Background
Turnaround time is often used as a key performance indicator in pathology, and as a quality marker of the service. Turnaround times are often a challenge where capacity, volume and staffing requirements may be exceeded. A key challenge is the overuse of urgent requests, which results in:
- blocked flow from emergency departments
- additional pressure on ward and laboratory staff
- a high volume of phone calls from those chasing results
- genuinely urgent requests being delayed
Dr Emily Leach at the Eastern Pathology Alliance recently embarked on a project to review turnaround time challenges, and this case study shares the learning more widely.
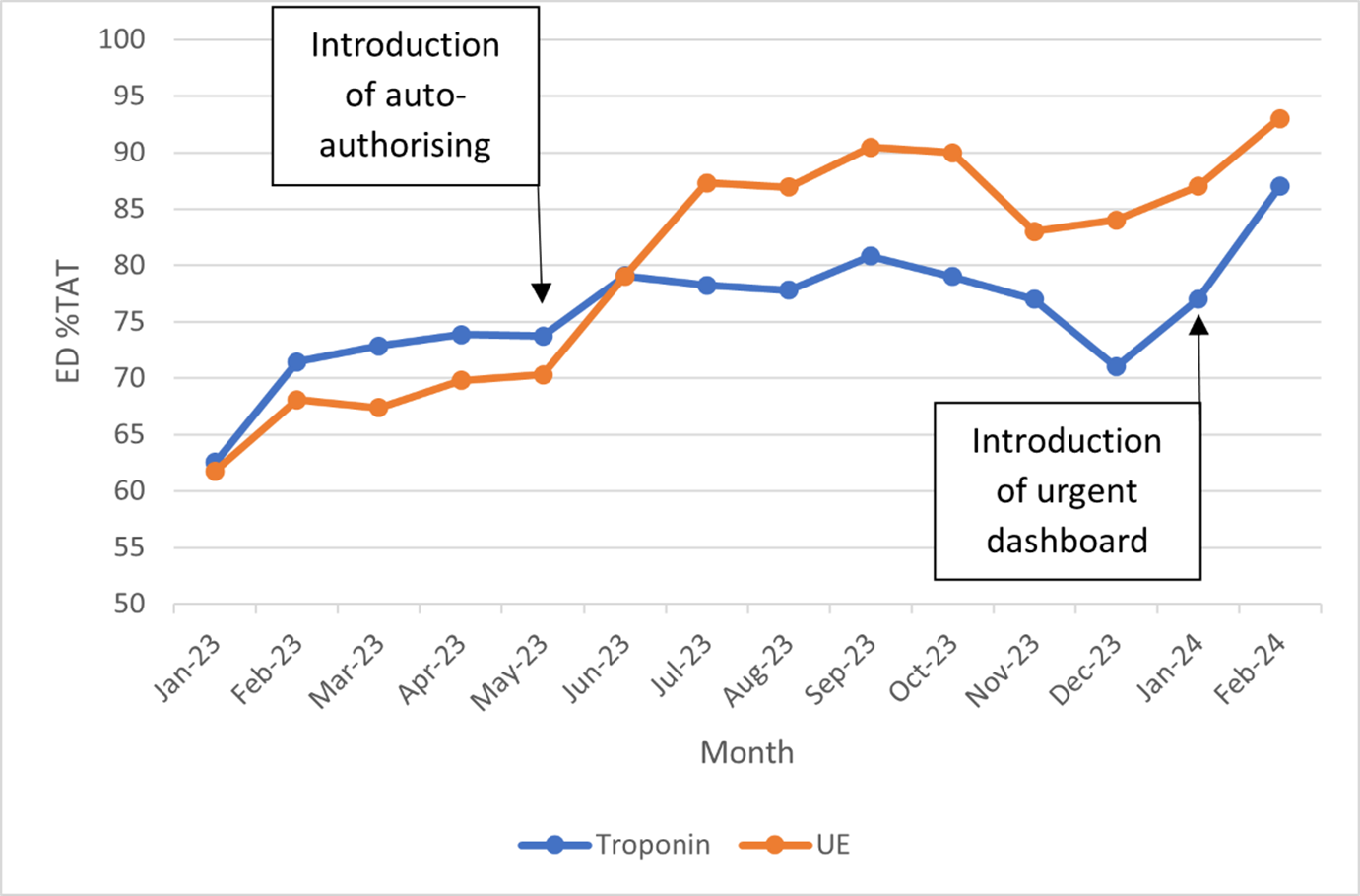
Figure 1: Run chart showing the percentage of emergency department requests achieving their turnaround time target when using troponin and urea and electrolyte as a benchmark
This chart shows that after introducing the auto-authorisation of results, and an urgent test dashboard, the percentage of tests achieving their turnaround time target has increased.
Benefits seen at the Eastern Pathology Alliance
- improvements were seen in both urea and electrolyte and troponin tests used as a benchmark to determine turnaround time (see figure 1)
- auto-authorisation was implemented on all biochemistry tests in a stepwise approach
- the development of a dashboard showing urgent tests highlights patients due to breach within 30 minutes, allowing staff to direct their time where it is most needed
- laboratory staff now understand the importance of their role in improving turnaround times, and how it is linked to the patient pathway.
The steps to improve turnaround time
1. Review your current impacts on turnaround time
- process map your current flows:
- how long does it take to analyse the sample?
- can you apply a complexity score to the analysis?
- are there any pre-analytical, analytical, or post-analytical issues that may impact the integrity of the result?
2. Create appropriate priority queues
- create priority queues to stream work, allowing staff to focus on the most time critical tests first
- at the Eastern Pathology Alliance, the queues used are:
- priority 1 – urgent and emergency department requests (including urgent requests from any area)
- priority 2 – inpatient requests
- priority 3 – GP and outpatient requests
3. Review tests marked as urgent
- consider your local definition of urgent, and what urgent doesn’t include.
- routine urgent locations are often the emergency department, the intensive care unit, and the neonatal intensive care unit
- other urgent requests tend to come from discharge, theatre, maternity, and for rapidly deteriorating patients
- review the appropriateness of allocated turnaround times – could you re-assign tests to a different flow?
4. Restrict access to urgent tests
- at the point of request – educate the requester on the impact of submitting an urgent request
- managing requests at point of request could reduce patients being unnecessarily bled. It also manages the requesting clinician’s expectations
- at the point of receipt – support laboratory staff to decline inappropriate urgent requests
5. Use technology to automate the process
- review all assays and their ‘normal’ ranges
- apply a delta check using a principle reference change value to ensure safe clinical auto-authorising
- the reference change value is a combination of biological and analytical variation
- the laboratory information management system can apply this reference change value to the reference range, authorising results without the need for human intervention
- as a result of auto-authorisation, staff only see the results that require clinical attention, streamlining their workload to only what is needed
6. Create a data dashboard
- work with your business intelligence team to create a dashboard to monitor urgent requests
- urea and electrolyte and troponin test sets were used as a benchmark to determine the turnaround time
- highlighting patients close to breaching enables you to clearly see what tests need to be prioritised
- the dashboard is constantly displayed and reviewed by staff, who use a data driven approach to prioritisation
7. Staff education
- engage with all staff, from specimen reception through to laboratory staff, keeping them informed of the process from concept through to completion
- provide suitable training, competency and instructional documentation
- train staff to have an understanding of auto-authorisation and delta check rules, showing them how it enhances result review
- maintain a fluid approach, amending the process to ensure safety and making it work for the staff
Overcoming challenges at the Eastern Pathology Alliance
Challenge: laboratory staff’s view of their role
Laboratory staff did not always understand their role in the patient pathway, and the impact that inappropriate turnaround times could have on the patient.
Solution: educate laboratory staff
Work with laboratory colleagues to educate them on the importance of quick turnaround times, both for the patient and the laboratory.
Challenge: restricting urgent tests
When everyone is under pressure and wants their result quickly, it is difficult to change their behaviour and restrict access to urgent tests.
Solution: communicate with external colleagues
Spread awareness of the impact of inappropriate turnaround times to external colleagues.
Challenge: resistance to change
As with any improvement project, there is a resistance to change among some colleagues.
Solution: involve stakeholders
Involve all stakeholders from the beginning of the project, listening to their feedback and develop the changes accordingly. Highlight the benefits from the change on staff and patients.
Figure 2: turnaround times in pathology driver diagram
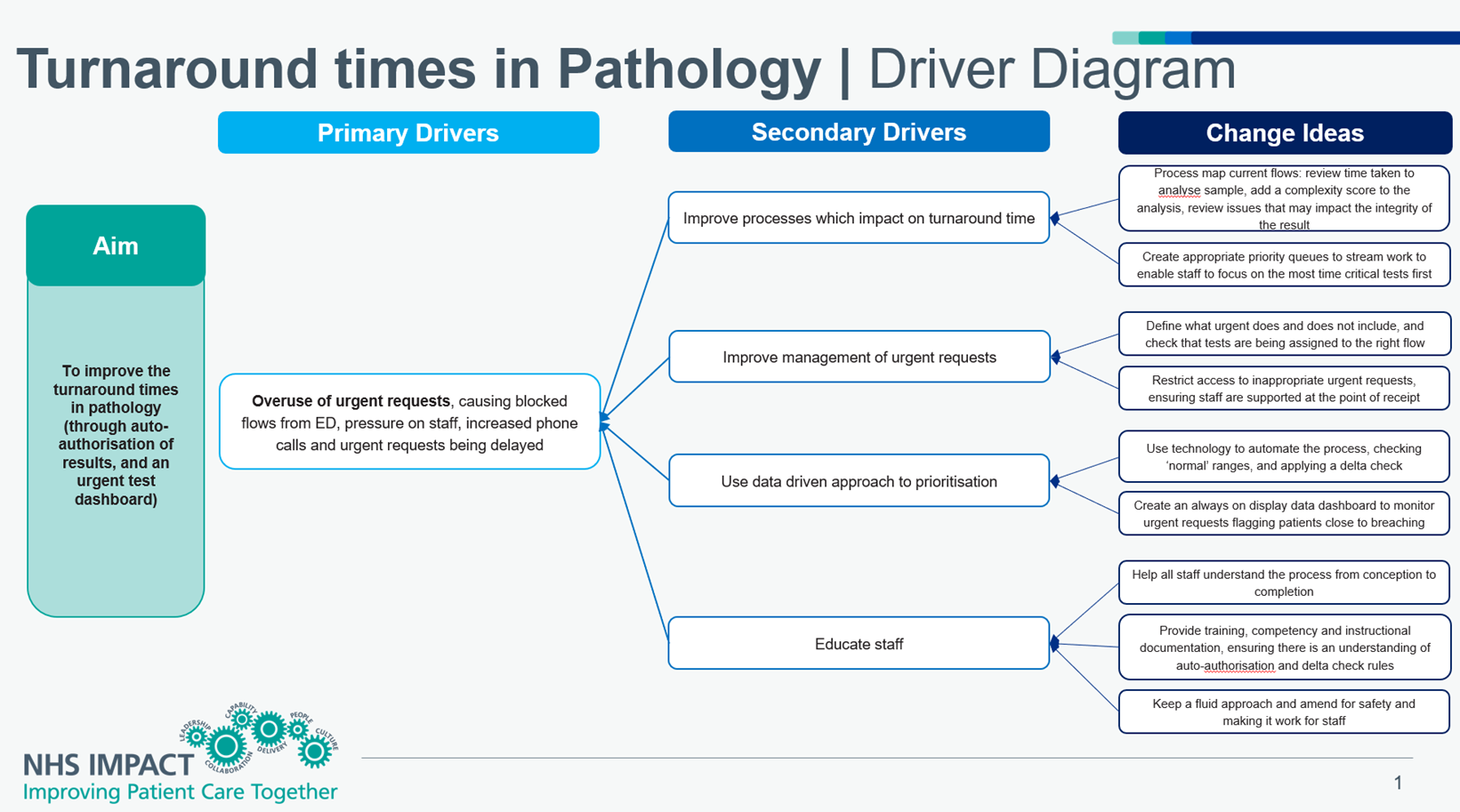
Figure 2: turnaround times in pathology driver diagram – click to view accessible text version of this diagram.
Reading from left to right
Aim: to improve the turnaround times in pathology (through auto-authorisation of results, and an urgent test dashboard).
Primary drivers: poor turnarounds times and overuse of urgent requests, causing blocked flows from emergency departments, pressure on staff, increased phone calls and urgent requests being delayed.
Secondary drivers:
- improve processes which impact on turnaround time
- improve management of urgent requests
- use data driven approach to prioritisation
- educate staff
Change ideas:
- process map current flows: review time taken to analyse sample, add a complexity score to the analysis, review issues that may impact the integrity of the result
- create appropriate priority queues to stream work to enable staff to focus on the most time critical tests first
- define what urgent does and does not include, and check that tests are being assigned to the right flow
- restrict access to inappropriate urgent requests, ensuring staff are supported at the point of receipt
- use technology to automate the process, checking ‘normal’ ranges, and applying a delta check
- create an always on display data dashboard to monitor urgent requests flagging patients close to breaching
- help all staff understand the process from conception to completion
- provide training, competency and instructional documentation, ensuring there is an understanding of auto-authorisation and delta check rules
- keep a fluid approach and amend for safety and making it work for staff
Links and resources
- to speak to colleagues at the Eastern Pathology Alliance about this project, please email LaboratoryMedicineOffice@nnuh.nhs.uk
- further resources on diagnostics can be found on the National Diagnostics Transformation FutureNHS page. An NHS email address will be required to access the page.

