1. Introduction
This clinical guidance supports the effective delivery of unscheduled dental care services in England, both during and outside normal working hours. It aims to support equitable access to timely, safe and effective care that is tailored to individual’s needs. It covers both in-person treatment and remote advice during initial triage.
It is designed to support the National service specification for urgent and non-urgent unscheduled dental care and replaces the Clinical standard for urgent dental care published by NHS England in November 2023. Local systems should have appropriate commissioned services, infrastructure and workforce in place to meet these needs and be able to adapt to changing national and local circumstances (such as major power failures).
It also supports the government’s manifesto commitment to deliver 700,000 additional urgent dental care appointments in 2025/26, focusing on cases triaged for treatment within 24 hour to 7 days.
Care counting toward the 700,000 additional appointments includes the treatment required to address a patient’s presenting complaint and the initial disease management of underlying risk factors, as outlined in section 6. This is defined as a single course of urgent treatment in line with the regulations.
Where a patient requires ongoing treatment (‘stabilisation’) to address their oral health needs (either a band 2 or band 3 course of treatment), this does not count toward the 700,000 appointments. Also, remote advice on self-management given during triage, before any face-to-face assessment, will also not count toward the 700,000 appointments.
The single course of urgent or unscheduled treatment should be recorded by submitting an FP17 for a band 1 urgent claim, unless alternative local arrangements are in place. Subsequent courses of treatment required to manage ongoing care needs should be recorded by submitting an FP17 for the appropriate banded course of treatment. There is no limit on how soon this ongoing treatment can begin after the patient’s unscheduled care needs have been addressed. NHS England will be amending the Dental Assurance Framework from 20 June 2025 to ensure that unscheduled care is not included in the metrics related to re-attendance within 3 months for either adults or children.
2. Principles of delivery
Unscheduled dental care should be high quality, with individuals seen at the right time, in the right place, by the right person delivering the right care. Care must be accessible to all patients – including children and adults, those with additional needs, and those not currently receiving treatment in primary dental services.
Patients must not be denied access to an available unscheduled dental care appointment where they do not have an NHS number, GP registration or current permanent address. They must also be allowed access to an available unscheduled urgent care appointment if they are not undergoing current treatment or are not known to a practice.
There should be streamlined access to unscheduled dental care, personalised support for complex needs, and a proactive approach to prevention. These principles align with the Fuller Stocktake report commissioned by NHS England.
3. Defining unscheduled dental care
3.1 Unscheduled dental care
As defined in the Management of acute dental problems guidance produced by the Scottish Dental Clinical Effectiveness Programme (SDCEP), patients requiring unscheduled dental care can be categorised into 1 of the following 3 categories:
- emergency unscheduled care (immediately life threatening and oral and dental conditions): patients who may require clinical triage by an appropriately trained clinical triage professional within 60 minutes and subsequent treatment within a timescale that is appropriate to the severity of the condition
- urgent unscheduled care: patients who may require clinical care within 24 hours or as soon as practically possible, unless the condition worsens
- non-urgent unscheduled care: patients requiring dental care within 7 days, unless the conditions worsens
Figure 1 in the appendix provides an outline of these pathways.
3.2 Emergency unscheduled care
Emergency unscheduled care, which involves life-threatening conditions, is generally not covered by this clinical guidance or the national service specification. It is included here because of its integration with the wider unscheduled dental care system. It may need to be considered for provision under a different pathway.
However, some emergency care treatments (life-threatening oral and dental conditions listed below) may be appropriately provided, under the care covered by this guidance, based on clinical need and with patient safety as the priority. Providers should be prepared to consider undertaking emergency unscheduled dental treatment where dental teams are sufficiently skilled and competent to do so. This will need to be considered on a case-by-case basis (for example, cases of permanent tooth avulsion where reimplantation within 60 minutes is strongly advised or managing spreading dental infection where timely intervention is critical). This will help to maintain and improve clinical outcomes.
Emergency conditions are defined as those requiring clinical triage within 60 minutes. Examples include:
Life threatening conditions
- oro-facial swelling that is spreading (with or likely to cause airway or intracranial compromise)
- dental conditions resulting in acute and severe systemic illness
- oro-facial fracture
Emergency dental need
- intra-oral bleeding that the patient cannot control with local measures
- management of avulsed permanent teeth
3.3 Urgent unscheduled care
‘Urgent unscheduled dental care’ refers to conditions that require urgent attention but are not life-threatening. Urgent dental care includes the triage and management of these conditions – both during and outside of normal working hours – and is usually provided within 24 hours or as soon as practicably possible. Examples of urgent conditions include:
- oro-facial swelling or infection that is spreading, recurrent or continuing, with lymphadenopathy (without airway or intracranial compromise)
- severe dental and facial pain (that is, pain that cannot be controlled by the patient following self-help advice including analgesia)
- dentoalveolar injuries, including fractured teeth and severe luxation injuries, that affect oral function or pose a risk to the airway
- avulsed primary teeth
- significant facial trauma requiring urgent referral or review
- intra-oral bleeding that can be controlled with local measures
- severe gingival bleeding requiring urgent treatment, or acute conditions of the gingivae or oral mucosa – including therapy for pericoronitis or for rapidly progressive or necrotising periodontal disease and viral lesions (for example, herpetic) – along with any relevant necessary oral hygiene advice or coaching
Once the patient’s urgent unscheduled care needs have been met, any remaining non-urgent dental presentations should be managed by signposting the patient to ongoing routine care or, where appropriate, transitioning them into personalised care pathways for high needs.
3.4 Non-urgent unscheduled care
This covers patients requiring face-to-face professional care within 7 days and can include the following types of cases:
- mild or moderate pain that responds to pain-relief measures
- minor dental trauma that may require a professional review without clinical intervention (such as concussion injuries involving permanent teeth)
- post extraction bleeding that the patient can control using self-help measures
- loose or displaced crowns, bridges or veneers that are not a risk to the airway
- fractured or ill-fitting dentures (and other appliances) that are affecting oral function or causing oral trauma
- fractured posts
- localised oro-facial swelling that is not spreading, recurrent or continuing (without airway or intracranial compromise or lymphadenopathy)
- fractured, loose or displaced fillings
- treatment of sensitive cementum or dentine
- significantly loose teeth that are not a risk to the airway
- oral soft tissue infections or persistent lesions
The lists above are neither exclusive nor exhaustive. They align with the patient eligibility criteria defined in section 6 of the National service specification for urgent and non-urgent unscheduled dental care.
Within non-urgent unscheduled care (care required between 2-7 days), we can identify 2 key care flows or cohorts:
- reparative and episodic care typically requiring a single, discrete course of treatment involving provisional care
- higher-needs unscheduled care involving generalised, unmanaged progressive disease (predominantly caries and periodontitis) that requires dental care extending beyond the presenting complaint, including behaviour change support, prevention, and initial disease management
Patients accessing unscheduled dental care services who need routine, episodic reparative care will typically receive a single, discrete course of treatment, usually delivered in 1 appointment, where there is no evidence of active disease or clear risk factors. This sort of reparative treatment includes for example, the management of:
- lost fillings
- displaced crowns and bridges
- fractured or broken teeth
- un-restorable teeth requiring extraction
- localised periodontal conditions
Treatment using clinically appropriate restorative materials, exodontia, extirpation or drainage should aim to provide immediate stability while the patient seeks ongoing care. Importantly, preventive advice and guidance should be provided to address risk factors for progressive oral disease where clinically indicated.
3.5 Determining the urgency of treatment
Establishing the nature of unscheduled care required may require assessment of multiple factors identified through triage and clinical assessment (explored further in section 5 and section 6 of this guidance).
These factors may include the extent of pain, swelling, immediate or long-term loss of function, how long the symptoms have lasted and the level of response to appropriate medication.
The patient’s medical history, potential co-morbidities and systemic health risks should be taken into account, and the expressed needs of patients should also be considered (in conjunction with clinical findings) when determining the urgency of unscheduled treatment. This will help decide the most appropriate category of unscheduled care, as described in section 3.1.
Where patients present in unscheduled care appointments with unmanaged progressive disease alongside their acute concerns, these acute concerns are expected to be managed first (without the need for a complete oral health assessment). As explained in section 6, initial progressive disease management should focus on addressing modifiable risk factors that may have contributed to the acute presentation.
Further information on managing patients needing unscheduled NHS intervention after self-funded treatment is available in the Avoidance of doubt: clinical policy for self-funded dental treatment requiring NHS intervention guidance.
4. Access to care
4.1 Access to care
Unscheduled oral and dental care services should be inclusive and accessible to everyone. There should be no physical, language, cultural, social or other barriers to accessing care and not having an NHS number, a GP registration or a current permanent address must not obstruct access. Services should be accessible to and able to meet the unscheduled dental needs of:
- children with dental trauma (following the criteria in section 3)
- people with complex medical needs
- people with physical or sensory disability
- people with safeguarding concerns
- people with specific access problems, such as those who are homeless, housebound, refugees or asylum seekers
Appointments should be of sufficient length to manage individual unscheduled care needs and provide appropriate treatment for the presenting complaint or condition. Within practice settings, treatment length would normally be determined at the clinical triage stage.
Patients should be able to access unscheduled oral and dental care in the most suitable environment, in line with this clinical guidance, and as per paragraphs 7 and 8 of the National service specification for urgent and non-urgent unscheduled dental care.
Patients’ appointments should be provided either through a single point of access, contacting the dental provider directly, or referral into the service. This may include signposting patients into an unscheduled care network. Contact through the single point of access might be through NHS 111 (telephone or online) and/or another single point of access stipulated by the commissioner. Unscheduled care services should have staff with an appropriate mix of skills, training and resources to provide the required care. This should be in line with the unscheduled care timescales outlined in section 3.
5. Clinical triage
5.1 Purpose and process
Clinical triage aims to accurately assess the presenting problem, prioritise patients consistently based on their unscheduled oral and dental care needs, and ensure that appropriate patient pathways are followed based on the presenting clinical needs.
Healthcare professionals triaging patients should be able to identify the nature of the problem and direct patients to the appropriate service within a clinically appropriate timescale. Oral and dental healthcare professionals must ensure teams have the appropriate clinical triage training, experience and skill mix to triage patients effectively. To support members of the team with triage, recognised patient algorithms like Scottish Dental Clinical Effectiveness Programme (SDCEP) should be used. These will help with appropriately managing patients in both unscheduled urgent and non-urgent dental care situations.
The triage process may result in providing remote advice about self-management before a face-to-face assessment. Delivering this advice does not count as an unscheduled dental care appointment, as described in the National service specification for urgent and non-urgent unscheduled dental care. Please see figure 2 in the appendix for a flowchart illustrating this.
Mnemonic aids, such as SOCRATES, can be used by healthcare professionals to support pain assessment during triage:
- Site – where is the pain located?
- Onset – does/did it arise acutely or gradually?
- Character – what is the nature of the pain?
- Radiation – does the pain spread elsewhere?
- Associations – are there any other symptoms related to the pain?
- Time course – how long does the pain last?
- Exacerbating or relieving features – does anything make it better or worse?
- Severity – how bad is the pain (for example, on a scale of 1 to 10, with 10 being the worst)?
Some patients may present with more than 1 symptom. In this case, the main or 1st reported symptom can be used as the starting point of the pain assessment or complaint.
SDCEP’s Management of acute dental problems: guidance for healthcare professionals provides further advice on the management of acute dental problems.
5.2 Pain management
Careful identification of the nature of the problem through triage is crucial to managing the patient and determining how urgently they need care. This includes confirming the source of the patient’s pain and ruling out non-dental sources.
If pain is caused by, or linked to, other factors such as trauma, swelling, signs of systemic involvement, or loss of function, managing these factors may take precedence over pain when they present a greater risk to the patients’ systemic health in the immediate or longer term. The SDCEP Management of acute dental problems guidelines provide decision pathways to help healthcare teams assessing acute dental problems.
For example, the urgency of care for managing deep carious lesions or pulpitic pain (using interventions such as pulp extirpation, pulpectomy, or vital pulpotomy) will depend on the extent and nature of the patient’s pain and how well it can be managed by pain-relief measures. This is outlined in the urgent and non-urgent categories in section 3.
6. Initial ongoing disease management
6.1 Unmanaged progressive disease
This section provides further advice on the management of patients who present with unscheduled oral and dental care needs and also have generalised, unmanaged progressive disease.
Initial disease management aims to improve oral health for patients with unmanaged, progressive dental caries and/or periodontal disease. It helps patients get better control over their condition before more definitive care is provided and helps prevent reattendance at unscheduled care services.
Oral healthcare team members should consider risk factors common to the development and progression of the 2 major non-communicable oral diseases: dental caries and periodontal disease.
To deliver effective initial management, the dental team should:
- advise the patient of:
- the causes of acute current oral and dental conditions
- management processes and pathways, including those for ongoing care needs
- effective self-care and how to prevent further deterioration in oral health through tailored advice on prevention
- the need for ongoing management and monitoring of progressive disease as further banded (separate) courses of treatment
- begin chairside preventative actions such as applying fluoride varnish, ensuring cavities are cleansable and/or using a clinically appropriate restorative material, removing obvious plaque and calculus which could interfere with self-care, and advising on tooth brushing, the use of interdental aids and the mitigation of other risk factors (as described in Delivering better oral health)
- use a suitable behaviour change model, such as the Com-B behaviour change model
Initial management may involve an unscheduled episode or course of treatment that can be delivered in 1, or possibly up to 2 appointments. This may involve addressing the acute presentations during the first visit and raising the patient’s awareness of modifiable risk factors. A subsequent visit would review the resolution of the initial acute complaint and assess how well the patient has applied personalised prevention advice, including addressing the identified risk factors and improving self-care. Reviews of the patient’s response to initial management can take place through face-to-face or remote appointments, in line with NHS England guidance on online consultations.
For the avoidance of doubt, a comprehensive assessment of unmanaged disease, which includes a complete oral health assessment, would not be expected within an unscheduled appointment. Unscheduled care should focus on treating the presenting acute complaint, alongside a brief summary assessment of remaining unmanaged progressive disease. Minimum intervention oral care and British Society of Periodontology principles should be used when addressing dental caries or periodontal disease to promote a movement towards stable oral health.
7. Antimicrobial intervention and stewardship
7.1 Appropriate use and resources
Antimicrobials should be considered as an adjunct to other types of treatment for unscheduled care (for example, pulp extirpation and establishing local drainage of dental infections, where possible). It is not a substitute for appropriate clinical intervention. Before prescribing antimicrobials, dentists should ensure that there has been a thorough face-to-face assessment of the patient.
To reduce the risk of antimicrobial resistance, providers should follow antimicrobial stewardship and prescribing guidance, including helping patients understand when antibiotics are appropriate. Pain relief should be prioritised over antimicrobial medication, where appropriate.
The Faculty of Dental Surgery of the Royal College of Surgeons England, in conjunction with the College of General Dentistry, have published Antimicrobial prescribing in dentistry: good practice guidelines. Further guidance can be found in the UK Health Security Agency’s Dental antimicrobial stewardship toolkit and the Royal College of Surgeons of England’s clinical guidelines.
7.2 Patient assessment
Early recognition and management of oral and dental infections is critical. Patients – particularly children and clinically vulnerable and immunocompromised patients – can become systemically ill within a short period. Untreated local infections may spread, causing significant morbidity and even life-threatening consequences.
An assessment of the patient and subsequent diagnosis should be recorded in the clinical records. It should include, where appropriate:
- a comprehensive medical and dental history in line with the NHS England guidance
- an assessment of the presence of fever (> 38°C), malaise, fatigue or dizziness (note that the antipyretic effect of patients taking analgesics may temporarily lower their temperature)
- measurement of the patient’s pulse and temperature (normal temperature range is 36.2°C to 37°C). A standardised approach and equipment for recording patient temperature and pulse should be used
- definition of the nature, location and extent of the swelling, and any lymphadenopathy
- identification of the cause of the infection
- assessment of presence of sepsis using a decision support tool (for example, the National Institute for Health and Care Excellence (NICE) sepsis risk stratification tools)
After this assessment in primary care, clinical judgement should be used to decide whether treatment can be provided under urgent unscheduled care, or if referral to an emergency care provider such as a hospital specialist is necessary, particularly if you identify:
- signs of septicaemia, such as grossly elevated temperature (above 39.5°C), lethargy, tachycardia, tachypnoea and hypotension
- signs of severe sepsis or septic shock (see the sepsis decision support tool)
- spreading cellulitis
- swellings that may compromise the airway, cause difficulty in swallowing or closure of the eye
- dehydration characterised by lethargy, dizziness and headache
- significant trismus associated with a dental infection
- failure of the resolution of an infection following previous treatment
- a patient who is unable to cooperate with necessary and appropriate care
8. Quality improvement
8.1 Quality improvement of services
Providers of unscheduled care services should be encouraged to continuously improve the quality of care. This should include monitoring of significant events, annual antimicrobial prescribing audits and seeking feedback to support quality improvement.
Resources to support involving people and communities are available on the get involved section of NHS England’s website or by emailing the NHS Public Partnership team: england.peopleandcommunities@nhs.net
Patient-reported outcome and experience measures should be included in the specification.
A suggested patient-reported outcome measure is: ‘Was your dental problem resolved by your visit to the urgent dental care service?’
A suggested patient reported experience measure is: ‘Did you understand what treatment you needed?’
A key feedback tool is the friends and family test (FFT), which is underpinned by the principle that users of NHS services should have the opportunity to provide feedback on their experiences. Primary dental services providers in England must complete and submit the FFT form every month through the NHS Business Services Authority website.
Commissioners should evaluate services as part of the service monitoring and quality improvement process. This is particularly relevant before any re-procurement or extension of a service. Dental public health advice and support should be sought to support these service evaluations.
Appendix diagrams
Figure 1: Management pathways within the unscheduled care system
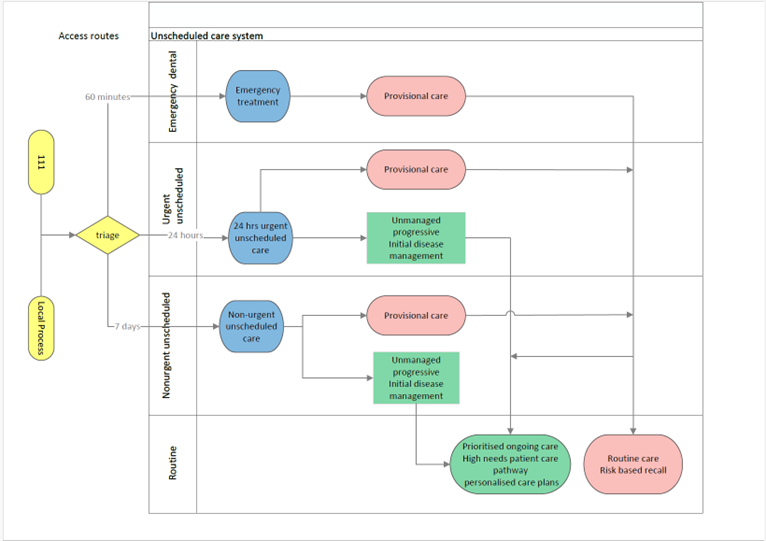
Figure 1: ‘Provisional care’ in this diagram is defined as the treatment of an initial, acute dental presentation using clinically appropriate restorative materials and other clinical interventions. This would be appropriate for patient cohorts requiring reparative and episodic care typically needing a single discrete course of treatment, when there is no evidence of active disease or clear risk factors. The purpose would be to provide immediate stability before a return to routine care.
Figure 2: Unscheduled care flow diagram for general dental practice
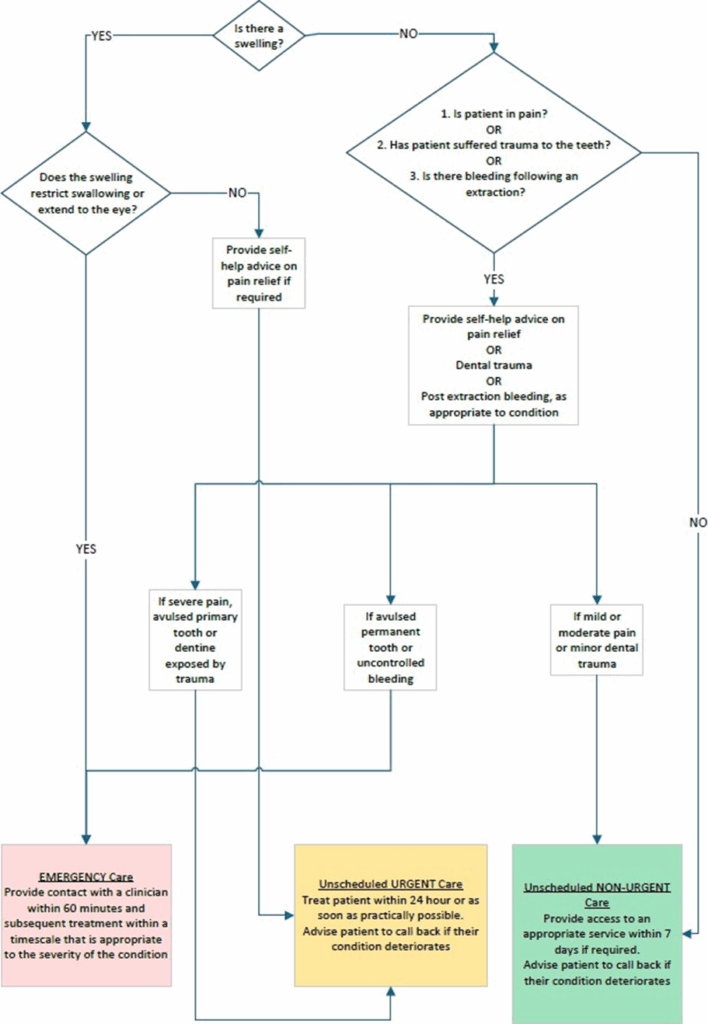
Figure 2: This diagram has been adapted from Prioritising dental emergencies (sdcep.org.uk).
A PDF version of these diagrams is available.
Publication reference: PRN01927_ii

