Models of care and measurement: consultation response
Classification: Official
Publication reference: PRN00654_i
August 2023
Foreword
In June 2018, the Prime Minister asked for a clinically-led review of NHS access standards to ensure they measure what matters most, both in optimising clinical outcomes and to patients.
Modernising cancer waiting times standards and refocusing performance measures on the critical NHS Long Term Plan objective of earlier and faster diagnosis, will help to ensure that we are always incentivising and holding the NHS accountable for delivering the best patient care. It will also facilitate a more intuitive understanding of the expectations a patient should have of their cancer care.
This report sets out the wide-ranging support received through the national consultation on the proposed new standards for cancer care, and highlights some of the key considerations raised to support their successful implementation. It also sets out the final policy recommendations, and the next steps required by both the NHS and Government to implement them.
The proposed new standards align with the recommendations in the 2015 Independent Cancer Taskforce report, build on the NHS Long Term Plan and prior to consultation were subject to testing across cancer providers.
We are confident that the proposals will stimulate clinical improvements to the way services are delivered and improve the experience for patients.
- Professor Sir Stephen Powis, National Medical Director
- Dame Cally Palmer, National Cancer Director NHS England
- Prof Peter Johnson, National Clinical Director for Cancer
Introduction
- In June 2018 the Prime Minister asked the National Medical Director of NHS England and NHS Improvement to review the core NHS access standards for cancer in the context of the NHS Long Term Plan, to ensure that they measure what matters most clinically and to patients. The review focused on changes to ensure cancer waiting times standards reflect current clinical and operational models of care. The standards also constitute a commitment from the NHS to people with a suspected or diagnosed cancer, and therefore must be easily understood both by patients and the clinical teams caring for them.
- Currently, nine access standards cover a range of treatment and referral routes for cancer. This is more than for all other elective care and can be complex and difficult to understand for both patients and NHS staff. The goal of the review has been to develop a new, simplified set of patient-centred standards appropriate to modern cancer care that are understandable both clinically and to the public.
- In March 2022, we published the recommendations for consultation. The consultation paper set out the proposed new standards, the rationale for the changes, and the evidence collected in support of those proposals. In parallel, a draft of the Cancer Waiting Times guidance version 12 was made available for comment, updated to include changes to the recording of patient pathways reflecting the proposed changes to the standards to promote the appropriate clinical management of patients. The final version of the Cancer Waiting Times Guidance v12 which responds to the feedback received through that process is published alongside this document.
- This document summarises the responses to the consultation and next steps.
Background to proposals
- The current set of Cancer Waiting Times standards has built up over time, and has not been reviewed in the round for almost ten years. In their 2015 report, the Independent Cancer Taskforce recognised that the current Two-Week Wait standard does not measure the most meaningful metric to the patient: the time they wait to receive a diagnosis or have cancer ruled out, and recommended its replacement with a new 28 day Faster Diagnosis Standard, but did not consider changes to the other Cancer Waiting Times standards.
- The 2WW standard was introduced 20 years ago as one of the first of the new wave of NHS targets. The standard only requires hospitals to provide an appointment to ‘stop the clock’ – regardless of whether that appointment is of value for the patient. Whilst this made sense in 2000, many pathways can now go ‘straight to test’, without the need for an outpatient appointment. We have heard from clinicians that some patients can be brought in for an appointment, just to ‘stop the clock’ when the best approach clinically and for the patient should be a ‘straight to test’ pathway for a diagnostic such as a colonoscopy.
- The separate 31-day and 62-day standards have evolved over that same 20 year period, with each new standard bringing additional cohorts into the Cancer Waiting Times system. Although performance is currently challenged, performance monitoring and management of these cohorts is now very well established, and the set of performance standards would benefit from simplification and harmonisation of expectations between, for example, those patients diagnosed via a screening service and those diagnosed because they had symptoms of possible cancer.
- In an interim report for this review, it was proposed to replace the three standards related to treatment starting within 62 days for urgent referrals, consultant upgrades and screening with one standard; and replace the four standards related to first and subsequent treatments within 31 days from diagnosis with one 31-day treatment standard. All patients covered by the current standards are captured by the scope of the new standards. Combining the 62 day and 31 day standards will ensure that expectation of rapid diagnosis and treatment applies equally to patients regardless of the route they take into their pathway, or the type of treatment they are receiving. That interim report also reiterated the recommendation to replace the Two Week Wait standard with the 28 Day Faster Diagnosis Standard.
- Following publication of the interim report, we engaged with stakeholders in June 2019, and received responses from 46 organisations, including hospitals, Cancer Alliances and charities across the country. Responses overall supported the core proposals. Support for the immediate removal of the 2WW standard was more mixed, with some asking whether the time taken to first appointment should be lengthened or whether there may be knock-on impacts on 62-day performance. This area was therefore chosen for focus during field testing.
- 12 sites were identified for testing, reflecting experience across a mix of rural and urban communities across the country including higher and lower performers with an appropriate level of data quality. A further 16 organisations were selected to act as a control group. Testing began in September 2019. No significant issues or concerns were raised by either the clinical or patient groups involved in the test sites, data from the test sites demonstrated that patients are not waiting significantly longer for first appointment than previously and performance against FDS and 62- day standards were shown to be unaffected or better in test groups than control groups. Feedback from test sites indicates that services can quickly flex their models to provide a diagnosis or rule out cancer more quickly and can adopt innovative solutions to manage increased demand without being disincentivised through the 2WW standard rules. Staff feedback supported the introduction of the new cancer access standards; they were perceived to be more patient-focused. This feedback did also identify key potential challenges for their implementation by trusts related to administration, due to increased tracking of patients who have cancer ruled out.
- It is also proposed to remove the reference within the Cancer Waiting Times guidance to the 31-day referral to treatment period for Urgent GP (GMP, GDP or Optometrist) referrals for acute leukaemia, testicular cancer, and children’s cancers. No separate performance standard currently exists for these patients and reporting of these patients within the numerator and denominator of the 62-day all cancer National Statistics published by NHS England will continue.
- The final set of standards proposed and which were consulted on are:
- Faster diagnosis standard: Maximum 28-day wait to communication of definitive cancer/not cancer diagnosis for patients referred urgently (including those with breast symptoms) and from NHS cancer screening.
- Maximum two-month (62-day) wait to first treatment from urgent GP referral (including for breast symptoms) and NHS cancer screening.
- Maximum one-month (31-day) wait from decision to treat to any cancer treatment for all cancer patients.
Consultation approach and questions
- Between 6 March and 6 April 2022 we publicly consulted on the proposals to seek the views of patients, the public and key stakeholders.
- In this we requested feedback on the simplification of the current standards, and a move from the 2WW for a first appointment to the confirmation or not of cancer within 28 days measured by the FDS. People across the country were asked to submit their views in the following ways:
- online consultation survey
- through email and letter correspondence.
- NHS England promoted the consultation online and through a press release.
- The NHS Cancer Programme individually engaged key organisational stakeholders including the Association of Breast Surgeons, Cancer Research UK, Breast Cancer Now, Cancer 52, and Macmillan immediately ahead of the consultation period.
- This report presents the findings on the questions set out for engagement with the public and wider NHS.
- An updated draft of the Cancer Waiting Times guidance version 12 was published for comment alongside the consultation, comments received have not been included in this response but will be considered in the final drafting of this document.
Engagement questions and proposed measures
- We sought responses to the following questions based on the current and proposed standards:
- Current Standards:
- Are you aware of the current cancer standards?
- What do you understand the two-week wait first seen standard to mean?
- What do you understand the 31-day first treatment standard to mean?
- What do you understand the 62-day referral to treatment standard to mean?
- Recommended standards
- To what extent do you agree or disagree with the proposal to replace the expectation of an appointment within two weeks with people receiving a definitive diagnosis or ruling out of cancer within 28 days of referral?
- To what extent do you agree or disagree with the proposal to simplify the existing referral to treatment standards by combining them into one 62-day standard?
- To what extent do you agree or disagree with the proposal to simplify the existing decision to treat to treatment standards by combined them into one 31-day standard?
- Respondents were asked to quantify the extent to which they agreed or disagreed on a scale from 1 strongly disagree to 5 strongly agree and for each question on the recommended standards were asked to explain their reasoning.
Consultation responses
Respondents
- We received 283 responses to the online survey, and 22 pieces of correspondence (letters and emails) were received. We analysed all responses received through these routes, against the relevant questions.
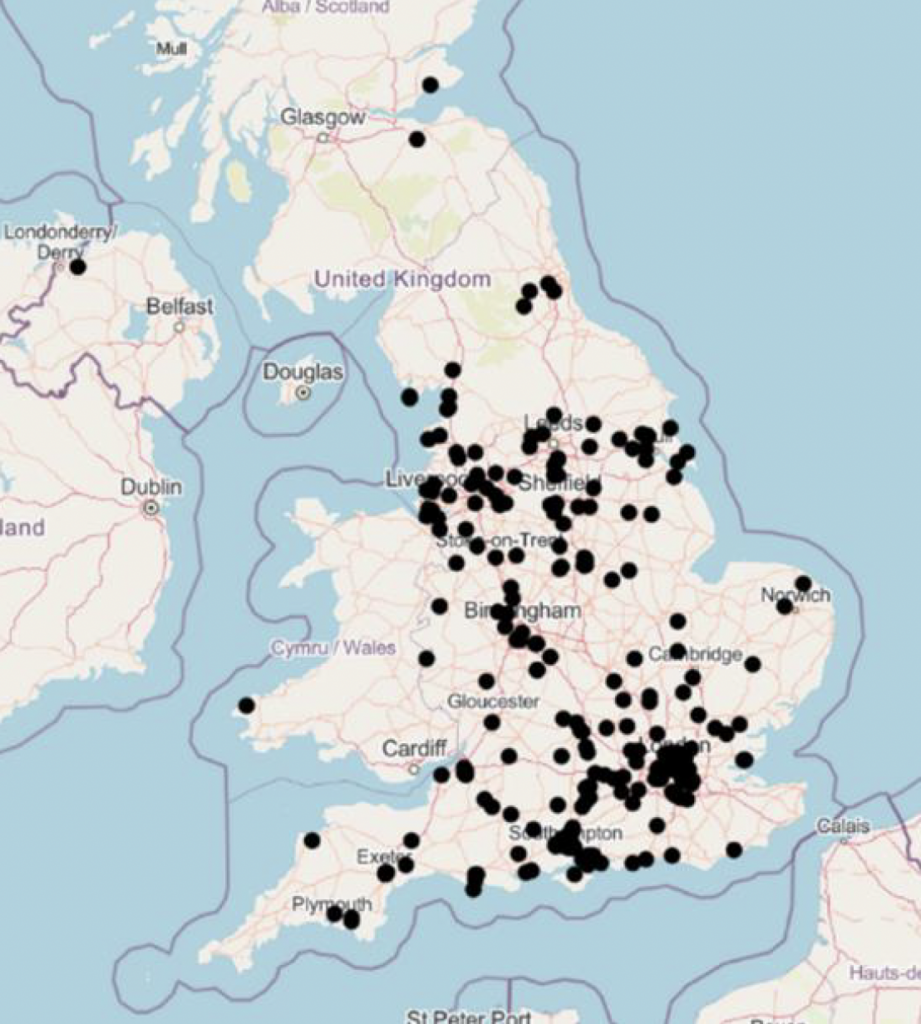
- No respondents declined to state if they were responding as an individual or on behalf of an organisation. Participants were not required to answer every question, and some provided personal views on the importance of timely access to appropriate care rather than specific views on the recommendations. Analysis of the respondents postcodes and organisational responses show that we received engagement and views from a range of public, voluntary and independent sector organisations across health, local government and wider social care and across England.
- 85% (240) of online survey respondents identified themselves as responding as an individual compared to 15% (43) providing a formal organisational response. Of the former, 83 (35%) identified themselves as either a patient or member of the public (see Table 1), and 118 (49%) as an NHS employee. 19 (56%) of the organisational responses were on behalf of an NHS organisation (see Table 2).
Table 1: As an individual responding to this survey, which of the following best applies to you?
| Respondent category | Number | Percentage |
|---|---|---|
| NHS employee | 118 | 50% |
| Patient | 87 | 37% |
| Member of the public | 26 | 11% |
| From a health-related group, charity or organisation | 5 | 2% |
| From another public sector organisation | 2 | 1% |
| Total | 238 | n/a |
Table 2: As an organisation responding to this survey which of the following best applies to you?
| Respondent category | Number | Percentage |
|---|---|---|
| Formal response on behalf of an NHS organisation | 24 | 56% |
| Formal response on behalf of a health-related group, charity or organisation | 19 | 44% |
| Total | 43 | n/a |
33. Via correspondence we received 22 responses across NHS organisations, NHS Staff, professional organisations, patient representative organisations and private companies. This breadth of responses – from health professionals, representatives of local government, education professionals, as well as charities and patient representative bodies – provides a consistent message on what is important clinically, operationally and, importantly, to patients and the public.
What the consultation responses said
34. 82% of respondents indicated they were aware of current Cancer Waiting Times standards and were asked what their understanding of the existing Two Week Wait, 31 day and 62 day standards means. 83% of respondents gave a definition of the Two Week Wait standard in line with the current Cancer Waiting Times guidance, with 73% doing so for the 31 day standard. Understanding of the 62 day standard was less clear, with 57% giving a definition of the standard as set out in guidance. 9 of the 22 pieces of correspondence gave definitions of the current standards, all of which were in line with guidance. Broadly speaking, therefore, the cohort of respondents had a reasonable understanding of the current Cancer Waiting Times standards.
35. Overall, 65% (183) agreed with the proposal to replace the expectation of an appointment within two weeks with the proposal that people receive a definitive diagnosis or ruling out of cancer within 28 days of referral. Just 8% strongly disagreed. Figure 2 shows the proportions of responses. Organisations were more likely to agree with the proposal than individuals (81% compared to 62%):
| Respondent view | Percentage |
|---|---|
| Strongly agree | 37% |
| Agree | 28% |
| Neither agree nor disagree | 13% |
| Disagree | 15% |
| Strongly disagree | 8% |
Figure 2 – To what extent do you agree with the proposal to replace the expectation of an appointment within two weeks with the proposal that people receive a definitive diagnosis or ruling out of cancer within 28 days of referral? Base: 281
- When asked to comment further on their response on replacing the Two Week Wait with the Faster Diagnosis Standard (FDS) the top three themes raised were:
- 71 respondents (29%) in agreeing with the proposal felt it would support quicker diagnosis.
- 37 respondents (15%) made observations that different cancers require different time frames (e.g. different pathways).
- 27 respondents (11%) in agreeing with the proposal felt that the 28-day standard is clear and realistic (e.g. gives a clear time frame for patients and clinicians).
- When analysing top themes by respondent type those in agreement felt that the proposal will support quicker diagnosis and that the 28-day standard is clear and realistic. Only one theme of disagreement was noted, from the patient/public group, that 28 days is too long to wait for a definitive diagnosis or ruling out of cancer (12 respondents). Of the correspondence on replacing the Two Week Wait with FDS, 22 themes in agreement were raised. Those in agreement felt the proposal will support quicker diagnosis, improves monitoring and reporting, improves quality of diagnosis, and improves service efficiency. Of those in disagreement, the most common related to concerns that the current 75% FDS threshold was too low. Observations from both the formal respondents and the correspondence included the need to ensure appropriate resources to implement the proposal and to consider that different cancers require different time frames (e.g. different pathways).
41. On the proposal to simplify the existing referral to treatment standards into a combined 62-day standard, overall, 54% (149) agreed and 21% (58) disagreed with 26% neutral. Just 10% strongly disagreed (Figure 3):
| Respondent view | Percentage |
|---|---|
| Strongly agree | 26% |
| Agree | 28% |
| Neither agree nor disagree | 26% |
| Disagree | 11% |
| Strongly disagree | 10% |
Figure 3 – To what extent do you agree or disagree with the proposal to simplify the existing referral to treatment standards into a combined 62-day standard? Base: 278
- Organisations were more likely to agree with the proposal than individuals (78% compared to 50%). When analysing by stakeholder type, NHS / public sector organisation respondents, employees and formal voluntary / charity sector respondents agreed (90%, 64% and 68%) with this proposal more.
- When asked to comment further on their response on the proposed combined 62 day standard the top three themes raised were:
- 35 respondents (17%) in agreeing with the proposal felt that it simplifies the process (e.g. makes it faster).
- 32 respondents (16) in disagreeing with the proposal felt 62 days is too long to wait for a patient with suspected cancer.
- 31 respondents (15%) in agreeing with the proposal felt the 62-day standard sets a clear expectation for patients and clinicians (e.g. easy to understand).
- Of the correspondence on the proposed combined 62 day standard, 18 themes in agreement were raised, with 11 in disagreement. Those in agreement felt that the proposal simplifies monitoring and reporting, supports equal access for treatment of all cancer patients and sets a clear expectation for patients and clinicians (e.g. easy to understand). Of those in disagreement, the most common related to concerns that the proposed performance threshold was unknown.
- 48. On the proposal to simplify the existing decision to treat to treatment standards into a combined 31-day standard, overall, 59% (162) agreed and 12% (32) disagreed with 30% neutral (Figure 4).
| Respondent view | Percentage |
|---|---|
| Strongly agree | 26% |
| Agree | 33% |
| Neither agree nor disagree | 30% |
| Disagree | 7% |
| Strongly disagree | 4% |
Figure 4 – To what extent do you agree or disagree with the proposal to simplify the existing decision to treat to treatment standards into a combined 31-day standard? Base: 276
- Organisations were more likely to agree with the proposal than individuals (78% compared to 50%). When analysing by stakeholder type, NHS / public sector organisation and voluntary / charity sector respondents (84% and 81%) showed stronger agreement than patients, members of the public and NHS employees (50% and 58%).
- When asked to comment further on their response on the proposed combined 31 day standard the top themes raised were:
- 25 (15%) respondents reflected agreement with the proposed standard.
- 25 respondents (15%) in agreeing with the proposal felt the combined 31-day standard simplifies the process.
- 21 respondents (12%) in agreeing with the proposal felt it improves access to diagnosis and treatment (e.g. faster).
- 11 respondents (7%) each made observations that that different cancers require different time frames (e.g. different pathway) and to ensure there are appropriate resources to implement the proposal.
- Of the correspondence on the proposed combined 31 day standard, 10 themes in agreement were raised, including that the proposal simplifies monitoring and reporting. with 5 single instances of disagreement. Themes from the correspondence included appropriate monitoring and reporting of the standard (e.g. disaggregated by cancer type), the need for clear guidance about new standards (e.g. clear definitions) and that different cancers require different time frames for diagnosis.
Response to themes raised in the consultation
- Some respondents and correspondents raised concerns that the Faster Diagnosis Standard threshold of 75% is too low. It has always been our intention to increase the threshold from the initial 75% at the appropriate time. At the present time, NHS action is focused on delivering the commitments on recovery from the pandemic, including ensuring achievement of the 75% standard by March 2024, as set out in the Delivery plan for tackling the COVID-19 backlog of elective care. However, we do feel that the time is now right to set out the future trajectory to raising the standard. As part of the announcement of the final policy, we have therefore set out our intention to raise the Faster Diagnosis Standard to 80% by the end of the 2025/26 financial year.
- Some respondents raised the length of waiting times standards. Waiting times standards are relatively narrow instruments, designed to provide a measure suitable for capturing a minimum expectation which will be deliverable for the vast majority of patients. Whilst we should always strive for the fastest possible accurate and safe diagnosis, the 28 day Faster Diagnosis Standard and the 62 day standard are considered by most clinicians to be a clinically appropriate timeframe for almost all cancers to be diagnosed and treated.
- Many patients with suspected cancer are diagnosed or ruled out considerably more quickly than the headline 28 days captured in the standard, with over 40% of people having their cancer diagnosed or ruled out within 14 days. Similarly, for some cancers such as acute leukaemias, cancers are usually treated within days, rather than weeks or months. A target of 85% of people beginning treatment within 62 days does not suggest that these timeframes should or will slow down.
- We will continue to publish Cancer Waiting Times data in distinct time bands to demonstrate that a significant proportion of patients wait considerably less time than the maximum timeframes of the standards stipulate, for example 0-14 and 14-28 days for the FDS, and propose to highlight these faster breakdowns more frequently to aid understanding of the standards and performance against them.
- Respondents made a number of helpful observations on how best the proposals could be introduced to maximise benefits to patients and the NHS. Common themes included:
- ensuring appropriate monitoring and reporting of the standards (e.g. disaggregate by source of referral, suspected cancer type)
- consider that different cancers require different time frames, but whilst under the theme of equality, supporting equal access for treatment of all cancer patients
- ensuring appropriate resources to implement the proposals
- We propose to address the first two of these through a series of changes to the monthly and quarterly Cancer Waiting Times data publication, to ensure complete clarity over performance by source of referral, suspected cancer referral type and widening the range of different diagnosed cancer types a specific breakdown is provided for. Specifically, we plan in future to publish 62 day and 31 day performance individually for Lung, Breast, Skin, Lower GI, Prostate, Other Urological, Lymphoma, Other haematological, OG, Hepatobiliary, Head and Neck, Gynaecological and ‘All Other’ cancers. However, we do not propose introducing different waiting times standards for different cancer types – the standards are set to represent all cancer types and clinical scenarios, and it is expected that some cancer types should consistently deliver shorter waiting times than others, and that this will be reflected in overall performance.
- Some feedback that proposed performance thresholds were unknown, particularly for the 62 day standard, may explain the relatively high proportion of respondents who neither agreed nor disagreed with the proposals for the 62 day and 31 day standards. To incorporate the responses that standardisation and equality across cancer types matter, we propose to retain the performance thresholds of 85% for the 62 day standard (currently this threshold applies only to those referred by a GP) and 96% for the 31 day standard (currently this threshold applies to those receiving their first treatment).
Next steps
- The feedback we received strongly supports changing the Cancer Waiting Times standards in line with the recommendations, whilst underlining the importance of introducing change in a clear and structured way.
- We therefore have had approval from government to implement the following standards for Cancer Waiting Times, replacing all current Cancer Waiting Times standards from 1 October 2023:
- Faster Diagnosis Standard: Maximum 28-day wait to communication of definitive cancer / not cancer diagnosis for patients referred urgently (including those with breast symptoms) and from NHS cancer screening. Performance threshold: 75%
- Faster Diagnosis Standard: Maximum two-month (62-day) wait to first treatment from urgent GP referral (including for breast symptoms), NHS cancer screening and Consultant Upgrade. Performance threshold 85%
- Faster Diagnosis Standard: Maximum one-month (31-day) wait from decision to treat to any cancer treatment for all cancer patients. Performance threshold 96%
- The changes proposed will require amendments to the official statistics publications for Cancer Waiting Times, for which a separate consultation will be carried out as required by guidance relating to Official Statistics. This will also include the proposed changes to tumour level granularity.
- Delivery of the Cancer Waiting Times standards forms part of the NHS Standard Contract and the handbook to the NHS constitution. The Two Week Wait standard is also included in the NHS Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012, which the Government has agreed it will formally amend in due course. Required changes to the handbook to the NHS constitution will be made by DHSC prior to 1st October and the standard contract will be updated at the earliest opportunity. A clear and explicit communication to providers and commissioners on expectations for delivery of Cancer Waiting Times against the new standards will be issued.
67. A new version of Cancer Waiting Times guidance, version 12, will come into force on 1 October and is published alongside this document.
Annex A: Background and demographics of those responding to the online survey
Ethnicity
| Ethnicity | Number of people | Percentage |
|---|---|---|
| White: British | 209 | 79% |
| White: Irish | 3 | 1% |
| White: Gypsy or traveller | 0 | 0% |
| White: Other | 0 | 0% |
| Mixed: White and Black Caribbean | 1 | 0.4% |
| Mixed: White and Black African | 0 | 0% |
| Mixed: White and Asian | 2 | 1% |
| Mixed: Other | 0 | 0% |
| Asian/Asian British: Indian | 17 | 6% |
| Asian/Asian British: Pakistani | 1 | 0.4% |
| Asian/Asian British: Bangladeshi | 0 | 0% |
| Asian/Asian British: Chinese | 0 | 0% |
| Asian/Asian British: Other | 1 | 0.4% |
| Black/Black British: African | 0 | 0% |
| Black/Black British: Caribbean | 0 | 0% |
| Black/Black British: Other | 0 | 0% |
| Other ethnic group: Arab | 1 | 0.4% |
| Any other ethnic group | 2 | 1% |
| Base | 266 |
Sexual orientation
| Sexuality | Number of people | Percentage |
|---|---|---|
| Heterosexual | 217 | 83% |
| Lesbian | 7 | 3% |
| Gay | 3 | 1% |
| Bisexual | 2 | 1% |
| Other | 0 | 0% |
| Prefer not to say | 32 | 12% |
| Base | 261 |
Relationship status
| Status | Number of people | Percentage |
|---|---|---|
| Married | 179 | 68% |
| Civil partnership | 4 | 2% |
| Single | 24 | 9% |
| Divorced | 9 | 3% |
| Lives with partner | 16 | 6% |
| Separated | 0 | 0% |
| Widowed | 7 | 3% |
| Other | 1 | 0.4% |
| Prefer not to say | 22 | 8% |
| Base | 262 |
Age category
| Age | Number of people | Percentage |
|---|---|---|
| 16 – 19 | 0 | 0% |
| 20 – 24 | 3 | 1% |
| 25 – 29 | 2 | 1% |
| 30 – 34 | 12 | 5% |
| 35 – 39 | 23 | 9% |
| 40 – 44 | 16 | 6% |
| 45 – 49 | 32 | 12% |
| 50 – 54 | 39 | 15% |
| 55 – 59 | 39 | 15% |
| 60 – 64 | 30 | 11% |
| 65 – 69 | 22 | 8% |
| 70 – 74 | 20 | 8% |
| 75 – 79 | 11 | 4% |
| 80 and over | 10 | 4% |
| Prefer not to say | 7 | 3% |
| Base | 266 |
Religion
| Religion | Number of people | Percentage |
|---|---|---|
| No religion | 94 | 36% |
| Christian | 121 | 46% |
| Buddhist | – | – |
| Hindu | 9 | 3% |
| Jewish | 5 | 3% |
| Muslim | 6 | 2% |
| Sikh | 1 | 0.4% |
| Any other religion | 4 | 2% |
| Prefer not to say | 23 | 9% |
| Base | 263 | n/a |
Sex
| Sex | Number of people | Percentage |
|---|---|---|
| Male | 87 | 33% |
| Female | 161 | 62% |
| Intersex | – | – |
| Prefer not to say | 13 | 5% |
| Other | – | – |
| Base | 261 | n/a |
Pregnant currently
| Pregnancy status | Number of people | Percentage |
|---|---|---|
| Yes | 1 | 0.4% |
| No | 237 | 93% |
| Prefer not to say | 17 | 7% |
| Base | 255 |
Recently given birth
| Recent birth status | Number of people | Percentage |
|---|---|---|
| Yes | – | – |
| No | 241 | 94% |
| Prefer not to say | 16 | 6% |
| Base | 257 | n/a |
Health problem or disability
| Level of limitation | Number of people | Percentage |
|---|---|---|
| Yes, limited a lot | 30 | 12% |
| Yes, limited a little | 45 | 17% |
| No | 185 | 71% |
| Prefer not to say | – | – |
| Base | 260 | n/a |
Disability
| Disability | Number of people | Percentage |
|---|---|---|
| Physical disability | 27 | 10% |
| Sensory disability | 6 | 2% |
| Mental health need | 5 | 2% |
| Learning disability or difficulty | 2 | 1% |
| Long-term illness | 41 | 16% |
| Other | 4 | 2% |
| Prefer not to say | 12 | 5% |
| Base | 264 |
Carer
| Carer category | Number of people | Percentage |
|---|---|---|
| Yes – young person(s) aged under 24 | 39 | 15% |
| Yes – adult(s) aged 25 to 49 | 7 | 3% |
| Yes – person(s) aged over 50 years | 29 | 11% |
| No | 181 | 69% |
| Prefer not to say | 12 | 5% |
| Base | 263 | n/a |
Gender reassignment
| Gender reassignment | Number of people | Percentage |
|---|---|---|
| Yes* | 5 | 2% |
| No | 226 | 90% |
| Prefer not to say | 19 | 8% |
| Base | 250 | n/a |
*Have you gone through any part of a process or do you intend to (including thoughts and actions) to bring your physical sex appearance and/or your gender role more in line with your gender identity? (This could include changing your name, your appearance and the way you dress, taking hormones or having gender confirming surgery)
Armed services
| Armed services member | Number of people | Percentage |
|---|---|---|
| Yes | 19 | 7% |
| No | 232 | 88% |
| Prefer not to say | 12 | 5% |
| Base | 263 | n/a |
NHS England Wellington House 133-155 Waterloo Road London
SE1 8UG
© NHS England 2023
Publication reference number: PRN00654_i

