of long-term compliance with treatment. It should be noted that the requirement depends on the follow-up taking place and not on patient compliance with medication. We suggest that telephone appointments take place 120 days from the date of discharge and that the data are recorded in the NHFD.
15. Heart failure
Purpose
- The aim of this BPT is to support best practice in the care of patients with heart failure, as outlined in: NICE clinical guideline NG106 Chronic heart failure in adults: diagnosis and management, clinical guideline CG187 Acute heart failure: diagnosis and management and quality standard QS9, chronic heart failure.
Design and criteria
- The payment of the BPT depends on providers meeting both these criteria:
- Data submission to the National Heart Failure Audit (NHFA) with a target rate of 70%. This means that at least 70% of all eligible records need to be submitted to NHFA.
- Specialist input with a target rate of 60%. This means that at least 60% of all patients recorded in the audit have received specialist input, as defined by NHFA.
- The BPT price is higher than the standard HRG price to reflect higher costs that providers may incur in achieving best practice.
Specialist input to the management of heart failure
- Management of heart failure by cardiology and heart failure specialists results in better outcomes for patients. Not only is mortality reduced in hospital and in the month following discharge, but the quality of care received in hospital benefits patients for some years following discharge, reducing subsequent admissions. (see HQIP 2015/16 national heart failure audit). Specialist input is also associated with patients receiving other evidence-based care processes.
- NHFA defines specialist input as a face-to-face review with a consultant cardiologist, or a consultant with a subspecialist interest in heart failure, or a specialist registrar or a heart failure nurse specialist. This is the definition on which success against the BPT will be judged alongside the data submission rate. For clarity, this should exclude non-specific categories (for example, ‘Other’ or ‘Unknown’). Providers should be able to show they have sufficient skill mix to provide specialist input for at least 60% of all non-elective heart failure admissions.
- The threshold for specialist input has been set relatively low to enable providers to make progress in meeting best practice in the early years of full national implementation. We anticipate that expectations of best practice will be revised upwards in future.
Submission of data to NHFA
- NHFA was established in 2007 to monitor the care and treatment of patients admitted to hospital in England and Wales with heart failure. It collects and reports data based on recommended clinical indicators and the outcomes of acute patients discharged from hospital with a primary diagnosis of heart failure. Further information can be found on the National Institute for Cardiovascular Outcomes Research (NICOR) website.
- Submitting data to NHFA will enable providers and commissioners to benchmark services, identify areas for improvement and monitor progress in improvements in the care of people with heart failure.
Operational
- The BPT applies at the HRG level for all relevant non-elective admissions.
- SUS+ will automatically assign the base price to in-scope activity. Using a guide developed by NICOR, providers will be required to submit a validation report to commissioners. Providers and commissioners should discuss expected BPT performance for the year as part of the planning process and factor best practice funding into their API fixed element.
- Meeting best practice criteria, and payment of the expected BPT achievement, should be based on the latest available data.
- Specialist input for the BPT is defined by NHFA (see above). Commissioners may wish to request from providers a list of members identified as heart failure specialists for payment purposes.
- Commissioners may wish to consider the skills and competencies required by healthcare professionals to provide the expected outcomes for people with heart failure. A further source of information is the Skills for Health website, which includes several competency tools on heart failure.
- Commissioners may wish to review the NICE commissioning guide to support the commissioning of services for people with heart failure. In particular, the NICE clinical guidelines on chronic heart failure and acute heart failure outline the importance of the multidisciplinary team in the care of people with heart failure. The multidisciplinary team may be made up of several professionals who may work with the patient at any point in the care pathway. Commissioners may choose to work with providers to develop a multidisciplinary heart failure team if one is not already in place.
- Commissioners and providers may wish to monitor whether reported improvements in the rate of specialist input correspond to improvements in other care processes measured by NHFA.
- Commissioners and providers will need to work together to ensure the accuracy of data submitted to NHFA to ensure fair and accurate payments are made.
16. Major trauma
Purpose
- The aim of the BPT for major trauma is to encourage best practice treatment and management of trauma patients within a regional trauma network. The BPT covers activity at major trauma centres for the most seriously injured patients.
Design and criteria
- The BPT is made up of two levels, differentiated by the injury severity score (ISS) for the patient and conditional on achieving the criteria set out below.
- A level 1 BPT applies for all patients with an ISS of 9 or above, providing:
- the patient is treated in a major trauma centre
- Trauma Audit and Research Network (TARN) data is completed and submitted within 25 days of discharge
- a rehabilitation prescription is completed for each patient and core components recorded on TARN with documented evidence in patient notes of a copy to the patient, GP and ongoing care provider if applicable
- any coroners’ cases are flagged within TARN as being subject to delay to allow later payment
- if the patient is transferred as a non-emergency they must be admitted to the major trauma centre (MTC) within two calendar days of referral from a trauma unit; if there is any dispute around the timing of referral and arrival at the MTC, this will be subject to local resolution
- patients with a Glasgow Coma Scale (GCS) score of <9 have documented evidence of intubation being considered within 30 minutes of arrival at the MTC.
- A level 2 BPT applies for all patients with an ISS of 16 or above, providing all level 1 criteria are met and that:
- if the patient is admitted directly to the MTC or transferred as an emergency, they must be received by a trauma team led by a consultant in the MTC; the consultant can be from any specialty, but must be present within five minutes
- patients admitted directly to a MTC with a head injury of abbreviated injury scale (AIS) 1+ and a GCS score of less than 13 (or intubated prehospital), and who do not require emergency surgery or interventional radiology within one hour of admission, receive a head CT scan within 60 minutes of arrival
- tranexamic acid is administered within one hour of arrival at scene (or arrival at the MTC for self-presentations) for patients with at least one injury associated with significant bleeding or those with a significant head injury and a GCS score of less than 13
- all patients aged 65 years or older have a Clinical Frailty Scale completed within 72 hours of admission by a geriatrician (defined as a consultant, non-consultant career grade (NCCG) or specialist trainee ST3 or above).
- While not currently a condition of level 1 payments, patients with severe injuries being admitted directly to the MTC or transferred as an emergency should be received by a consultant-led trauma team as soon as possible (ideally within 30 minutes).
Operational
- The BPT is not conditional on the patient’s HRG being in the VA chapter (multiple injuries) and applies to both adults and children.
- A patient cannot attract additional payments for both level 1 and level 2. For example, a patient with an ISS score of 17 would attract a maximum additional payment of the level 2 score, not both level 1 and level 2.
- The BPT will not be applied through SUS+, and organisations will need to use the TARN database to support manual agreeing API fixed elements.
17. Non-ST segment elevation myocardial infarction (NSTEMI)
- This BPT is designed to improve the time from admission to receiving coronary angiography for people with NSTEMI. The current national achievement rate for NSTEMI patients undergoing coronary angiography within 72 hours of admission is 55%.
- The scope of the BPT includes patients who are transferred between hospitals to receive care (that is, where a patient is transferred from one hospital to another to undergo the procedure) and so the time will be calculated from the time of admission to the first hospital.
Purpose
- Myocardial infarction (MI) is usually caused by a blockage in a coronary artery leading to tissue death and consequently the typical features of a heart attack: severe chest pain, changes on the electrocardiogram (ECG) and raised concentrations of proteins released from the dying heart tissue into the blood.
- There are two types of MI:
- ST segment elevation myocardial infarction (STEMI), which is generally caused by complete and persisting blockage of the coronary artery
- non-ST segment elevation myocardial infarction (NSTEMI), reflecting partial or intermittent blockage of the coronary artery.
- According to NICE quality standard QS68, timely angioplasty, followed by percutaneous coronary intervention (PCI) where required, is associated with improved outcomes. However, only 55% of people with NSTEMI who undergo coronary angiography do so within 72 hours of admission. The purpose of the NSTEMI BPT is to improve adherence to this quality standard.
Design and criteria
- Compliance with the BPT will be measured through the Myocardial Ischaemia National Audit Project (MINAP) database. This collects data on time from admission (arrival at hospital) to coronary angioplasty for patients experiencing both NSTEMI and STEMI events. The definitions for arrival time at hospital as used in the BPT and recorded by MINAP can be found on the NICOR website.
- Best practice will be considered to have been achieved where 60% of NSTEMI patients receiving coronary angiography (with follow-on PCI if indicated) do so within 72 hours of first admission to hospital. For patients who are transferred between hospitals for the procedure, the time will be calculated from admission (arrival) to the first (non-interventional) hospital.
- The term ‘follow-on PCI’ refers to the PCI being undertaken at the same time as the diagnostic angiogram, assuming that PCI is indicated. The best practice should only be achievable by providers that can undertake the combined procedure of diagnostic angiography and PCI (where indicated) within 72 hours of admission with NSTEMI. The BPT does not require PCI to be undertaken but it does require it to be possible at the same procedure as the angiogram, if appropriate. This is in line with the NICE quality standard QS68.
Operational
- The BPT applies at sub-HRG level (flag ‘BP50’) for all relevant non-elective admissions:
- emergency/transfer (21–25, 2A, 2B, 2C, 2D, 28, 81)
- patient aged 19 or over (on admission).
- The BPT is made up of two components: a base price and a BPT price (based on a conditional top-up payment added to the base price). The base price applies to all activity irrespective of whether the characteristics of best practice are met. SUS+ will automate the base price.
- Using a guide developed by NICOR, providers will be required to submit a validation report to commissioners. Where satisfied that providers have achieved the best practice criteria, commissioners should manually adjust the base price by applying the conditional top-up. Success against the best practice criteria is measured at provider level and for the provider that undertakes the procedure.
- The BPT applies at a sub-HRG level to ICD10 code I214 ‘acute subendocardial myocardial infarction’. This is because the HRGs will cover a larger group of patients than the BPT intends. The HRGs the BPT may apply to are listed in Annex A.
- Meeting best practice criteria, and payment of the BPT as part of API fixed elements, should be based on the latest available data.
18. Paediatric diabetes
Purpose
- The aim of the paediatric diabetes BPT is to support clinical services to deliver consistent, high-quality care to children and young people with diabetes.
Design and criteria
- The BPT is an annual payment, per patient, that covers:
- outpatient care from the date of discharge from hospital after the initial diagnosis until the patient is transferred to adult services at the age of 19
- inpatient care for any admissions related primarily to diabetes. Providers will continue to be reimbursed for admissions where diabetes is not the primary reason for admission using the usual payment mechanism outside the BPT.
- Before implementing or paying the BPT, providers and commissioners will need to agree:
- data flows and supporting information to show that the best practice criteria have been achieved (suggested evidence of validation is set out below)
- processes for identifying activity covered by the BPT to avoid duplicate payment (SUS+ will not apply the BPT).
- To qualify for the BPT the provider must demonstrate they meet all criteria as set out in Table 8 below. Information to validate compliance will be available from the:
- National Children and Young People’s Network
- National Paediatric Diabetes Audit (NPDA)
- National Children and Young People with Diabetes (CYPD) Quality Programme.
Table 8: BPT criteria and suggested evidence of achievement
|
Criteria |
Suggested evidence of achievement | |
|
a. |
Participation in the annual NPDA, with quarterly data uploads, including the patient reported experience measurement (PREM). |
|
|
b. |
Active participation in the regional paediatric diabetes network. Trusts must contribute to funding the network administration, and show that at least one representative of the CYPD multidisciplinary team (MDT) attends at least 75% of CYPD regional network meetings. |
National children and young people with diabetes Network reports |
|
c. |
Participation in a nationally agreed CYPD quality programme. |
Published national and/or network annual reports or self-assessment |
|
d. |
On diagnosis, a young person’s diabetes is to be discussed with a senior member of the paediatric diabetes team within 24 hours of presentation. |
Self-assessment |
|
e. |
All newly diagnosed patients must be seen by a member of the specialist paediatric diabetes core team by the next working weekday. |
Self-assessment
|
|
f. |
Each newly diagnosed patient has an individualised, structured education programme, that includes being educated about level 3 CHO counting within two weeks of diagnosis (Type 1) or given advice about appropriate weight management (Type 2). |
Self-assessment
|
|
g. |
Each patient is offered a minimum of four clinic appointments per year with a MDT, defined as including a paediatric diabetes specialist nurse, a paediatric diabetes dietitian, paediatric clinical psychologist and doctor. At every visit, the patient must be seen by a doctor with appropriate training in paediatric diabetes and at least one other member of the MDT. At least 90% compliance is expected for this criterion. |
Self-assessment |
|
h. |
Each patient is offered additional contact by the MDT for check-ups, telephone contacts, emails/texts, school visits, home visits, troubleshooting, advice, support, etc. Eight contacts per year are a minimum requirement. At least 90% compliance is expected for this criterion. |
Self-assessment |
i. |
Each patient is offered at least one additional appointment per year with a paediatric dietitian with training in diabetes (or equivalent appropriate experience). At least 90% compliance is expected for this criterion. | |
|
j. |
Each patient is offered a minimum of four haemoglobin HbA1c measurements per year. All results must be available and recorded at each MDT clinic appointment. At least 90% compliance is expected for this criterion. |
Self-assessment |
|
k. |
All eligible patients must be offered annual screening as recommended by current NICE guidance. |
Self-assessment |
|
l. |
Discussion of the mental health and wellbeing of a patient should be an integral part of a patient’s review with their MDT. Each patient must be assessed at least annually by their MDT as to whether additional psychological support is needed. The provider of formal psychological support for diabetes-related problems must be an integral part of the MDT. | |
|
m. |
Each provider unit must provide patients and their families with 24-hour access to advice and support. This should also include 24-hour expert advice to fellow health professionals on the management of patients with diabetes admitted acutely, with a clear escalation policy on when further advice on managing diabetes emergencies should be sought. The provider of expert advice must be fully trained and experienced in managing paediatric diabetes emergencies. |
Self-assessment |
|
n. |
Each provider unit must have a clear policy for their transition diabetes care and subsequent transfer to adult services. The policy must be in line with National Guidance on Transition. Each provider unit must also ensure that it has in place clear protocols and guidelines for treatment of 16 to 18 year olds admitted for diabetic ketoacidosis (DKA) and that these have been agreed with adult services. |
Self-assessment
|
|
o. | Each unit must have an operational policy that clearly sets out: i) a policy for children and young people who have a high HbA1c level (≥ 69 mmol/mol) as a result of poor blood glucose controlii) a policy for children and young people who ‘did not attend/were not brought’ (DNA/WNB) to clinic, taking into account local safeguarding children board policies. |
Self-assessment |
|
p. |
Clinically appropriate NICE recommended diabetes self management technology should be offered to and discussed with patients annually. |
Self-assessment |
- The BPT payment will also cover:
- patient education about using insulin pumps, continuous glucose monitoring (CGM) and hybrid closed loop systems, whether provided as an inpatient, outpatient or day case
- intermittent CGM for diagnostic purposes
- blood glucose testing strips and insulin prescribed as an emergency by the MDT.
- The BPT does not cover:
- the cost of insulin pumps and associated consumables
- the cost of CGM systems when used continuously for therapeutic purposes
- routine prescriptions for insulin, blood glucose testing (including flash glucose scanning/FreeStyle Libre) and ketone monitoring issued in primary care.
- Where commissioners are satisfied that the criteria have been achieved, the BPT level of payment should be factored into the fixed element to cover all patients attending the clinic.
- If a patient is referred elsewhere for a second opinion, shared care or full transfer of care, and if the referring and receiving centres wish to share the distribution of the BPT payment, they will need to agree subsequent division of funding using a service-level agreement. The precise division of funding will need to be negotiated locally.
- Annex A sets out the paediatric diabetes BPT prices, per patient that receives care that meets the criteria. Providers and commissioners are asked to agree their API fixed element based on an assessment of expected paediatric diabetes patient numbers and whether the provider is likely to deliver best practice.
- Where best practice is not delivered when the funding was made available in the fixed element, this should be discussed and a plan put in place, or funding adjustments made, in the next financial year/planning process. No in-year payment adjustments should be made.
- In areas of higher socioeconomic deprivation, an uplift in funding level may be considered appropriate by commissioners and providers to enable an enhanced offer of care to be delivered.
- The funding provided by the paediatric diabetes BPT is integral to high quality care for a patient cohort with high clinical need. If commissioners intend to vary away from this national pricing guidance, and reduce funding for their local paediatric diabetes service to a level that is less than what a service delivering best practice care is expected to cost, a written justification will need to be agreed between the provider and commissioner and published.
19. Paediatric epilepsy
Purpose
- The aim of the BPT is to enable access to consistent high-quality care for children with epilepsy.
- There is an ongoing need to improve the quality of, and reduce the variation in, care for children with epilepsy in the UK in line with the recommendations in NICE clinical guideline CG137 Epilepsies: diagnosis and management. This includes accuracy of diagnosis, classification and suitable drug choices. It requires improvement in adequate communication and care planning, including comorbidity diagnosis management and school support.
- Trusts should develop services that include appropriate access to epilepsy specialist nurses (ESNs), mental health professionals and paediatricians with expertise in epilepsies. ESNs form a fundamental bridge between primary, secondary and tertiary care and epilepsy surgery care. They ensure that epilepsy is managed in the community and school when needed rather than just in the hospital ward or clinic.
Design and criteria
- The BPT has three levels:
|
Level |
Description |
Coding |
|
Level 1 |
Where a provider is unable to demonstrate compliance with the BPT |
TFC 420 (Paediatrics) |
|
Level 2 |
Where a provider is able to demonstrate compliance with the BPT (criteria a to h) |
TFC 223 (Paediatric epilepsy) |
|
Level 3 (non-mandated) |
Where a provider is able to demonstrate compliance with criteria i (mental health provision) |
Local data |
- Compliance with the BPT criteria to be measured using the Epilepsy12 national clinical audit reporting tools.
- The BPT is payable to providers of a service that meets all of the criteria listed in Table 9.
Table 9: BPT criteria and evidence of achievement
Criteria |
Evidence of achievement | |
|
Level 2 | ||
|
a | The provider has continuously and fully participated in the Epilepsy12 national audit. This is defined as the provider submitting data to service descriptor, clinical and PREM domains as defined by the audit. |
Epilepsy12 participation |
|
b |
The trust has a defined paediatric epilepsy clinical lead. |
Epilepsy12 service descriptor SD4 |
|
c |
ESN(s) are employed in the provider. |
Epilepsy12 service descriptor SD5 |
|
d |
The provider routinely plans comprehensive care for children with epilepsy. |
Epilepsy12 service descriptor SD27 |
|
e | The provider’s epilepsy clinics allow at least 20 minutes with a consultant with expertise in epilepsy and an ESN. This may be at the same time or at separate appointments. |
Epilepsy12 service descriptor SD6 |
|
f |
The provider has specific outpatient clinics for ‘young people’ with epilepsies. |
Epilepsy12 service descriptor SD18 |
|
g | The provider has agreed referral pathways for children with: · neurodevelopmental problems (eg autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD))· mental health concerns (eg anxiety, mood disorders and non-epileptic attack disorders) · tertiary paediatric neurology services· adult services. |
Epilepsy12 service descriptor SD23 |
|
h |
Where the provider does not achieve the level 3 mental health provision (described in criteria i), they must have an agreed action plan describing steps towards integrating mental health provision in epilepsy clinics. |
Epilepsy12 service descriptor SD24 |
|
Level 3 (non-mandated) | ||
|
i | The provider has mental health care integrated within the epilepsy service. This comprises epilepsy clinics where mental health professionals can provide direct input into clinical care and MDT meetings where epilepsy and mental health professionals discuss individual patients |
Epilepsy12 service descriptor SD24 |
- The BPT covers outpatient care after the first acute or outpatient assessment. It applies to patients aged 18 and under with a diagnosis of epilepsy, until they transfer to adult services.
Operational
- Only activity meeting the level 2 best practice criteria should be coded against TFC 223 (Paediatric epilepsy). Where a provider codes to TFC 223 but is unable to demonstrate compliance with the BPT, then funding equivalent to the price for TFC 420 (Paediatrics) should apply. The TFC 223 (Paediatric epilepsy) first attendance price does not require BPT compliance.
- Epilepsy12 methodology is designed to help trusts demonstrate compliance with the BPT. Commissioners and providers should monitor compliance with the criteria, using Epilepsy12 locally, to determine the relevant payment against the TFC 223.
- To support the BPT, Epilepsy12 will publish annual reports that include the BPT dataset. However, this will be based on the previous audit year. To support continued improvement and timely payment, trusts will be able to update their service descriptor domain data during the year. The audit includes an export function to generate updated quarterly reporting to support validation. Epilepsy12 will also make available provisional participation reports annually, based on the previous audit year.
- The BPT does not include costs related to:
- acute inpatient care
- epilepsy investigation and treatment costs (eg electroencephalography, magnetic resonance imaging, drugs, surgery, vagal nerve stimulation, ketogenic diet, etc) with the exception of the costs of blood tests
- the assessment and treatment for other (non epilepsy-related) health problems not normally treated in an epilepsy clinic
- more complex epilepsy patients who, in line with NICE guidelines, have shared care with a paediatric neurologist and are coded to the paediatric neurology TFC. The percentage of patients in a particular clinic, service or provider who have shared care with neurology will depend on local pathways and casemix. This is estimated to range from 30% to 60%.
- SUS+ will automatically apply the BPT (level 2) to activity coded to TFC 223 (Paediatric epilepsy). Activity must only be coded to this TFC if it meets the level 2 best practice criteria.
- Where both provider and commissioner have agreed to fund and deliver the level 3 criteria, and the commissioner is satisfied the criteria have been achieved, commissioners should reflect this in the agreed API fixed element.
- The pricing approach using TFC 223 is designed to adequately reimburse the costs of best practice (at level 2). Activity captured within the general paediatric TFC (TFC 420) does not reflect the costs of best practice.
20. Parkinson’s disease
Purpose
- Parkinson’s therapy in secondary care settings ranges from basic (a care of elderly or neurology review) to comprehensive (multidisciplinary review with full access to therapy services).
- The aim of this BPT is to enable access to consistent high-quality management of Parkinson’s disease, in line with NICE clinical guidelines, to reduce unscheduled care and length of stay in hospital.
Design and criteria
- The BPT applies to adults with a probable diagnosis of Parkinson’s disease where care during the first year is delivered in line with the criteria below. This is an annual payment to reflect the costs from the initial referral date for the first year of care only. The BPT excludes the costs of admitted patient care and the cost of any items not covered by unit prices.
- The criteria for best practice are:
- Referrals from primary care with suspected Parkinson’s disease must be seen by a movement disorder specialist (neurology/elderly care) within six weeks. These timescales apply to all patients for the purposes of the BPT, but the expectation is that new referrals in later stages of disease with more complex problems will continue to be seen within two weeks.
- Each patient must receive regular follow-up and diagnostic review with a specialist nurse at least every six months with a process to identify the appropriate period of follow-up. Each patient must have a nominated person identified to continue with follow-up and diagnostic review.
- All patients must be referred to a Parkinson’s disease nurse specialist (PDNS) (local titles may include neurology nurse specialist or movement disorder specialist) who will be responsible for co-ordinating care.
- Evidence to demonstrate that the provider is using recognised tools: for example, patient feedback, non-motor symptoms (NMS) screening tool and cognitive assessment tool.
- Patients must be offered therapy assessment within one year (including physiotherapist, speech and language therapist and occupational therapist). The BPT does not include the costs of the therapy assessment. However, payment depends on therapy assessment being offered (irrespective of whether the patient takes this up). In a few circumstances, therapy assessment is not relevant – where providers are able to evidence this, the BPT still applies.
- Commissioners must monitor compliance with the criteria through evidence provided by providers, which may include local records of clinic attendances, local education programmes, etc. Where a provider does not meet all the criteria, activity should continue to be paid outside of BPT pricing.
- The criteria for the BPT are underpinned by:
- NICE clinical guideline 71, Parkinson’s disease in adults
- National Service Framework for long-term conditions
- recommendations 12 and 13 of Local adult neurology services for the next decade – report of a working party, Association of British Neurologists and the Royal College of Physicians
- The European Parkinson’s disease standards of care consensus statement, European Parkinson’s Disease Association, Volume I, 2011.
Operational
- SUS+ will not apply the BPT and there is no discrete TFC for Parkinson’s disease activity. Organisations will therefore need to identify activity and administer the BPT locally. Therefore, activity meeting best practice may need to be excluded from the CDS to avoid double payment. Providers can achieve this by including an equals sign (=) as the last significant character of the six-character CDS data item Commissioning Serial Number. The equals sign would exclude the episode.
- One way to identify the activity for consideration against the BPT is to use the non-mandatory diagnosis codes in outpatients (G20X).
- If a patient is referred elsewhere for a second opinion, shared care or full transfer of care, and if the referring and receiving centres wish to share the distribution of the BPT payment, they will need to agree subsequent division of funding using a service-level agreement. The precise division of funding will need to be negotiated locally.
- The pricing approach is designed to adequately reimburse the costs of best practice. At present, the activity covered by the BPT is captured within a non-mandatory neurology TFC (TFC 400), which does not reflect the costs of best practice.
21. Referral of appropriate post-myocardial infarction (STEMI) patients to cardiac rehabilitation
Purpose
- Cardiac rehabilitation is a co-ordinated and structured programme designed to remove or reduce the underlying causes of cardiovascular disease. It provides the best possible physical, mental and social conditions so that people can, by their own efforts, continue to play a full part in their community. A healthier lifestyle and slowed or reversed progression of cardiovascular disease can also be achieved (NICE guideline CG172).
- Myocardial infarction (MI) is usually caused by blockage of a coronary artery causing tissue death and consequently the typical features of a heart attack: severe chest pain, changes on the ECG and raised concentrations of proteins released from the dying heart tissue into the blood. There are two types of MI:
- ST segment elevation myocardial infarction (STEMI), which is generally caused by complete and persisting blockage of the coronary artery
- non-ST segment elevation myocardial infarction (NSTEMI), reflecting partial or intermittent blockage of the coronary artery.
- People who are referred to rehabilitation programmes early have better rates of uptake and adherence and hence improved clinical outcomes.
Design and criteria
- The BPT is designed to incentivise referral to cardiac rehabilitation services of appropriate post-STEMI patients within three days of an initiating event and before discharge. Nationally, an estimated 50% of people post-STEMI are referred within three days to cardiac rehabilitation. The target compliance rate is 60%: that is, 60% of patients need to be referred to cardiac rehabilitation services within three days of an initiating event for the BPT payment to be made. There is a data field in the National Audit of Cardiac Rehabilitation (NACR): ‘the primary reason why the patient was referred to Cardiac Rehabilitation, this may be a diagnosis such as MI or treatment such as CABG’.
- We recommend a 10% payment differential between the base and BPT price (that is, 10% between BPT and non-BPT price).
Operational
- The HRGs in Table 10 below fall within the scope of this BPT.
Table 10: HRGs within the BPT’s scope (where there is also a primary diagnosis included from Table 11)
|
HRG code |
HRG name |
|
EB10A |
Actual or Suspected Myocardial Infarction, with CC Score 13+ |
|
EB10B |
Actual or Suspected Myocardial Infarction, with CC Score 10-12 |
|
EB10C |
Actual or Suspected Myocardial Infarction, with CC Score 7-9 |
|
EB10D |
Actual or Suspected Myocardial Infarction, with CC Score 4-6 |
|
EB10E |
Actual or Suspected Myocardial Infarction, with CC Score 0-3 |
|
EY40A |
Complex Percutaneous Transluminal Coronary Angioplasty with CC Score 12+ |
|
EY40B |
Complex Percutaneous Transluminal Coronary Angioplasty with CC Score 8-11 |
|
EY40C |
Complex Percutaneous Transluminal Coronary Angioplasty with CC Score 4-7 |
|
EY40D |
Complex Percutaneous Transluminal Coronary Angioplasty with CC Score 0-3 |
|
EY41A |
Standard Percutaneous Transluminal Coronary Angioplasty with CC Score 12+ |
|
EY41B |
Standard Percutaneous Transluminal Coronary Angioplasty with CC Score 8-11 |
|
EY41C |
Standard Percutaneous Transluminal Coronary Angioplasty with CC Score 4-7 |
|
EY41D |
Standard Percutaneous Transluminal Coronary Angioplasty with CC Score 0-3 |
|
EY42A |
Complex Cardiac Catheterisation with CC Score 7+ |
|
EY42B |
Complex Cardiac Catheterisation with CC Score 4-6 |
|
EY42C |
Complex Cardiac Catheterisation with CC Score 2-3 |
|
EY42D |
Complex Cardiac Catheterisation with CC Score 0-1 |
|
EY43A |
Standard Cardiac Catheterisation with CC Score 13+ |
|
EY43B |
Standard Cardiac Catheterisation with CC Score 10-12 |
|
EY43C |
Standard Cardiac Catheterisation with CC Score 7-9 |
|
EY43D |
Standard Cardiac Catheterisation with CC Score 4-6 |
|
EY43E |
Standard Cardiac Catheterisation with CC Score 2-3 |
|
EY43F |
Standard Cardiac Catheterisation with CC Score 0-1 |
Table 11: Target population ICD10 codes (primary diagnosis)
|
ICD10 code |
Description |
|
I210 |
Acute transmural myocardial infarction of anterior wall |
|
I211 |
Acute transmural myocardial infarction of inferior wall |
|
I212 |
Acute transmural myocardial infarction of other sites |
|
I213 |
Acute transmural myocardial infarction of unspecified site |
|
I219 |
Acute myocardial infarction, unspecified |
|
I220 |
Subsequent myocardial infarction of anterior wall |
|
I221 |
Subsequent myocardial infarction of inferior wall |
|
I228 |
Subsequent myocardial infarction of other sites |
|
I229 |
Subsequent myocardial infarction of unspecified site |
- The number of patients referred to cardiac rehabilitation should be calculated through the NACR. Providers will be expected to supply the commissioner, on a quarterly or more frequent basis, with the number of patients referred for cardiac rehabilitation as a proportion of all relevant activity.
- We have developed a specification to calculate the relevant activity for assessing compliance with the BPT criteria emergency/transfer (21-25, 2A, 2B, 2C, 2D, 28, 81)
- ICD10 codes (as in Table 11)
- HRGs (as in Table 10)
- discharge destination: usual place of residence (19).
- The price generated by the grouper and SUS+ is the conventional price. Where a provider and commissioner have agreed a pricing structure for the BPT, this should be reflected in API fixed elements.
- In calculating the target population, only patients discharged home should be included, to ensure that patients transferred between hospitals are not included more than once across providers.

