Organisation objective
- NHS Long Term Plan
Working with people and communities:
What approaches have been used to ensure people and communities have informed this programme of work?
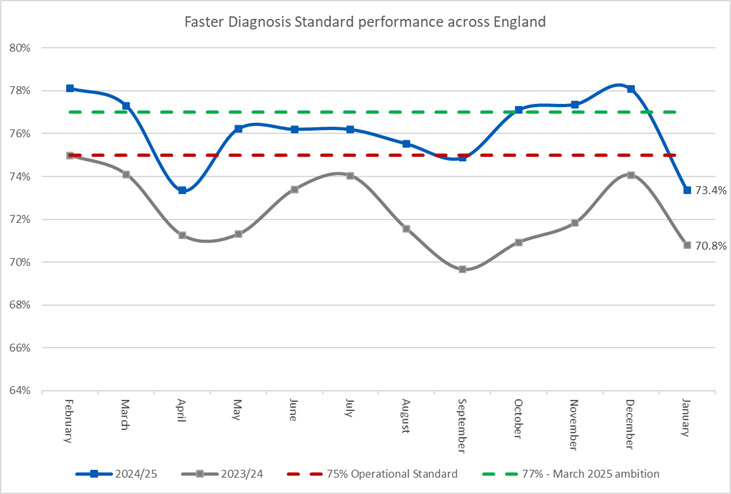
- recruited patient and public voice (PPV) partners
- consultation/engagement
- qualitative data and insight, for example, national surveys; complaints
- quantitative data and insight, for example national surveys
- partnership working with voluntary, community and social enterprise organisation
The NHS Cancer Programme has a permanent patient and public voice (PPV) forum, from which patient representatives are nominated by cancer alliances to provide input into each of our major programmes. Alliances routinely engage with people and communities to ensure that service provision is designed with the voice of people at the heart and inform how they are working with trust/systems partners, people and communities to improve experiences of cancer care across the cancer pathway.
New programmes and proposals go through our PPV forum for comment and scrutiny, and the chair of our PPV forum sits on the National Cancer Board as a full member.
The Cancer Programme also uses a range of quantitative and qualitative sources of data and information to inform our programmes. The cancer patient experience survey (CPES) and U16 CPES provide valuable insights into the issues facing patients. Our regular charity forum meetings give the voluntary sector and patient organisations the opportunity to scrutinise and feed into our work, and we make specific partnerships on areas of shared interest such as the promotion of lung cancer screening.
Action required
The Board is asked to:
- note the information provided in the report
- note the progress made on operational performance and programme delivery
Background/issue and context
1. The Long Term Plan set out stretching objectives to improve cancer survival. The primary focus of efforts to improve survival has been to increase the percentage of cancers diagnosed early when it is more likely to be treated successfully. This shift towards earlier diagnosis, and the community and home-based testing nature of these programmes are in line with the vision of the government to deliver shifts from both ‘treatment to prevention’ and ‘hospital to community’.
2. Overall early diagnosis of cancer has increased by 2.8% points since 2019 to its current level of 58.7%, including a 1%-point improvement in the 12 months to October 2024. This is the first improvement in early diagnosis in a decade, recognised in Lord Darzi’s report as one of the areas where the NHS is making progress. This progress is largely due to the successful implementation of the programme of work targeting earlier diagnosis, particularly lung cancer screening.
3. In February, the Secretary of State launched a consultation exercise to support the development of a new cancer plan, with patients, clinicians, charities and the wider public invited to submit their views. The new plan will be completed following the publication of the 10 Year Health Plan this summer.
Latest operational performance for cancer
4. Improving operational performance for cancer against the access standards in the NHS Constitution remains a priority for the National Cancer Programme. By March 2025, national targets were set to reach 77% performance on the 28-day Faster Diagnosis Standard (FDS) and 70% performance on the 62-day referral to treatment waiting time standard. We have made excellent progress and are confident of meeting these goals, with performance against the 62-day referral to treatment standard rising to 69.6% in Q3 2024/25, an improvement year-on-year of 4.6% points. Performance against the FDS, which supports a diagnosis or ruling out of cancer within 28 days, improved to 77.5% in Q3, a year-on-year improvement of 5.3% points. Whilst there remains more to do to fully recover performance, this represents real and sustained improvement for the first time since the standards were last met in 2015.
Figure 1: Faster Diagnosis Standard performance across England in 2023/24 and 2024/25
5. The core of our performance improvement approach has been ‘tiering’, providing targeted intervention and support to the most challenged providers. Tiering has continued to deliver results. For performance against the 62-day standard, in the most challenged providers (those in ‘tier 1’ in Q1 2024/25) there was an 8.6% point improvement between Q3 2023/24 and Q3 2024/25, compared to just 3.7% in non-tiered providers. The approach has also reduced the variation across the country, with the system-level performance interquartile range reducing from 8.4% in Q3 2023/24 to 6.6% in Q3 2024/25.
6. We have also seen benefits from the implementation of key pathway changes. 41% of skin cancer referrals in Q3 2024/25 used a teledermatology approach in which high quality images are reviewed remotely and most patients can be reassured and discharged. Seasonal variation on the skin cancer pathway has reduced from an around 10% drop in FDS performance through 2023 to under 5% through 2024.
7. The implementation of faecal immunochemical testing (FIT) into the bowel cancer pathway has now reached our target of 80% of referrals being accompanied by a FIT result. This enables effective risk stratification of referrals and has supported an improvement in bowel cancer diagnostic performance from 51% to 64.4% between Q3 2022/23 and Q3 2024/25. We continue to explore other opportunities to maximise the benefits offered by FIT, including the potential to combine the results with a blood test and other basic information like age and sex to provide a much more accurate risk score and avoid even more unnecessary colonoscopies.
8. Further pathway changes are at an earlier stage but are already demonstrating results. Cancer alliances have been focused on addressing performance in the most challenged providers for gynaecology, breast and urology pathways. This includes the implementation of specific pathways for women who experience unscheduled bleeding after starting hormone replacement therapy (HRT) and specific pathways for women with breast pain only and no other symptoms, both of which are often referred onto cancer pathways but are extremely unlikely to have any significant pathology. Recent work has suggested that this could apply to as many as 40% of referrals to gynaecological cancer pathways. Although there is more to do on these pathways, FDS performance is improving more rapidly than baseline performance for other pathways, with year-on-year improvement of 4.8% points, 7.2% points and 3.2% points on the gynaecology, urology and breast pathways, respectively.
Delivery of key programmes
9. The Lung Cancer Screening Programme has continued to expand rapidly in 2024/25, with an estimated 995,000 people invited to the programme. Approximately 37% of the eligible population have now been invited, over 2.6 million people in total since 2019. The programme has diagnosed over 6,000 lung cancers, more than 75% at an early stage. As a result, the early diagnosis rate for lung cancer has increased by 9.7% points compared to 2019, with an improvement of 4.6% points in just the last year. The programme has also disproportionately benefitted those with the greatest need, with those in the most deprived quintile now amongst the most likely to receive an early diagnosis.
10. People with Jewish ancestry have a higher risk of carrying BRCA mutations, the key cause of hereditary breast cancer. As part of the ‘Jewish BRCA’ programme, over 26,000 testing kits have now been distributed, with nearly 300 BRCA carriers identified so far – people who can now have either preventative treatment or more intensive screening.
11. The Community Liver Health Check Programme has carried out over 45,000 fibroscans on people at high risk of significant liver disease, going well beyond our target for the year of 30,000, with around 3,000 people identified as being at high enough risk of cancer to require regular ongoing surveillance.
12. Alongside our survival and performance goals, the programme has continued to work successfully with providers to improve patient experience and support. The latest iteration of our Cancer Improvement Collaborative was an exemplar of how NHS England can use its convening power to bring providers together to address a shared challenge, with 15 providers from across the country working together to focus on improving administration and patient communication in cancer care. The projects will continue to run until May 2025.
Continuing to innovate
13. Building on our targeted, proactive approach to early diagnosis, we have completed a pilot of primary-care based case finding for people who may have serious liver disease. This pilot has leveraged the data we already have in primary care to identify 13,000 people to receive an initial test, with 300 of those eventually referred onto surveillance pathways for hepatocellular carcinoma. The programme is currently being evaluated with a view to potential expansion, whilst a similar programme focused on pancreatic cancer symptoms will begin early in 2025/26.
14. The Cancer Vaccine Launch Pad (CVLP) was established in 2023 to support the rapid development of clinical trials of new vaccine technology aiming to create personalised treatments for cancer in partnership with industry and to spread access to these trials to patients across the country. Since being established, 55 CVLP sites have screened 3,125 patients, resulting in 432 eligible patients being referred to the clinical trial. 60% of patients in England undergoing colorectal surgery now have access to the trial. The CVLP is now looking to onboard further cancer vaccine trials in other areas, seeking to widen its impact and make the NHS in England an engine of growth for the cutting edge UK life sciences sector.
Next steps and the new cancer plan
15. The next phase of work for the NHS Cancer Programme will be determined by the outcome of the work to develop the new cancer plan, which is being jointly led by NHS England and the Department of Health and Social Care. The plan is likely to continue to have a strong focus on earlier diagnosis as key to deliver the government’s mission to reduce lives lost to the biggest killers, and as a driver of the ‘3 shifts’ from treatment to prevention, hospital to community and analogue to digital.
16. The NHS Cancer Programme will remain focused on the delivery of core programmes, building on the successes delivered through our national strategy to date and working with and through cancer alliances to take the Lung Cancer Screening Programme to a further 1.2 million people in 2025/26, continuing to improve performance against the 62-day standard to 75% and the Faster Diagnosis Standard to 80% by March 2026, and to continue to develop our most impactful and innovative programmes such as the Cancer Vaccine Launch Pad to more patients.
Publication reference: Public Board paper (BM/25(11(Pu))

