Background
King’s College NHS Foundation Trust identified delays in their vetting of complex scans and patient follow-ups, a lack of standardisation between vetting radiographers and radiologists, and adverse incidents occurring from scans not being performed in the correct time frame. The team engaged in an improvement project to tackle these issues, and their improvement process is shared in this case study.
Benefits seen at King’s College NHS Foundation Trust
- significant improvements were seen in the request to appointment turnaround time
- the number of scans vetted per day by the assigned radiographer increased in excess of 20%
- there are consistently less than 0.5% DM01 CT breaches monthly
The steps to implement a radiology information system vetting module
1. Stakeholder mapping
- identify all stakeholders involved in the improvement project
- this includes administrative teams who will have workflow adjustments, vetting radiographers, sub-speciality radiologists, and the business intelligence unit
2. Implement the vetting module on the radiology information system provider
- this ensures that all protocol descriptions are standardised in language and terminology for scanning radiographers, reducing ambiguity
- review the vetting protocol to ensure all the necessary information is captured at time of vetting, such as the estimated glomerular filtration rate (eGFR) and the surveillance scan date
- the dedicated vetting module significantly improves the productivity of the number of scans vetted
3. Develop a standard operating procedure
- develop a standard operating procedure for the vetting radiographer to standardise practice amongst colleagues
- the standard operating procedure should set out the expectations of the role, key contacts, awareness of cancer and operational targets, and escalation pathways to keep patients within pathway timeframes
4. Identify workstreams
- identify and implement the necessary workstreams – these were:
- completed – for administrators to book
- on hold – awaiting further information, eg eGFR result, clinical information
- referred to radiologist – justification is required by a radiologist to proceed, eg the clinical details do not meet the radiographer authorisation protocols
5. Create a role for a vetting radiographer
- dedicate a daily rostered vetting radiographer in a separate environment away from the scanning control room with a dual monitor display to ensure task focus and high productivity
- create a shared email inbox and provide a dedicated phone line to improve continuity of management for patients
6. Set up a daily checklist
- design a checklist for the vetting radiographer to sign off daily
- the daily tasks list was designed and ordered by priority from what was being frequently missed or forgotten, leading to breached targets
7. Training for all stakeholders
- following the above changes, ensure all identified stakeholders receive the appropriate training to adhere to the new processes
- take feedback from staff to understand how the changes are working in practice and adjust the processes accordingly
8. Methodical deep dive
- ensure waiting list patients are scrutinised weekly and that an automatic dashboard is set up to visualise the waiting list data
- all patients waiting over 3 weeks to be booked had a superintendent review
- ensure that the weekly interrogation of data is reviewed proactively, allowing sufficient lead time to accommodate patients before breach date
Overcoming Challenges at Kings College NHS Foundation Trust
Challenge: workstreams not being checked
Radiologists were not always reviewing the ‘referred to radiologist’ workstream, meaning that these patients were delayed.
Solution: combine workstreams and email reminders to avoid patients being missed
Patients are still added to the ‘referred to radiologist’ workstream so the vetting radiographer is aware to follow up.
Additionally, radiologists are also emailed directly for a protocol to ensure no delay in the pathway.
Challenge: low compliance rate
Some radiologists had a low compliance rate for using the vetting module.
Solution: ensure all staff are appropriately trained
Further training was needed after the go live date, to ensure all stakeholders understood the workflow changes and the associated benefits.
Challenge: data discrepancies
Administrative teams were requested to book directly from the ‘vetting completed’ list, but this led to data capture discrepancies in the business intelligence unit.
Solution: involve business intelligence colleagues in the project
Work with the business intelligence unit to understand and resolve these discrepancies moving forwards.
Figure 1: driver diagram: reducing radiology appointing DM01 delays
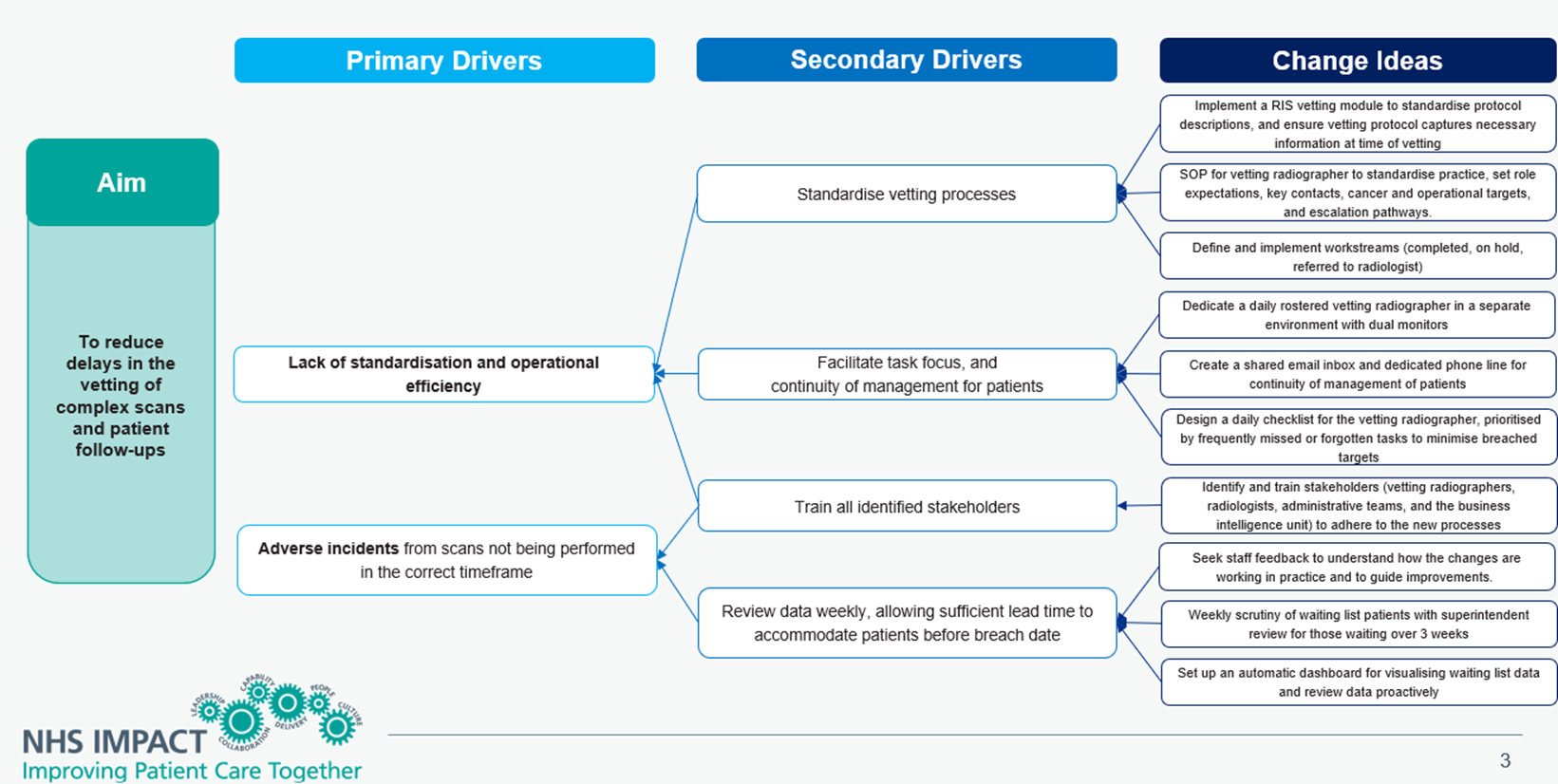
Figure 1: reducing radiology appointing DM01 delays driver diagram- click to view accessible text version of this diagram.
Reading from left to right
Aim:
To reduce delays in the vetting of complex scans and patient follow-ups.
Primary drivers:
- lack of standardisation and operational efficiency
- adverse incidents from scans not being performed in the correct timeframe
Secondary drivers:
- standardise vetting processes
- facilitate task focus, and continuity of management for patients
- train all identified stakeholders
- review data weekly, allowing sufficient lead time to accommodate patients before breach date
Change ideas:
- implement a RIS vetting module to standardise protocol descriptions, and ensure vetting protocol captures necessary information at time of vetting
- standard operating procedure for vetting radiographer to standardise practice, set role expectations, key contacts, cancer and operational targets, and escalation pathways
- define and implement workstreams (completed, on hold, referred to radiologist)
- dedicate a daily rostered vetting radiographer in a separate environment with dual monitors
- create a shared email inbox and dedicated phone line for continuity of management of patients
- design a daily checklist for the vetting radiographer, prioritised by frequently missed or forgotten tasks to minimise breached targets
- identify and train stakeholders (vetting radiographers, radiologists, administrative teams, and the business intelligence unit) to adhere to the new processes
- seek staff feedback to understand how the changes are working in practice and to guide improvements
- weekly scrutiny of waiting list patients with superintendent review for those waiting over 3 weeks
- set up an automatic dashboard for visualising waiting list data and review data proactively
Links and resources
- conducting a stakeholder analysis, section 3.1 of The handbook of quality and service improvement tools
- to speak to someone at King’s College about this project, please contact the Radiology team at kch-tr.radiographersuperintendents@nhs.net
- Further resources on diagnostics can be found on the National Diagnostics Transformation FutureNHS page. An NHS email address will be required to access the page
Publication reference: PRN01007

