Using data and analysis to enable effective decision-making
Classification: Official
Publication approval reference: PAR1189
Foreword
The COVID-19 pandemic has taught us a great deal about the power of integrated data and intelligence to address urgent needs. When it comes to using data to meet the needs of different communities, it has driven us to go further, faster.
Data was essential to our day-to-day response to the pandemic, with local health and care system partners working closely with analysts to develop high quality insights at pace.
Data enabled us to identify those who are most vulnerable to coronavirus, helping us to build a more effective shielding list and prioritise vaccinations, and it enabled teams to find and support specific groups who were most at risk from isolation and the wider social impacts resulting from the pandemic.
Data also powered vital research that helped to discover new treatments that have saved many lives.
Across the health and care system people are using data more efficiently and effectively than ever before. Having access to accurate real-time information is transforming how we plan, manage, and sustain services, enabling leaders, clinicians and frontline teams to make more informed and effective decisions.
With integrated care systems (ICSs) now on a statutory footing following the establishment of integrated care boards (ICBs) and integrated care partnerships (ICPs), it is time for them to unlock the potential of integrated data and population health analytics to develop a deeper understanding into the extent and nature of the health inequalities within their populations.
Data-driven population health approaches will be a key tool in our response to these inequalities. The challenge for ICSs will be to quickly develop their use of population health analytics, from using data to inform their approach to condition management, to utilising predictive risk factors that help to increase early detection and prevent ill health.
Person and pathway centred datasets, including information about the wider determinants of health, are needed, as well as the analytical teams and data-literate leaders that can make use of them.
These approaches are needed now more than ever, not only to target health inequalities and variation in care quality at a local level, but also to help systems to make the best use of their collective resources and to track and measure outcomes in more tailored and effective ways.
The work we are starting with ICSs and place-based teams on the new Integrated Care Experience Survey, which will help to fulfil the Long-Term Plan commitment of an Integration Index, will provide one important way to assess the outcomes of personalised, integrated care.
Population health analytics should be used within a wider population health management (PHM) approach that not only ensures groups most at risk of ill-health are prioritised to receive preventative care, but also supports clinical and care staff in place-based teams to design and deliver new integrated care models that are tailored for these at-risk groups.
These local teams can only do this if they have a detailed understanding of their diverse communities that is not only informed by rich datasets, but also by qualitative insights into the needs and experiences of these communities. In order to achieve this, analytical, information governance and data security teams must take steps to ensure their use of data is lawful and transparent, complying with relevant legal requirements to respect the rights of individuals. This should allow local teams to gain and maintain the trust of patients and the public in safeguarding their confidential health and care information.
This guidance and the accompanying toolkit provide systems with a framework for developing their use of data, analytics and insights in these ways by building multi-disciplinary, cross-organisational intelligence functions that sit at the heart of their approach to care design and delivery. The guidance has been heavily shaped by ICSs across the country and is built from local good practice examples which the toolkit describes in more detail.
Levels of data and analytical maturity vary nationwide, but used to its full effect this guidance will provide teams with a springboard to improve performance through the use of evidence. It also provides details on how systems can develop their local data architecture as part of the national whole, so that we can create an effective learning system across the entire health and care landscape.
Ultimately, systems need to ensure that their decision-making is based firmly on the best possible intelligence at every level – not only across the system as a whole, but also within their place-based and integrated neighbourhood teams. The Fuller stocktake report and the work ICSs have done to embed population health management has highlighted the importance of local analytical teams working symbiotically with neighbourhood teams to understand population need and to translate data into new care models
Data and analytics should not just drive smarter planning, care co-ordination and performance management at the overall ICS level, but should also be supporting staff to deliver transformation on the front line.
We have asked systems to appoint a chief analyst, or an equivalent executive leader, whose role will be to realise this vision for the widespread use of data, analytics and insight – but in order to achieve real change it is just as important that all leaders across each ICS commit to the routine use of evidence as a core principle within health and care.
The opportunities presented by using intelligence to save lives and improve well-being are close to endless, and our journey together in this space has only just begun.
Matt Neligan
Director of System Transformation
NHS England
Ming Tang
Chief Data and Analytics Officer
NHS England
The challenge
The COVID-19 pandemic has demonstrated the importance to local leaders of the ability to draw upon the right intelligence at the right time. This would not have been possible without analytical collaboration between the NHS, local authorities, and other partners. System-wide analytical working is crucial to inform planning decisions that address cross-system priorities to deliver the best health and social care for local populations and support improved and equitable health and wellbeing.
For this to happen, a multi-disciplinary approach is needed that requires analytical teams to work seamlessly with frontline clinical teams, including GPs, public health, service redesign, quality improvement and financial transformation teams. This joined-up approach is intended to drive responsive and data-led decision making about population health and service integration through the use of quantitative and qualitative data and insights from across the system.
Putting data, analytics and intelligence at the heart of an ICS will support ICBs, ICPs, providers and place-based partnerships to act in the interests of people, communities and populations.
Background
Integrating care: Next steps to building strong and effective integrated care systems across England, first published in November 2020, announced the expectation for ICSs to: “develop shared cross-system intelligence and analytical functions that use information to improve decision-making at every level, including:
- actionable insight for frontline teams
- near-real time actionable intelligence and robust data (financial, performance, quality, outcomes)
- system-wide workforce, finance, quality, and performance planning
- the capacity and skills needed for population health management.”
This vision was supported in the NHSx What Good Looks Like framework, in which success measure 7 describes how ICS digital and data capabilities can support ‘healthy populations’. It specified a number of measures that would be delivered or supported by the ICS intelligence function, including a key role in driving PHM:
- Lead the delivery and development of an ICS-wide population health intelligence platform with a fully linked, longitudinal dataset (including primary, secondary, mental health, social care and community data) to enable population segmentation, risk stratification and PHM – these platforms must be part of the national whole to ensure that we create a learning system across health and care.
- Use data and analytics to redesign care pathways and promote wellbeing, prevention, and independence (for example, identifying patients for whom remote monitoring is appropriate).
- Create integrated care models for at-risk population groups, using data and analytics to optimise the use of local resources and ensure seamless co-ordination across care settings.
- Ensure that local ICS and place-based decision-making forums, as well as PCN MDTs, have access to timely population health insight and analytical support.
- Make data available to support clinical trials, real-world evidencing, and AI tool development.
- Drive ICS digital and data innovation through collaborations with academia, industry, and other partners.
The 2022/23 priorities and operational planning guidance re-emphasised the importance of PHM and prevention approaches, and the use of data and analytics to drive these activities. It called for systems to work together to share data and analytic capabilities and in particular:
- to develop plans to put in place the systems, skills and data safeguards that will act as the foundation for this.
- to have in place the technical capability required for PHM, including:
- longitudinal linked data available to enable population segmentation and risk stratification
- using data and analytics to redesign care pathways and measure outcomes, with a focus on improving access and health equity for underserved communities.
More recently, the 2023/24 priorities and operational planning guidance has re-stated the need for organisations to put the right data architecture in place for population health management (PHM), as well use forthcoming digital maturity assessments to measure progress towards the core capabilities set out in What Good Looks Like.
NHS England and the Government also recently published two major strategic plans: Data Saves Lives, which is the data strategy for health and social care, and A Plan for Digital Health and Social Care which is the strategy to digitise services, connect them to support integration and to use this platform to transform services, creating fundamentally new care models.
Data Saves Lives sets out plans to harness the potential of data in health and care, while maintaining the highest standards of privacy and ethics. It emphasises the need to put in place the right technical architecture and establish effective governance to oversee and guide this work. It also describes how we must take targeted action to build public trust around how we use data in the NHS.
A Plan for Digital Health and Social Care sets out NHS England and the Government’s delivery plans to March 2025 and describes a vision for digitally transformed health and care services beyond 2025. It is aimed at health and social care leaders across the system and industry partners who supply the health and care system.
In addition, the Goldacre review into the use of health data for research and analysis emphasised the importance for the NHS and its partners to work collaboratively to unlock the potential of data-led insights, with a focus on transparency and data privacy through the development of trusted research environments. It calls for investment in analytics within the health and care sector, including growing, upskilling and professionalising the analytical workforce.
This guidance document
This guidance builds on and clarifies the expectations of ICS intelligence functions, which have been previewed in other guidance published over the past two years, including Integrated Care Systems: Design Framework and more recently in the priorities and operational planning guidance over the last two years (as described above).
It has been developed in partnership with ICSs around the country, building on the many emerging examples of good practice in this area. It explains what an ICS intelligence function should aim to do and what an emerging, developing, and maturing intelligence function could look like. It will be supplemented over the course of 2023 by further support documents about ways in which systems can build their intelligence functions, covering areas such as data architecture (including information governance) and the development of the analytical workforce.
Importantly, this is not intended to be a prescriptive vision, or a set of national ‘must dos’. It aims to describe a set of principles and components that ICS teams shared with us throughout 2021 and 2022. That said, the following expectations will help to ensure that the existing 2022/23 planning guidance commitments, including those listed above, can be delivered by systems in an effective manner:
- During 2023, to continue to put in place cross-system information governance arrangements, particularly between primary and secondary care and local government partners, that enable the safe and timely flow of information across the ICS and support the ICB to deliver its functions.
- During 2023, to appoint a chief analyst (or an equivalent role, such as chief data and analytics officer) to lead the intelligence function, supported with the responsibility for putting in place clear reporting arrangements into ICB, ICP and place-based decision-making forums to ensure insight into population need is informing local strategies and transformation priorities.
What is an intelligence function?
An intelligence function is a system-wide, multi-disciplinary collaboration of intelligence professionals, with representation from analytical leaders and key teams across the whole ICS. At its core, it is a way of co-ordinating a diverse range of analytical skills to support the needs of the system.
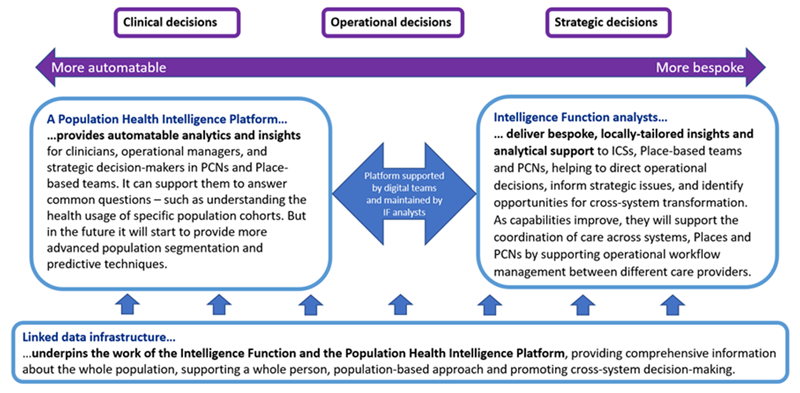
The purpose of the intelligence function is to ensure that decisions across system, place and neighbourhood teams are routinely informed by evidence that is tailored to the local context, including a detailed understanding of health inequalities between population groups, and that the system is supported to take a population-based approach to care planning and delivery, including the use of data to shape the personalisation of care. Figure 1 (on page 11) describes different uses of health and care data, including those that the intelligence function may take a lead role in. NHS England is currently producing a suite of data products to support ICSs in their approach to these activities. More information on analytical tools is provided in Appendix 1, below.
While it may have its initial basis within core teams in the ICB, the intelligence function should be collaborative and multi-organisational, comprising analysts and other insight specialists from all constituent parts of the ICS – including NHS provider organisations, local authority care services, public health teams and voluntary sector partners – and serving the strategic goals of the ICP.
Local foundations
By benefiting from this diverse expertise and building on existing resources, its work will be founded on a detailed and comprehensive understanding of the local population. For example, systems may wish to consider the role of their intelligence function when developing their approach to people and community engagement, to ensure that the insight generated – both qualitative and quantitative – is incorporated into their wider intelligence about the population.
This approach will support the system to hone its allocation of resources, including through an emphasis on preventative care for groups who are most at risk of ill-health. These shared assets of data and insight mean that the intelligence function can act as a trusted integrator of the different partners of the ICS and work across traditional organisational and contractual boundaries to progressively focus on proactive, population-based models of care that support individuals across the life course.
Collaboration with other ICS teams
As well as incorporating a wide range of analytical disciplines, an effective intelligence function would be supported by digital and information governance teams and would work in partnership with other ICS teams, such as transformation, operations, care quality and finance teams.
In this way, the intelligence function would not be treated as a support service but rather would work with ICS teams as an active partner, providing systematic input into decision-making and service design through the production of timely and robust evidence, and routinely equipping teams with intelligence that drives improvements in performance.
This model can be particularly demonstrated in PHM, where the role of the intelligence function would be to empower clinicians and other care staff with actionable insights about specific population groups that they can use to design and support the implementation of new pro-active personalised care models.
This would be underpinned by a co-ordinated, system-wide approach to information governance that ensures as far as possible that relevant professionals from all relevant teams and organisations have access to the data and tools they need.
Governance structure
A robust intelligence function will benefit from a clear governance structure, with links into the ICB and ICP to ensure that its outputs are informing key decisions while receiving appropriate steer and oversight. It would be led by a chief analyst (or an equivalent role): a senior ICS leader with responsibility for information or analytics with appropriate analytical knowledge, skills, and experience, who can bring together organisations to deliver the specific population-based needs of the system.
Some systems may wish to organise their intelligence function in line with the key ICS design principle of subsidiarity by allocating appropriate dedicated resource to each place within the system and providing direct support to integrated neighbourhood teams. In larger or more heterogeneous ICSs it may make sense for intelligence functions to be organised more distinctly at place level, with greater place-level autonomy and a more federated governance structure.
Learning networks
Intelligence functions are encouraged to operate within a national and a regional learning network, using best-practice tools, resources and wider datasets provided by national teams and local knowledge and intelligence services, and sharing and collaborating on analyses and approaches with teams from other ICSs, tailoring these where necessary to the local context.
Regional analytical teams will support ICSs in their development of intelligence functions, and will act as the hub for collaboration with the national thematic analytical teams and with other national bodies, with the local insight generated by intelligence functions increasingly informing decisions about national and regional planning and transformation priorities.
National enablers
There are a number of programmes in development or underway nationally that will support and enable the local development of your intelligence functions.
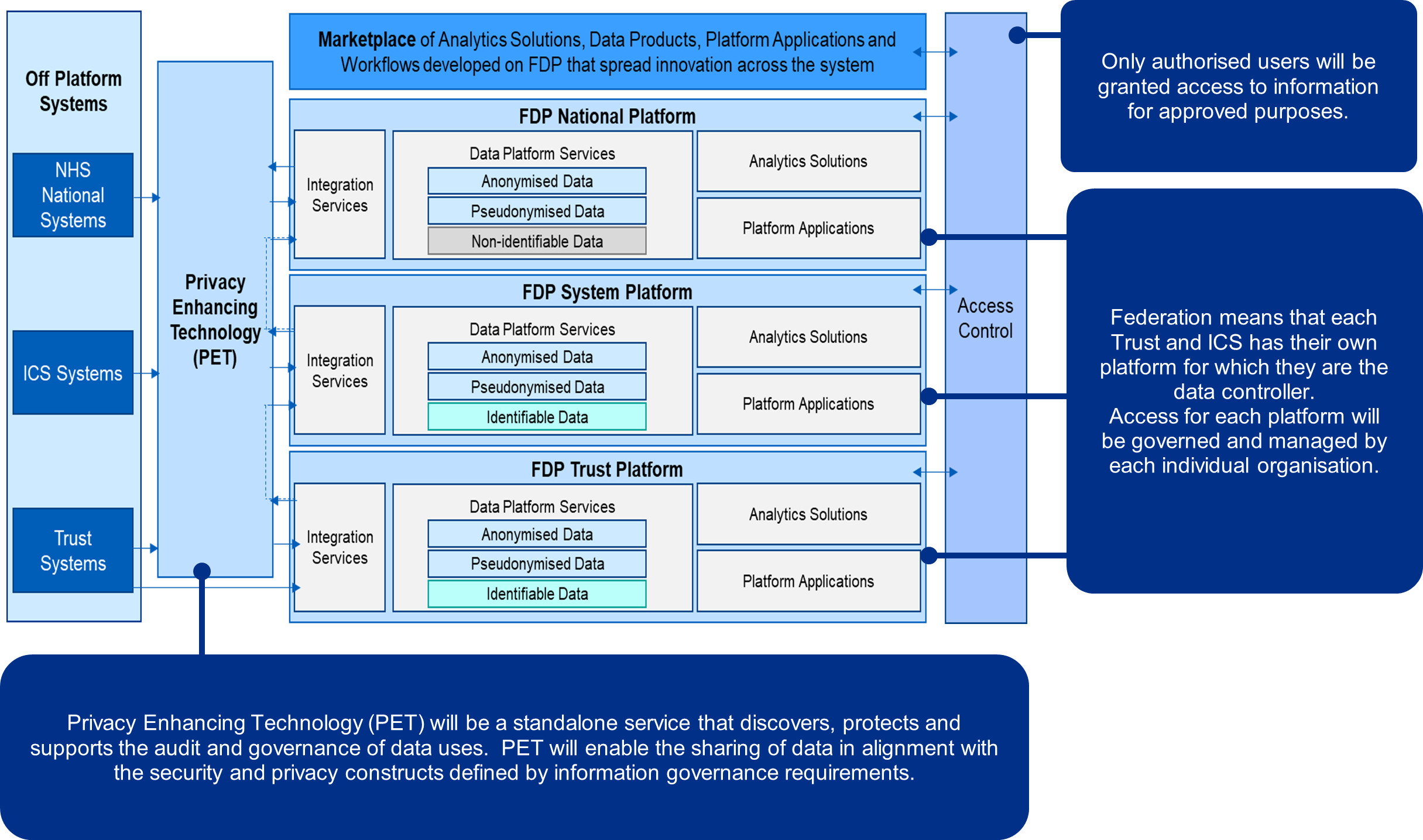
Federated Data Architecture
NHS England is currently developing a federated data architecture and a common data platform. As such, systems will need to ensure their local data infrastructure and functionality coheres with the national offer and is consistent with national standards.
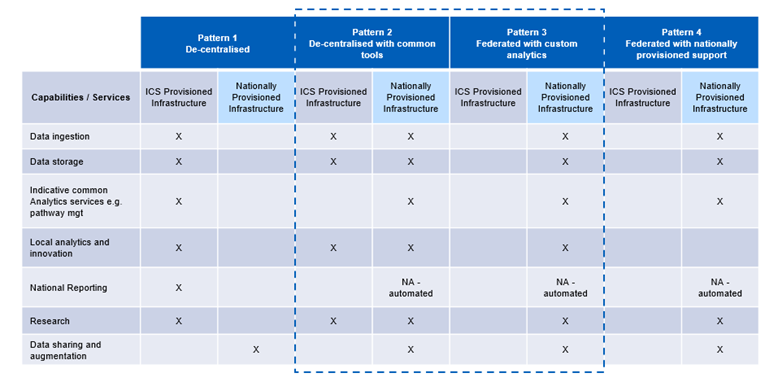
Further details on these plans can be found in Appendix 2, which include a description of the different ways in which systems can achieve this coherence with the national system, depending on their desired level of local flexibility versus their desire to take advantage of nationally-provided products.
More information about the federated data architecture will be provided by NHS England in the coming months, accompanied by tools and resources to support systems in their local planning against these requirements.
As part of the Federated Data Platform, Privacy Enhancing Technology (PET) will be a standalone service that discovers, protects and supports the audit and governance of data uses in line with those in figure 1. PET will enable the sharing of data in alignment with the security and privacy constructs defined by information governance requirements.
Secure data environments
NHS England is changing how NHS health and social care data is made available for research and analysis. Secure data environments were identified in the Data saves lives strategy as the default way that NHS health and social care data will be accessed for research and analysis in future.
The Secure data environment policy guidelines set out expectations for how Secure Data Environments will be used, and the rules by which all platforms providing access to NHS data will need to comply.
Information governance and privacy
The Information governance framework for integrated health and care: shared care decords – NHS Transformation Directorate (england.nhs.uk)provides guidance on the use of confidential patient information in shared care record systems for direct care. However, analytical leads will need to work with local IG leads to ensure that they have a legal basis for using confidential patient information for purposes other than direct care; developing and making readily available to patients and the public a range of information materials that explain how and why their information is used; and establishing processes that support individuals exercising their data protection rights.
Who does what
The Who Does What programme will support ICSs to understand technology platforms or services that are available nationally to support investment decisions and avoid duplication. The National Service Catalogue – currently in beta – should be seen in the context of a wider programme of work that aims to provide a more joined-up approach to technology and data solutions.
Professionalising data and analytics
There are several commitments in the Data Saves Lives strategy which are specifically aimed at strengthening the profession of data and analytics. NHS England is in the final stages of developing a competency framework for data and analytics professionals (data analysts, data engineers and data scientists) which will help partners across an ICS to understand and value the work of data and analytics and can be used to design and inform roles in an intelligence function, including the head/ chief analytical officer. More information is available on FutureNHS.
Figure 1: Uses of health and care data (in line with Information governance framework for integrated Health and Care)
1. Use case: Direct care
- Single shared care record which sits across all health and care settings and is interoperable with clinical workflow systems
- Safe cross-organisation care delivery (including beyond Primary Care Network (PCN), Place, ICS or Regional boundaries)
- Remote and assistive technology, utilisation measurement tools and information sharing platforms to enable providers to monitor, understand and influence how interventions impact on outcomes and communicate with patients through different channels
User types:
- Clinical and care staff
- Citizens
Access and latency:
- Real-time, read/write access
- Identifiable data required
Data types:
- Linked event-based patient record
- Past/future appointments/pathway information
- Care plans, communications, safeguarding
2. Use case: Population health and proactive care
- Whole population approaches to understanding needs of different groups and communities, and current and future risks that drive poor outcomes, including the impact of wider socio-economic factors
- Near real-time risk stratification, and demand and capacity modelling to support care coordination across PCN multi-disciplinary teams and flow into and out of acute settings
- Care model design by integrated place-based teams
- Information sharing platforms to enable providers to monitor, understand and influence how interventions impact on outcomes
- Screening/prevention, case finding, proactive care, decision support
User types:
- Intelligence functions, PCN multi-disciplinary teams, and other authorised health and care staff across ICBs and ICS partners, including local authorities
Access and latency:
- Daily/real-time updates
- Identifiable data required by authorised staff to enable direct care (eg place, provider level)
Data types:
- Aggregated linked patient/person records (clinical, demographic, wider social determinants, outcomes)
- Provider/place/workforce data
3. Planning, oversight and service improvement
- Understand future drivers for change across the health economy and strategic redesign and realignment of services to meet population health needs
- Population based financial planning, clinical quality improvement and place-based budget management
- Capacity and demand management, health inequality insight, performance management (safety, quality, experience), workforce planning, financial MI/contracting
User types:
- Intelligence functions, place-based teams, ICPs, ICBs, and other authorised health and care staff across ICS partners, including local authorities
- National bodies
- Public
Access and latency:
- Weekly -> hourly updates (depending on criticality of action)
- Must not be identifiable and have clear principles for what level of sharing is appropriate for whom, including for open data/dashboards
Data types:
- Operational data (capacity, demand, activity/utilisation, cost, experience, safety, assets)
- Aggregated linked patient/person records
- Aggregated linked workforce data
4. Research and innovation
- Understand and address common ICS needs and future drivers, pool data about small cohorts, use clinical and wider research to inform understanding of risk for different population groups
- Clinical trial recruitment and follow-up, disease progression and understanding, deep-learning AI, trial set-up/sizing
User types:
- National and regional analytical teams, intelligence functions, academia, VCSE and industry researchers
Access and latency
- Weekly
- Anonymised for majority of use cases
- Trial recruitment and follow up requires re-identifiable data, imperfect but timely
Data types
- Rich, linked, clinical and operational data over life course / clinical pathway
- Including genomic and patient-reported data
How does an intelligence function help with decision-making?
The intelligence function will support teams across the ICS to make better decisions through the systematic use of timely and relevant evidence. By grounding decisions in robust intelligence and data analytics that draw on wide multidisciplinary knowledge and expertise, systems can respond to a more comprehensive and detailed understanding of their populations, supporting a targeted, more effective use of resources.
The strongest intelligence functions will power innovation and decision-making at all levels of their ICS, from strategic decision-making about cross-system transformation and budget delegation, to planning care and managing operations at place level, to applying near-real time population-based insights across integrated neighbourhood teams. They will be closely linked to a wide range of stakeholders, including system and place-level leaders, operational managers and frontline staff, who will provide steer on the types of tools and analyses required to help them understand population need, set population-based budgets, and deliver proactive clinical and operational working.
In addition to responding to the needs of decision-makers, the intelligence function may also drive cross-system priorities, producing analyses and evidence that identify areas of opportunity for senior leaders and professional staff to consider. As capabilities improve, intelligence functions will begin to enable the co-ordination of care across systems, places and neighbourhood teams by supporting operational workflow management between different care providers.
Population health management
One key purpose of intelligence functions is to support a PHM approach to care, including by developing a detailed understanding of the local population’s health and care needs, such as granular intelligence on inequalities across different population groups. This will be powered by a person-level, linked data set, which can grow to include information about the wider determinants of health to support ICSs increasingly take a bio-psycho-social approach to understanding need and redesigning care models.
The intelligence function can support place-level leaders to tackle health inequalities in their area by operationally targeting areas where there is greatest need of support, or where there is unwarranted variation in care quality, and by planning new service models in response to unmet need, including giving consideration to the workforce, financial and contractual enablers.
Transformation
Together with other teams in the ICS, the intelligence function can support clinical staff to proactively use analysis to drive transformation, eg in how they implement anticipatory care across integrated neighbourhood teams. Intelligence professionals and clinicians across the ICS should have access to a population health intelligence platform that performs standard analyses, such as population segmentation and risk stratification, so that care can be targeted and personalised to the greatest effect. ICSs will want to give consideration to how analytical teams from the intelligence functions can support place-based forums with insight into population need to enable the design of new preventative integrated care models.
As population health analytics develop in power, the focus is expected to grow from condition management to the use of predictive risk factors to aid early detection and the prevention of ill health. These platforms need to interface with the national federated data platform to enable learning, improvement, and innovation through the effective and meaningful use of data across national, regional, and local contexts.
Evidence base
Another key role of a high-performing intelligence function would be to drive high standards of evidence-based decision-making. In any given scenario, the desired intelligence may not always be available, and as such it would be the role of the intelligence function to advise decision-makers when their evidence is not fully fit for the specific issue at hand, ensuring that uncertainty and other limitations of data are understood and responded to accordingly, and thus helping to maintain high standards not only in the quality of intelligence but also in its application.
To realise the potential of data to drive transformation, systems may wish to consider how they can build on existing population-based, multidisciplinary intelligence work, as well as reprioritising and modernising their use of analytical resources. In many systems we have worked with, they are planning to support development of their intelligence function by growing and developing the analytical workforce, including data management teams.
Systems may want to take account of this in their digital transformation and investment plans. It will also be important for systems, regions, and national teams to support a wider culture and capability among ICS managers towards the routine use of data and intelligence in planning and decision-making.
The decision making eco-system of the intelligence function
What does a good intelligence function look like?
The table below describes the key components of an intelligence function, and how these could develop over time.
ICSs may wish to use it to assess their own development towards a maturing intelligence function.
Purpose
Emerging: Responds to pressing cross-system and place-based requirements from senior leaders, providing intelligence on pressures within the system and forecasts of population need.
Supports transformation programmes to embed principles of analytics and population health management in new care models.
Developing: Develops the means for clinicians to interrogate the data and analytically manage their population. Primarily this support will be through building a population health intelligence platform that allows clinicians to cohort their population by different risk groups and segment by psychosocial characteristics – enabling them to identify specific individuals for further follow-up.
Has a communications strategy to share its outputs and insights with system stakeholders.
Maturing: Has a developed strategy for how population health intelligence will underpin relationships between the ICB and its partners, including budget setting, based on population need. Acts as an integrator of ICS functions, through providing strategic and operational insights to shape system and place-based priorities and strategy.
Scope
Emerging: Receives a remit to inform and investigate system -wide and place-level priorities and uses intelligence to inform the population health priorities of the ICS.
Has an agreed analytical project prioritisation process for ensuring that work is high-value and will be used to maximum effect by leaders, transformation teams and clinicians.
Developing: Provides operational and actionable intelligence to front-line multi-disciplinary teams and place-based service design forums, including beginning to provide real-time analytics to inform the flow of people, and deployment of workforce and other resources across the system (ie analytics that cannot be provided by individual organisations).
Evaluation of ICS activities is agreed as part of the intelligence function’s remit.
Maturing: Hosts and delivers insights and workflows for care co-ordination centres that manage flow across an ICS.
Supports the development and sharing of insights with research partners, such as academia.
Governance
Emerging: Representation from analytical leaders across the ICS within formal governance. Established analytical lead for each ICS (or, where appropriate, for each place).
Clear governance into the ICB and ICP – where both have a steering, oversight and listening role (and, where appropriate, governance will link into place-based forums).
Single information governance framework across system partners, with an agreed way of sharing information for PHM.
Developing: Intelligence function run and chaired by a chief analytical officer or an equivalent.
A clear governance link to the ICB board. The intelligence function has a remit to bring issues to the ICB or ICP for discussion where appropriate.
A single roles-based access definition for the linked health and care data infrastructure, describing who can use what data and tools, and how parties are responsible for stewarding the data.
Maturing: Active sponsorship from a board-level representative, such as a chief information officer, that ensures the intelligence function’s routine input into executive discussions.
Data and analysis
Emerging: Linked data available on the whole population from primary and secondary care, including mental health and community services. Data accessible to intelligence function analysts.
Analysis segmented, where possible, by ethnicity, deprivation, and other characteristics relevant to the Core20PLUS5 categories.
Intelligence function connected into the regional analytical team to ensure that the local data infrastructure and functionality coheres with the national offer and is consistent with national standards.
Developing: Data accessible to system partners through a population health intelligence platform and provides opportunities for automation and bespoke analysis.
Linked data set includes adult social care.
Analysis is produced that is replicable, with code shared across ICS partner organisations.
Incorporating wider analytical skills of evaluation and qualitative analysis.
Wider sources of evidence included in analyses, such as engagement activities, user feedback, clinical audits and insight from VCSE partners.
Most data segmented by ethnicity and deprivation. Some data available on inclusion health groups.
Maturing: Population health intelligence platform has advanced analytical techniques built-in to allow for sophisticated predictive modelling of population need, utilisation and cost over time and the impact of interventions, including dynamic modelling of risk.
Linked data set incorporates data on wider determinants of health, such as information about housing and employment.
Analytical outputs are routinely informed by mixed methods approaches, including citizen and workforce feedback and other qualitative data, for example from citizen apps and surveys.
All key data segmented by ethnicity and deprivation. Good data available on inclusion health groups.
Scale
Emerging: Consideration of the analytical support needed at system, place and PCN levels.
Establishment of links between ICSs within a region and/or across regional boundaries.
Developing: Clear operating model for how the intelligence function works at system and place-level to respond to the needs of both geographies.
Analysts embedded in each place (where appropriate) and providing insights aligned to sub-ICS geographies, building on their relationships with those who work closely with these communities.
Established model for regional collaboration, including cross-regional forums, which responds to non-alignment with local authority boundaries and considers strategic benefits of shared investment.
Maturing: Regional analysis and benchmarking to support ICSs to understand flow across their borders.
Multi-disciplinary teams
Emerging: Dedicated analytical resource identified in the ICB for addressing strategic challenges.
Clear collaborative working arrangements with a wide range of ICB teams, including transformation, finance, workforce and quality improvement.
Representation from a wide range of ICS partners, including NHS provider analysts and intelligence professionals from public health and other local authority teams.
Developing: Moving towards a federated model of working with multi-disciplinary service redesign and improvement teams at place and/or system level, which incorporate expertise on analysis, transformation, and finance, as well as clinicians and others needed to improve population health.
The intelligence function brings in a wider range of skills, such as evaluation and qualitative research and analysis.
Maturing: Intelligence function works with patient experience professionals and community engagement colleagues to ensure that qualitative and quantitative insights about the population are informing the interpretation of other analyses and are given equal weight in decision-making about targeted service improvements.
Resourcing and development
Emerging: Supported by a dedicated intelligence programme team to support the function’s governance and ensure cross-system engagement.
Mapping of system analytical workforce to identify capability gaps in delivering IF purpose and scope. This could use or build on skills mapping undertaken by the local knowledge and intelligence service (LKIS).
System partners agree a resource plan for the hosting, funding and delivery of the intelligence function, including support from digital teams.
Developing: Resource allocated from ICB and ICS partner teams for collaborative projects (alongside ICB analyst time).
Investment in skills development for analysts across a range of capabilities, including population health analytics, programming languages and data visualisation.
Strategy for developing the local analytical workforce in response to resource and capability gaps regarding advanced analytics, eg data science or modelling skills.
Dedicated analytical capacity provided by NHS providers
Maturing: Sustained investment in the intelligence function to provide resource and capability to deliver opportunities for using advanced analytics to minimise inequalities and drive health improvements and care efficiencies.
Evaluation of the impact of the intelligence function and its impact on ICS decision quality.
Useful resources
- Intelligence function toolkit
- ICS functions and governance – ICS guidance – Integrated Care (future.nhs.uk)
- ICS National Data Platform (single point of access for analytical tools – see Appendix 1)
- Population Health Intelligence Platform model specification (expected mid 2023)
- Population and Person Insight (PaPI) dashboard
- Population and Person Insight FutureNHS
- Model Health System
- National Federated Data Platform (initiation from late 2022/early 2023 – see Appendix 2 for details)
- PHM Academy
- HEE e-learning for healthcare PHM modules
- AnalystX workspace, including:
- Building strong integrated care systems everywhere: guidance on the ICS people function
- National Data Guardian – GOV.UK (www.gov.uk)
The System Workforce Improvement Model (SWIM) is a framework intended to support ICSs with development and improvement on People and Workforce areas, from planning to delivery of care. It is designed to support ICSs to assess their capacity and capability and identify support needs in establishing their people function. It is voluntary and not part of any formal oversight process.
Appendix 1: ICS analytical tools
Users can access the following tools via the ICS National Data Platform landing page of the NHS Data Platform, to which more tools will be added as they are built.
Model Health System
- Model Health System is a free data-driven improvement tool with data on activity, theatre productivity, diagnostics, workforce, medicines optimisation and more
- Population based data presented in MHS includes risk factors, disease prevalence, primary care, medicines, diagnostics, waiting times, outpatient/A&E/inpatient activity and patient outcomes.
- Information is available at various different organisational levels (Provider, sub-ICB, ICB and region with hospital site and clinical network level in development)
- Functionality includes benchmarking (with national, regional and demographic/provider peer comparisons), time-series, SPC and funnel plot charts.
Population and Person Insight dashboard
- The PaPI dashboard has been developed using nationally available linked person and event level datasets including secondary, emergency care, community services and specialised services data; grouping patients into segments based on common healthcare needs.
- Understanding the population by cohorts of those with similar health and care needs is integral to a more person-focussed health system.
- It provides a starting point for population health management approaches, to work with local areas, refine their models with their local intelligence and benchmark emerging opportunities.
- Data can be viewed through several lenses; from national right through to PCNs.
ICS place tool
- The tool will allow users to build a Place, or multiple Places, within an ICS’s geography.
- This will enable users to explore and visualise data and metrics relevant to health and care.
- Example, map asthma incidence versus deprivation in a PCN; enable PCN to determine where to deploy their resources to reduce health access inequity and achieve PCN level targets.
Health Inequalities Improvement dashboard
- Engages leaders across the system leaders to focus on inequalities reduction.
- Supports with both strategic planning and decision making and
- Operational planning to take action to reduce inequalities.
- Monitors programme impacts such as:
- CORE20PLUS5
- Digital exclusion
- Dataset coding completeness
- Restoration of service activity and waiting list
Anticipatory care dashboard
- The Anticipatory Care Planning Dashboard (ACPD) is a tool that helps Integrated Care Systems understand the size and demographic breakdown of cohorts to determine which of these cohorts could benefit most from receiving anticipatory care.
- Data-driven approaches have been used within the dashboard to support systems in identifying target populations for further prioritisation.
Primary Care Data and Insights dashboard
- Brings together a wide range of data and indicators relevant to primary care services and contractor groups, generating insight to support primary care improvement and transformation, and to inform strategic decision making at all levels of the system;
- Currently includes data relating to the national manifesto commitments for primary care and some health, equity, and population demographic views;
- Ongoing development will introduce:
- GP workforce recruitment and retention schemes
- patient satisfaction
- staff health and wellbeing
- community pharmacy
- dentistry.
NHS Performance Overview
- Supports ICBs in strategic planning across the quadruple aim of healthcare
- Presents key management information held by NHSE across as many areas as possible (acute, primary care, mental health, discharge, capacity)
- Provides one consistent dataset that can be used by all parts of the system
- Presents up-to-date information that is updated automatically
- Supports preparation for Board reporting
- Currently live with onward beta testing in August 2022.
Appendix 2: Federated Data Platform
Every day, NHS staff and clinicians are delivering care in new and innovative ways, achieving better outcomes for patients and driving efficiency. Scaling and sharing these innovations across the health and care system in England is a key challenge for the NHS.
That is why NHS England is investing in a data platform to support health and care organisations to make the most of the information they hold and to work together to understand patterns, solve problems and plan services for their local populations. Ultimately, the goal is to help the NHS transform the health and care of the people it serves.
A ‘data platform’ refers to software which will enable NHS organisations to bring together operational data – currently stored in separate systems – to support staff to access the information they need in one safe and secure environment.
A ‘federated’ data platform means that every hospital trust and integrated care system (ICS) will have their own platform but they are able to connect and share information between them where this is helpful. For example, to discharge a patient from hospital into a care setting (when the appropriate data sharing agreements are in place).
A digitised, connected NHS can deliver services more effectively and efficiently, with people at the centre.
Better outcomes and experience for people
A more efficient NHS ultimately means a better service for patients, reduced waiting times and more timely treatment. The platform will provide ICSs the insights they need to understand the current and future needs of their populations so they can tailor early preventative interventions and target health and care support. Patients will have more flexibility and choice about how and where they access services and receive care, helping them to stay healthy for longer.
Better experience for staff
NHS staff will be able to access the information they need in one secure place. This reduces the time they spend chasing referrals, scheduling appointments, and waiting for test results and allows them to work more flexibly to deliver high quality care for their patients.
A federated data platform will provide trusts and ICSs with a set of core capabilities and nationally developed solutions. Initially, these solutions will focus on supporting five key NHS priorities:
- Elective recovery – to address the backlog of people waiting for appointments or treatments which has resulted from the COVID-19 pandemic alongside Winter pressures on the NHS.
- Vaccination and immunisation – to continue to support the vaccination and immunisation of vulnerable people whilst ensuring fair and equal access and uptake across different communities.
- Population health management – to help integrated care systems proactively plan services that meet the needs of their population.
- Care coordination – to enable the effective coordination of care between local health and care organisations and services, reducing the number of long stays in hospital.
- Supply chain management – to help the NHS put resources where they are need most and buy smarter so that we get the best value for money.
Future national use cases will go through an extensive process of identification and prioritisation, in line with the principles of data minimisation as set out in the UK General Data Protection Regulation (GDPR).
A federated data platform will also provide trusts and ICSs with the capability to develop their own digital tools that address their most pressing operational challenges and enhance their ability to make informed and effective decisions.
Driving adoption
We understand the importance of investing in deployment and adoption alongside application development. The FDP will build upon existing infrastructure within ICSs. There will be no gaps in service provision during transition and mobilisation.
We have developed a set of four integration patterns ranging from a common data connection data pipeline to full adoption of the FDP. We expect all Trusts or ICS to fall into one of these integration patterns, dependant on use case. We will be engaging with ICSs early 2023 to understand their pattern.
The adoption approach takes account of the individual differences in digital maturity of each ICS and their ability to achieve common standards:
- Each ICS will be required to achieve common standards in data reporting and connectivity but can achieve these through a variety of different solutions.
- Tailoring the implementation to different adoption patterns allows a flexible and adaptable approach for each ICS no matter their current stage of digital development.
- ICSs will be provided with equitable access to key capabilities/ services to achieve connectivity.
- In all patterns NHS England will be providing core data sets and national activity and reference data.
- Through alignment with the shared care programme NHS England will ensure there is a common standard for data integration.