Introduction
Cervical cancer leads to approximately 685 deaths a year in England and most cervical cancer cases (99.8%) are caused by the human papillomavirus (HPV) virus. By increasing equitable uptake of both HPV vaccination, which protects against most forms of the virus, and cervical screening, which checks for high-risk HPV, we can make cervical cancer a disease of the past.
On 15 November, 2023, NHS England outlined its ambition to eliminate cervical cancer by 2040, aligning with the World Health Organization’s (WHO) global initiative to achieve a below 4 per 100,000 cervical cancer incidence rate.
Eliminating cervical cancer in England is not only an important public health goal but also a crucial step toward improving women’s overall health and wellbeing. This complements the ambitions in the Department of Health and Social Care’s (DHSC) Women’s Health Strategy.
While women tend to live longer than men, they are more likely to spend their lives in ill health, which can lead to personal financial health costs. As HPV vaccination and cervical screening offers range from adolescence through to later years, we have the opportunity to improve outcomes for girls and women across their lives.
Eliminating cervical cancer is more achievable than ever before. The latest HPV vaccine type introduced in the UK in 2021 is proven to be even more effective in improving health outcomes – in the long term it is predicted to reduce cases of women’s cancer and HPV attributable deaths by 16% and 9%, compared to the previous vaccine type. Studies in England have shown that the HPV vaccine stops 90% of cervical cancer cases and can reduce incidence in low socioeconomic groups. The move from a 2 to single dose HPV vaccination offer in September 2023 should also make it easier for school-aged children and young adults to get fully vaccinated. Meanwhile, cervical screening saves approximately 5,000 lives a year through checking for the presence of high-risk HPV and early detection of abnormal cells, which if left untreated may lead to cervical cancer.
Despite the opportunities to eliminate cervical cancer, both HPV vaccination and cervical screening coverage have declined over recent years. While the latest cervical screening coverage data shows that progress is being made, inequalities in vaccination uptake and screening coverage exist among certain communities and there is variation across the country (see figures 1 and 2 below). Cervical cancer incidence rates in England are 65% higher in the most deprived quintile compared with the least. Common challenges related to accessibility and discomfort during cervical screening need to be addressed.
Figure 1: HPV vaccination coverage
The percentage of year 10 girls vaccinated by integrated care board (ICB) in August 2023, according to UK Health Security Agency data
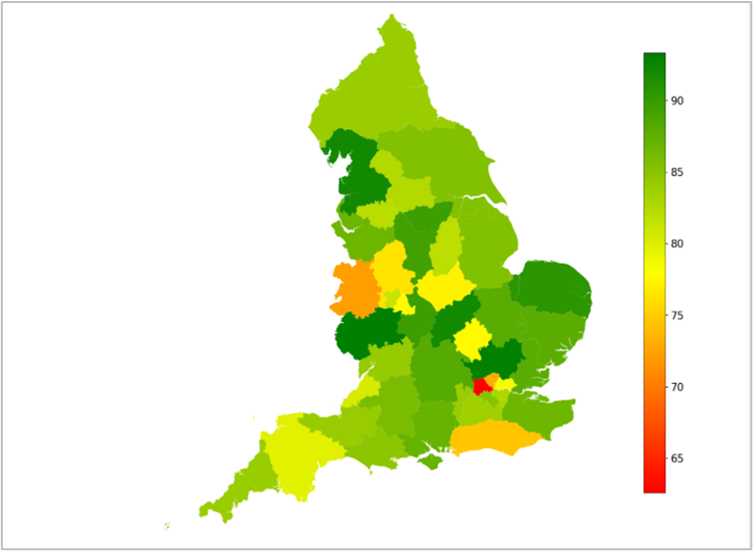
Figure 1 is a map of England showing variation in HPV coverage between ICBs, with some achieving more than 90% coverage and others below 65%.
Figure 2: Cervical screening coverage
The percentage of women aged 25 to 64 in each ICB who were covered by cervical screening at the end of March 2024, according to Cervical Screening Programme data
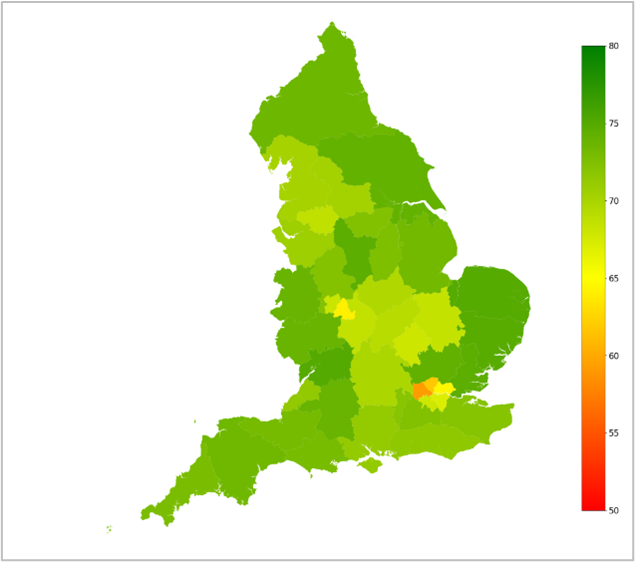
Figure 2 is a map of England showing variation in cervical screening engagement between ICBs, with some achieving more than 75% coverage and others below 65%.
This publication outlines how the NHS in England will improve equitable uptake and coverage of HPV vaccination and cervical screening, supporting progress toward the ambition to eliminate cervical cancer. This will be a long-term and collective effort across the NHS, as ICBs take on responsibility for commissioning vaccination and screening services for their populations from April 2026.
This publication has been developed following discussion with our stakeholders, including cancer charities.
Eligibility
All young people aged 12 to 13 (school year 8) are eligible for HPV vaccinations. Any young people who miss their vaccination are then eligible to receive it as part of a catch-up cohort between the ages of 14 and 25.
Cervical screening is offered to women and people with a cervix aged 25 to 64. There are people who do not identify as women, who have a cervix and are therefore at risk of developing this form of cancer so are eligible for cervical screening. These groups include trans men, non-binary and intersex people. Their specific experiences and needs will be considered in the delivery and communication of services that will help achieve cervical cancer elimination.
Where we are now?
As set out by the WHO’s global strategy for cervical cancer elimination, our ambition means reaching the following milestones:
By 2030:
- 90% of girls fully vaccinated with the HPV vaccine by the age of 15
- 70% of women screened using a high-performance test (for example, HPV primary screening test) by the age of 35 and, again, by the age of 45
- 90% of women identified with cervical disease receive treatment (meaning 90% of women with precancer are treated, and 90% of women with invasive cancer managed)
By 2040:
- cervical cancer incidence rate of below 4 per 100,000 women
Currently, progress is being made to reach these milestones, although more work needs to be done.
- HPV vaccination – In the 2023-2024 academic year, 76.7% of girls and 71.2% of boys aged 14 or 15 were vaccinated by year 10. The vaccine uptake in year 8 increased compared to the previous year (72.9% of girls and 67.7% of boys in 2023-2024, compared to 71.3% and 65.2% respectively for dose 1 in 2022-2023).
- Cervical screening – 76.9% of women aged 35 to 39 have a screening test recorded before their 35th birthday. 75.9% of women aged 40 to 44 have been screened in the previous 5 years. Data is not yet available to show that the same people screened by the age of 35 go on to be tested again before their 45th birthday, in line with the cervical cancer elimination targets. We expect that this data will be available in future through developments to the new national screening call and re-call system for invitations and reminders (Cervical Screening Management System (CSMS)).
- Pre-cancer treatment – We are looking into routinely available data to agree the appropriate measurements for this milestone.
- Cancer treatment – 88.3% of all cervical cancers received one or more forms of chemotherapy, radiotherapy and tumour removal treatment. This rose to more than 96% for cervical cancer at stages 1 to 3.*
- Incidence rate – 9 per 100,000 for women of all ages.
*The remaining 11.7% of cervical cancer cases across all stages are classified as having “other care”. This represents the group of patients who had no record of chemotherapy, tumour resection/removal, or radiotherapy in the time frame assessed. This may include patients who received other treatments (such as hormonal therapy or management of symptoms), treatment outside of the time frame assessed, treatment in a private setting, or where there is data missing from the datasets used.
Meeting the nationally-set targets and KPIs for vaccination and screening in England will also play a key role in achieving elimination, alongside maintaining a strong focus on HPV vaccination for boys and young men.
Both programmes have made changes to improve vaccination and screening rates. This includes regionally led action plans to increase HPV vaccine uptake, which are overseen by NHS England nationally, and the implementation of a new national screening call and re-call system, which will support improvement of cervical screening invitations and results. The positive impact of the HPV vaccination is also starting to be seen in reduced cervical cancer incidence rates among vaccinated women (see the reduced incidence rate in 2020 for women aged 25 – 29 in figure 3 below).
Figure 3: Cervical cancer rates by age
Comparison of cervical cancer incidence between 2010 and 2020 for 5-year age groups, according to National Disease Registration Service data (October 2024)
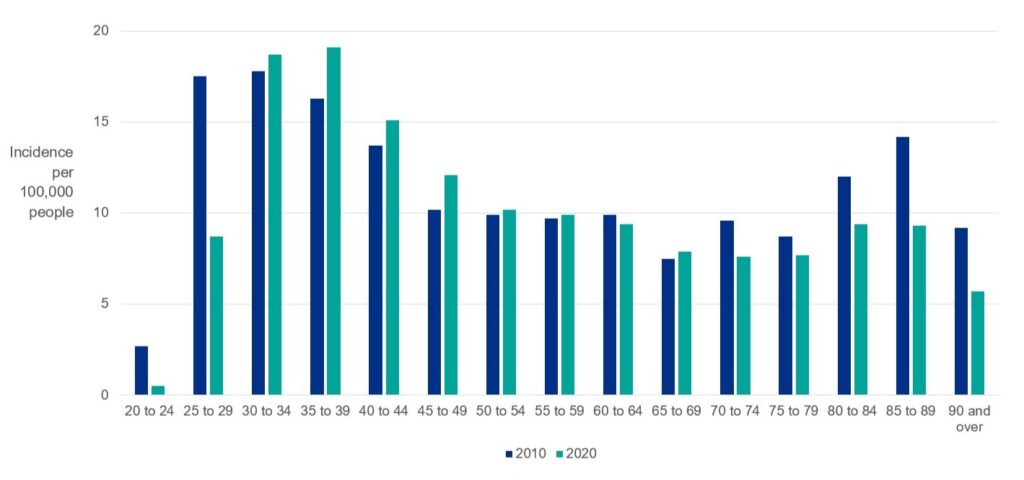
Figure 3 is a bar graph comparing cervical cancer rates for different age groups between 2010 and 2020. It shows a sharp drop for 25 to 29 year olds.
Similarly, improving earlier diagnosis of cancers, including cervical cancer, continues to be a priority for cancer services. This includes encouraging people who have noticed unusual or persistent changes in their health to contact their GP practice and making funding available to cancer alliances to encourage and support the whole system to promote early diagnosis. In the case of primary care networks (PCNs), this could include support for promoting cervical screening attendance and reviewing referral practice, which could include for cervical cancers, in line with the PCN directed enhanced service (DES).
There are other strategic aims that will support the elimination of cervical cancer through increased HPV vaccination and cervical screening coverage. This includes the NHS Vaccination Strategy (December 2023), which sets out the core components of vaccination services to help increase uptake and coverage, including for HPV vaccination. We are also developing proposals to further improve and transform screening services, including cervical screening, through streamlined commissioning arrangements and more local flexibility to improve access.
How we will get there
We will build on what is already working well to drive vaccination and screening uptake and coverage, focussing on 5 cross-cutting themes. This will involve some joint work across both vaccination and screening programmes, such as:
- communicating the combined importance of HPV vaccination and cervical screening through invitations, healthcare campaigns and workforce training – as well as other channels and materials
- identifying priority risk population groups or geographical areas, informed by vaccination and screening data, to tailor national and local initiatives. This could include populations with low HPV vaccination and low cervical screening rates and women eligible for cervical screening who haven’t received their HPV vaccination (including those who were not eligible for HPV vaccination when the offers began in 2008)
1. Increasing access
We need to ensure people can get their vaccination and screening offers at a time and place that suits them and in a way that meets individual needs. Improving access will involve maximising opportunities offered through a range of delivery settings and approaches and will include the following steps.
1. Strengthening the core offer of HPV vaccination
- The core offer for HPV vaccination is commissioned from school aged immunisation services (SAIS) providers for those up to 18 years old and is predominately offered in secondary schools (with outreach activities such as community clinics and house visits). This is supplemented with opportunistic delivery of catch-up HPV vaccinations (for those 14 to 25 years old) in general practice.
- In 2025/26 we are focusing on augmenting this core offer by:
- strengthening the contractual requirement for SAIS providers to offer catch up opportunities across all adolescent vaccinations, to maximise opportunities to vaccinate the unvaccinated cohort in various settings
- working with colleagues from DHSC and the Department for Education to unblock operational challenges encountered by SAIS teams delivering vaccinations in schools, such as data protection and data sharing issues
- co-producing public-facing materials with partners, which will include targeted messaging to encourage uptake in population groups with lower vaccination rates
2. Expanding delivery settings/locations for HPV vaccination catch-up offers
- In line with the NHS Vaccination Strategy and the delegation of vaccination services to ICBs in April 2026, we will work with partners to explore how the provider network could be expanded for certain vaccinations (including the HPV vaccination). Alternative provision may support ICBs to design and deliver local models, offering catch-up HPV vaccinations tailored to reach diverse communities.
- This could include building on the existing GP offer, improving understanding and awareness among GP teams and the public, and enabling HPV vaccination catch-up in alternative settings such as community pharmacies.
3. Introducing HPV self-sampling as an option for people who do not engage in the cervical screening programme in early 2026 (if recommended by the UK National Screening Committee (UKNSC))
- The UKNSC will shortly be considering HPV self-sampling as an option for those who do not engage in the Cervical Screening Programme. Planning is already underway to ensure that, if the UKNSC makes a recommendation and it is approved by government and funded, the NHS will be ready to implement it. Plans may include allowing tests to be ordered through the NHS App, as well as alternative options for accessing tests. We will ensure there is appropriate laboratory capacity and sufficient reporting capability to track and monitor the effectiveness of self-sampling. We will develop tailored and personalised communications for individuals, working with DHSC to apply insights from research into the self-sampling offer.
- This may encourage people who would otherwise not come forward to take up their screening offer, improve patient experience and support trauma informed care.
2. Raising awareness
Ensuring people are aware of and understand the benefits of HPV vaccination and cervical screening is crucial for informed decision making. Creating effective, nuanced and culturally sensitive health communications relies on collaborative work with 3rd sector partners and local communities.
We will raise awareness of cervical cancer prevention offers through strategic, long-term and evidence-based communications. This will include:
- taking an insight-driven approach to messaging, using commissioned research across key community groups to develop a consistent cervical cancer elimination narrative within our communication materials. These assets will be available for use across the health system, particularly school-age services and primary care, and will include personal experiences from patient advocates that bring the importance of screening and vaccination to life
- a national cervical cancer elimination campaign, encompassing both HPV vaccination and cervical screening. This will include improving understanding of HPV as a virus and how it can lead to cervical cancer, explaining the vaccination and screening offers, and co-developing sensitive messaging due to cultural concerns related to sexual activity. School-age and general practice providers will play a key role in raising awareness of vaccination and screening opportunities, and community pharmacy will also help raise cultural awareness in their local communities. Key events and awareness days will be used to amplify the campaign message, including Cervical Cancer Prevention Week, International HPV Awareness Day and the publication of annual HPV vaccine and cervical screening statistics
- collaborating with partners such as school-age providers and the Department for Education to co-deliver cervical cancer prevention webinars in schools, universities and colleges, as well as for teaching staff and vaccinators. We will engage with charities to guide the development of public information materials and with parliamentarians to make the case for the importance of vaccination and screening
- improving understanding and awareness of HPV vaccination among boys and men, aiming to reduce transmission of HPV and therefore to lower cervical cancer rates in women, while also reducing the risk of other HPV-related cancers that can impact men. This will build on existing work, such as the HPV vaccine messaging in the NHS and Asda partnership during World Head and Neck Cancer Week
3. Reducing inequalities
There are differences in vaccination and screening coverage between communities and some groups face inequalities. Cervical cancer rates are higher in more deprived populations than in more affluent groups, for example. This may reflect lower vaccination and screening rates. Developing cervical cancer depends on multiple risk factors including age, history of attending cervical screening, vaccination status (or whether vaccination was available) and smoking status.
Barriers to vaccination and screening services for underserved communities and people who experience health inequalities must continue to be addressed. This will involve:
- building our understanding of barriers to and perceptions of HPV vaccination and cervical screening from groups including school-age vaccination providers, parents or guardians of children eligible for their HPV vaccination and women due to receive their first cervical screening invite. This can be shared with local systems to support planning of culturally-sensitive, community-led engagements with low uptake groups
- continuing to develop inclusive materials to better reach underserved communities through trusted voices, working with other arms-length bodies such as the UK Health Security Agency (UKHSA) to align resources. This will include translating cervical screening information leaflets into 30 different languages and testing a pamphlet on cervical cancer elimination in a number of different languages. We will work with faith leaders and partners to ensure tailored materials are shared in the right way through the right people
- identifying groups using national and local level data who may be at higher risk of developing cervical cancer, to inform national initiatives (such as tailored screening invitations) and support local service planning. This may include women who haven’t received their HPV vaccination or women aged 50 to 64 who have not been screened recently, to encourage them to attend while they are still eligible
- enabling trans men and non-binary people with a cervix to be routinely invited for cervical screening using the new call and re-call IT system (CSMS). This enables eligible individuals with a cervix who are not registered as ‘female’ with their GP practice to be sent an invitation automatically. Tailored public communications and training for clinical and non-clinical health care staff on the needs of LGBTQ populations will support implementation
4. Improving digital capabilities
We know that people’s experiences of HPV vaccination and cervical screening can be improved through digital developments, such as streamlining parental consent for vaccination and digitising invitations and reminders for screening.
To build on this work, NHS England is:
- partnering with school-age immunisation providers to test a new digital product for school-age vaccinations (including HPV). Manage Vaccinations in Schools (MAVIS) improves the end-to-end process of delivering vaccinations. The aim is to provide clear and centralised information on the benefits of vaccinations to parents and guardians, simplify the consent process, improve efficiency of vaccination recording and release time for vaccination providers to offer more outreach for low uptake communities. This will be supported by enhanced data sharing across provider teams, such as SAIS, Child Health Information Services (CHIS) and primary care.
- maximising the best use of available patient-level HPV vaccination data through digital platforms and enhancing the quality and coverage of future data. Improving the quality of data will help commissioners design vaccination services and target interventions, using accurate, timely and granular insight. Patient-level HPV vaccination data is scheduled to be onboarded to the NHS Federated Data Platform (NHS FDP) in summer 2025. This will include 2 years of backlog data and daily data flows, giving visibility of vaccinations delivered by SAIS providers. These changes will save time and effort for providers
- developing the digital enablers required to support increased access to catch-up HPV vaccinations in alternative settings (such as community pharmacy). This includes invitations and reminders and the ability to book appointments through the NHS App and website
- developing a digital-first approach to cervical screening invitations and reminders. We will offer screening invites through the NHS App (in 2025) and other digital channels. Letters will still be used to connect with those who are digitally excluded
- developing a service in the NHS App to improve people’s vaccination journeys. It will help users see which vaccinations they are eligible for, which they’ve already had (where data is available), and how and where to access the ones they still need
5. Strengthening workforce capacity
The workforce required to deliver the cervical cancer elimination plan is diverse, spanning a wide range of skills and roles across the healthcare system. There are recognised shortages in specialist areas such as colposcopy and pathology and demand on this workforce will fluctuate due to factors such as population growth, HPV vaccination uptake, changes to screening intervals, and the introduction of self-sampling.
To ensure sufficient capacity to deliver the plan, we need to implement retention strategies and maximise the skills of existing staff. Cross-training can allow healthcare professionals to perform multiple roles, increasing flexibility and ensuring service continuity during periods of fluctuating demand. For example, nurse colposcopists could support activities within hysteroscopy, cancer management, or quality improvement.
Additionally, extending roles to oversee self-sampling (if agreed) may help optimise workforce utilisation, particularly if sample-taking in GP surgeries and sexual health clinics declines. This shift presents an opportunity to enhance HPV vaccination efforts and support broader health optimisation strategies.
To meet future demand and strengthen workforce resilience, the NHS can broaden responsibilities and training offers to ensure capacity is well-distributed. Opportunities include:
- expanding roles: exploring opportunities for a broader range of healthcare staff to support HPV vaccination delivery, thereby spreading capacity across a wider workforce
- workforce planning: developing an agile cervical screening workforce that can adapt to changes in demand and policy, particularly in response to the long-term impact of HPV vaccination on screening offers
- integrated care and digital health: promoting integrated care models, leveraging digital health solutions (such as digital pathology), and fostering patient-centred approaches to improve cancer outcomes
- education and professional development: partnering with academic institutions to integrate the latest research into ongoing training programs and ensuring access to resources such as the e-learning module on population screening or just-in-time training on self-sampling
- supporting sample-taking professionals: working with professional bodies to ensure nurses and GPs receive just-in-time training on self-sampling (if approved by the UKNSC) and trauma-informed care principles
Additionally, service planners and cervical screening programme leads must understand workforce projections to support effective decision-making. Expanding the use of nurse-led clinics and encouraging dual training in colposcopy and hysteroscopy will help mitigate the impact of screening interval changes on career pathways. These measures will create greater career opportunities while ensuring staff can support different areas of service delivery when demand fluctuates.
By proactively planning for workforce challenges and capitalising on emerging opportunities, we can ensure a well-trained, adaptable workforce that is capable of delivering high-quality cervical screening, vaccination, and cancer prevention services now and in the future.
Next steps
Achieving cervical cancer elimination is a long-term goal that depends on joined up delivery of HPV vaccination and cervical screening programmes at national, regional and ICB level.
ICBs are well placed to understand the needs of their local populations and work with partners to offer services that meet those needs. They are best positioned to plan vaccination and screening services, using the recommendations set out in the cervical cancer elimination plan.
We will continue to engage with stakeholders inside and outside the NHS to explore potential policy changes that support the goal of eliminating cervical cancer. This work will be guided by national data analysis to identify where investment can deliver the greatest improvement outcomes.
Publication reference: PRN01603

