Classification: Official
Publication approval reference: B2016
Version 2, 10 January 2023
Foreword
The recent COVID-19 pandemic has highlighted the need for preparedness and readiness in healthcare. Specifically, in dentistry, the availability of urgent dental care provision was paramount as routine dental care was suspended on 25th March 2020, to facilitate compliance with national social distancing requirements.
Urgent dental care necessitates the need for simple, rapid access to a dental professional within and outside of normal working hours.
The aim of this clinical standard is to facilitate standardised, equitable patient access to urgent dental care, across England. The care patients receive should be timely, safe and effective while being tailored to meet the needs of the individual. Care decisions should be reached via a process of shared decision making. Care needs will range from remote triage and advice, to delivery of face-to-face care and it is therefore important local systems have the infrastructure, workforce and capability to readily meet these needs. Furthermore, it is important local urgent dental care systems are capable of adapting to changing local and national situations, for example, ensuring a seamless transition and delivery of care through different incident phases (including those related to COVID-19) or more local issues such as major power outages.
This clinical standard is designed to support commissioning teams to work with the dental profession locally to commission urgent dental and out-of-hours care systems. The document sits alongside a series of dental commissioning standards produced to support the transformation of NHS England dental services. Each standard sets out a framework for local work and should be read in conjunction with the Introductory guide for commissioning dental specialties. With the adherence to the standardised framework for place-based commissioning we can ensure that local NHS dental care pathways are developed and commissioned with consistency and excellence, across the whole spectrum of dental service provision.
The pace of transformation will inevitably vary across England with the requirement to conform to national quality standards applicable to all aspects of dental service provision in all regions. Continuing effective local collaboration between commissioners, their local patient populations, the local dental managed clinical networks (MCN), consultants in dental public health and local dental networks (LDN) will assist in achieving the nationally expected standards (note these may change as the role of sustainability and transformation partnerships (STPs) and integrated care systems (ICSs) becomes clear). The focus for commissioners is an assurance for local populations of timely access to high quality, evidence-based urgent dental care; confidence in a service designed at local level to meet local needs aligned with national standards and the NHS Long Term Plan.
1. Introduction
Urgent treatment refers to a course of treatment that consists of one or more of the treatments listed in Schedule 4 of the NHS Charges Regulations (urgent treatment under Band 1 charge):
- examination, assessment and advice
- radiographic examination and radiological report
- dressing of teeth and palliative treatment
- pulpectomy or vital pulpotomy
- re-implantation of a luxated or subluxated permanent tooth following trauma including any necessary endodontic treatment
- repair and refixing of inlays and crowns
- refixing a bridge
- temporary bridges
- extraction of not more than 2 teeth
- provision of post-operative care including treatment of infected sockets
- adjustment and alteration of dentures or orthodontic appliances
- urgent treatment for acute conditions of the gingivae or oral mucosa, including treatment for pericoronitis or for ulcers and herpetic lesions, and any necessary oral hygiene instruction in connection with such treatment
- treatment of sensitive cementum or dentine
- incising an abscess
- other treatment immediately necessary as a result of trauma
- not more than 1 permanent filling in amalgam, composite resin, synthetic resin, glass ionomer, compomers, silicate or silico-phosphate including acid etch retention.
This clinical standard is a revision of the original urgent dental care commissioning standard published in July 2019. The importance of urgent dental care provision during the recent COVID-19 pandemic has led to a review of the previous standard.
This standard supports NHS commissioners in the development of local urgent dental care services appropriate to clinical need. It supports delivery of the commitments on urgent care outlined in the NHS Five Year Forward View and Next Steps in the NHS Long Term Plan.
This standard aims to support the commissioning of urgent dental care, including out-of-hours services, in England, with a focus on ensuring that there is continued access to urgent dental care in the event of local, regional or national incident.
The NHS has a responsibility to ensure people have timely and appropriate access to urgent dental care. Under the NHS primary care dental contracts, general dental service providers are required to provide urgent dental care to patients who are undergoing a course of treatment at the practice within a practice’s normal working hours.
Urgent dental care should be of high quality and integrated with other urgent care services to ensure people with urgent dental needs are seen in the right place and at the right time. Care must be accessible to all patients including children and adults with additional needs and those not currently undergoing treatment in primary dental services. In some cases, urgent care will need to be delivered via a domiciliary route.
When commissioning urgent dental care, commissioners should consider emergency preparedness, resilience and response (EPRR) so that care delivery is maintained in the event of national, regional or local incidents, which may impact access to normal business as usual dental services. The long-term vision is for access to urgent and out of hours dental services to be directed through a national NHS 111 assessing urgent dental care needs through effective triage, underpinned by national and local directory of urgent care services (DoS). This single point of access will standardise access to urgent dental care for patients. Until this national service is available systems will need to ensure that there is an equivalent locally developed pathway in place.
This clinical standard outlines the minimum standards for urgent dental care services and commissioners are expected to implement the standards when procuring urgent dental care. NHS England commissioners are also expected to work with existing service providers and agree a timetable for adoption of these standards.
Purpose of the document
The purpose of the revised standard is to support commissioners to commission high quality urgent dental care services (7 days a week) and where there is a need for emergency dental care (24 hours a day), which are delivered in line with the national transformation plans for urgent care and meet the needs of the patient population including during times of incident.
Objectives:
- define urgent and emergency dental care
- describe standards for the commissioning of urgent dental care
- describe standards for the delivery of appropriate urgent dental care
- support commissioners to commission urgent dental care services which are flexible and can be scaled up or down to cope with planned or unexpected national, regional and local incidents developing contingency plans for each in line with EPRR
- describe possible outcomes for urgent dental care services which can be monitored and evaluated.
1.1 National policy on urgent care
In response to the Urgent and emergency care review and the NHS Five Year Forward View, NHS England developed the Integrated urgent care service specification; a national service specification for the provision of a 24 hours a day, seven days a week integrated urgent care access, clinical advice and treatment service. This service incorporated NHS 111 call-handling and former GP out-of-hours services and has been termed an integrated urgent care clinical assessment service (IUC CAS). Responsibility for its commissioning sits with clinical commissioning groups (CCGs). The specification aimed to revolutionise how urgent care services are provided and accessed to improve experience of, and clinical outcomes from urgent care. A key requirement is that arrangements are made for the management and referral of callers with dental symptoms.
2. Guidance for urgent dental care
2.1 Scope
This clinical standard has been developed to assist commissioners to design and commission urgent dental care services to meet the needs of their population.
Urgent dental care services should be accessible to both the local population and those who are visiting from neighbouring regions or overseas. Services should be accessible to all, including those who find it difficult to access care such as; people with additional needs, children and those not currently undergoing treatment. The services should not be limited by geographic boundaries. Urgent dental care should also be available on a domiciliary basis for those unable to travel to access care.
Primary General Dental Practices should have arrangements in place to deliver urgent care, in working hours, for patients who are undergoing a course of treatment currently, with the practice.
NHS commissioning teams should commission in hours and out-of-hours care for their populations.
2.2 Audience
This document is written for dental commissioning teams.
2.3 Roles and Responsibilities
NHS commissioning teams should assess current service provision against this standard. They will need to work within the newly emerging place-based commissioning structures and local consultants in dental public health. They should work with the public to understand their views, needs and requirements. They should work within emerging integrated care systems engaging with local and regional groups involved in urgent and emergency care, including directory of service leads, clinical commissioning groups and local authority commissioners to engage with place-based commissioning on urgent care to align services.
2.4 Urgent dental care managed clinical network (MCN)
Where there is no urgent dental care MCN, the local dental network must consider establishing one. For more information on how to establish a MCN see the Introductory Guide for commissioning dental specialities.
2.5 Publicising urgent dental care arrangements
NHS commissioners should ensure all stakeholders are aware of urgent dental care services and how to access them. Publicity and communication, particularly with the public, should be updated each time services change so that the information is current. This is especially important as part of incident management.
Information should include the NHS charges that may be payable and information on entitlement to free treatment and how to receive help with health costs; that definitive treatment may not always be appropriate, and that antibiotic stewardship will be in place.
All dental service providers must maintain an up to date entry on the NHS Choices website. Local mechanisms will need to be in place to ensure any updates are also captured in the directory of services (DoS). This is essential, as patients and NHS 111 should be able to rely on the accuracy of the DoS.
3. Commissioning standard development
This standard is a revision of the Urgent dental care commissioning standard published by NHS England in July 2019. As part of the development of the 2019 commissioning standard a rapid review of the literature was undertaken. Patient involvement, along with engagement of key stakeholders, was part of the process.
4. Urgent dental need explained
It is important to differentiate between emergency, urgent and non-urgent dental need as the time in which care should be provided differs between each category.
Urgent is defined as one that requires urgent attention but is not a life-threatening situation. Urgent dental care is the triage and management of these conditions either within or outside of normal working hours. Management of emergency conditions (which are life-threatening) falls out with the scope of this commissioning standard but has been included to recognise its integration within the urgent dental care system. It is also important urgent dental services have the capacity to diagnose, stabilise and refer were appropriate conditions requiring emergency intervention.
The timescales in which each category of need should receive care are outlined below and have been drawn from guidance produced by the Scottish Dental Clinical Effectiveness Programme (SDCEP) on acute dental problems:
- no dental care need – self-care – the patient can manage the problem without the need for face-to-face professional care
- non-urgent dental need – the patient requires a face-to-face professional care within 7 days
- urgent dental need – face-to-face professional care is required within 24 hours
- emergency dental need: face to face dental care required within 60 minutes
- emergency (life threatening) conditions: Life threatening illnesses or accidents which require immediate, intensive care – face to face professional care required within 60 minutes.
The type of conditions within each category are described below:
Emergency (life threatening):
- oro-facial swelling that is spreading (with or likely to have airway compromise)
- dental conditions that have resulted in acute and severe systemic illness
- oro-facial fractures.
Emergency dental need:
- bleeding that the patient cannot control with local measures
- avulsed permanent tooth.
Urgent dental need:
- oro-facial swelling that is spreading, recurrent or continuing (without airway compromise)
- severe dental and facial pain: that is, pain that cannot be controlled by the patient following self-help advice including analgesia
- dentoalveolar injuries, including fractured teeth
- significant facial trauma requiring urgent referral or review
- bleeding which can be controlled with local measures.
Non-urgent dental need:
- mild or moderate pain: that responds to pain-relief measures
- minor dental trauma which does not require professional intervention
- post-extraction bleeding that the patient can control using self-help measures
- loose or displaced crowns, bridges or veneers
- fractured or loose-fitting dentures and other appliances
- fractured posts
- fractured, loose or displaced fillings
- bleeding gums.
5. Assessing local needs and current service provision
Planning oral healthcare services must be underpinned by a needs assessment. In the context of this commissioning standard an oral health needs assessment must be used to determine if current urgent dental care service provision is meeting local oral health needs. This needs assessment must be supported by a consultant in dental public health. Commissioners must assess current urgent dental care (UDC) provision within the UDC system, including care provided by teaching hospitals and other secondary care services.
The need for urgent dental services will vary depending on planned or unexpected national, regional and local incidents, in line with emergency planning and contingency planning. The method utilised for the needs assessment should aim to answer the following:
- What is the health problem?
- What is the size and nature of the problem in the population?
- What service provision currently exists and where is it located?
- What do professionals, patients and the public and other stakeholders need?
- What are the most appropriate interventions?
- What are the resource implications?
Chestnutt et al. (2013) described a process for undertaking an oral health needs assessment and the broad stages which is set out in the overarching commissioning standard with examples of how this can be applied to urgent dental care.
6. Standards of delivery
6.1 Access to urgent dental care
Access to urgent dental care should be simple. Ideally this should be through a national NHS 111 (telephone or online) specific dental triage queue for those not currently undergoing treatment with a dental provider. This triage service should be available 24 hours per day, 7 days per week. Once a dental need has been established, triage should be undertaken by an appropriately trained and experienced dental team member. Patients’ appointments should be booked where possible into the urgent dental care service in line with the timescales outlined in section 4. Where this national system is not available a comparable local service should be commissioned according to IUC standards.
To simplify the referral process between NHS 111 and urgent dental services, a digital method is preferable. This may require the procurement of software and or additional equipment.
In a locally commissioned service if calls are triaged outside of the NHS 111 pathway, the service should be in line with the requirements of the national service specification for NHS 111, with similar patient dispositions. Calls should be redirected from NHS 111 using a simple single layer ‘press 1’ style interactive voice response process, which facilitates computer automated redirection. Any local triage systems should fit with the SDCEP definitions and timescales that are used in this standard. The triage service should be able to:
- receive patient information via NHS 111
- receive patient calls directly from NHS 111
- return calls and carry out a clinical telephone triage
- provide information and advice to callers, including pain management advice and signposting to NHS dental services
- use appropriately trained personnel
- advise on patient charges for urgent dental care and exemptions and advise on what to expect from the urgent dental care service
- undertake direct booking to urgent dental care appointments
- consider remote prescribing (as described in section 6.6).
The directory of services (DoS) is an important element of an accessible urgent dental care pathway. The DoS should be accurate and kept up to date for all urgent care services including out of hours and domiciliary services. Secondary care providers with dental or oral and maxillofacial services should be included in the DoS. This should be integrated with the national NHS 111 system.
To support signposting of any non-urgent cases, commissioners should ensure all dental providers keep their NHS website entry accurate and up to date and that the DoS for these services is accurate and up to date.
Urgent dental care services should be inclusive and accessible to everyone and there should be no physical, language, cultural, social or other barriers to accessing care. Commissioners must adapt and ensure that services are able to meet the urgent dental needs of the following groups:
- children with dental trauma
- people with complex medical needs
- people who require domiciliary care
- people with physical or sensory disability
- people with safeguarding concerns
- people with specific access problems such as homeless people, and refugees or asylum seekers
- people living in remote and rural locations.
Care should be provided from a suitable environment to enable access for people with physical and sensory disabilities, including wheelchair access and the availability of a hoist (where possible). Good public transport arrangements should be available. Appropriate interpreting services should be accessible.
The provision of domiciliary urgent care should be available both during and out with normal working hours. This service should be accessible to those who are unable to attend a face-to-face appointment in clinic. An example of a standard operating procedure for such a service can be found in the appendices.
Providers should be encouraged to use a range of methods to keep failed appointments to a minimum.
Treatment slots should be of sufficient length to manage individual urgent care needs and provide wherever possible definitive treatment. This should be a minimum of 20 minutes.
Oral health advice should be given in line with the evidence-based guidance in Delivering better oral health (Public Health England, 2017).
Information about the care provided, should be communicated to the patients’ usual dentist and to any other relevant professionals involved in the patients’ ongoing care within 48 hours of receipt of urgent dental care, where digital interoperability and patient consent allows. Transfer of patient information must meet the required standards regarding data protection/governance.
If the patient does not have a regular dentist, the urgent dental care service should signpost the patient to an accessible local dental service via the directory of services DoS) or NHS Choices. Frequent users of the service should be supported to seek routine continuing care.
Consideration should be given as to how the service will manage increased demand for example public holiday periods.
There should be feedback mechanisms to enable all providers and patients, involved in the urgent dental care system, to feedback. The feedback should be used to continuously improve the services and system.
6.2 Information technology systems
The urgent and emergency care system and pathway relies on IT systems to transfer people between services. There should be connectivity between NHS 111, any additional triage providers, urgent dental care providers, emergency departments and providers of general dental services. IT systems of urgent dental care providers need to be consistent with the national interoperability programme to avoid confusion and delay in the system.
All urgent care dental providers must have @nhs.net email account, to ensure safe transmission of patient identifiable information.
Urgent dental care systems should have access to the NHS Summary Care Record (SCR) to support patient safety. Urgent dental care providers will use this to check patients’ information and medical histories where necessary.
Data should be collected, stored and handled in accordance with General Data Protection Regulation (GDPR). Patient consent must be obtained.
Commissioners should also consider ensuring that urgent dental care services have:
- access to shared patient healthcare records, where appropriate
- the ability for patients to book appointments online
- the ability to signpost patients to other urgent care providers (both general and dental), for example emergency departments.
6.3 Triage and assessment
The purpose of assessment is to enable the consistent prioritisation of patients to ensure that those whose condition cannot be deferred to the next available in-hour dental service receive care, as appropriate, in the most suitable environment.
For local services commissioners should ensure that any triage and assessment protocols identify people who have an urgent dental need. The triage/assessment outcomes should match the descriptions of urgent dental problems and associated timescales described in section 3.
6.4 Shared decision-making
The care offered in an urgent dental care service should reflect evidence-based treatment. Any NHS treatment decision should be made between the practitioner and patient, following discussion of the options and their respective risks and benefits.
Commissioners should implement policies, procedures and design services to facilitate the shared decision-making process.
6.5 Advice
Advice should be available and be recorded on the patient’s clinical notes as part of their treatment history. This advice should include self-care and incorporate advice on analgesia signposting to other relevant services should also be available.
6.6 Remote Prescribing
In some situations, there may be a requirement for remote prescribing.
Video consultation may support the decision to prescribe where a face-to-face assessment is not possible and should ideally form part of the patient’s clinical records.
Where possible, remote prescribing should form part of urgent dental care provision and contingency planning.
Engagement and collaboration with local pharmacies will be essential when considering how this will be implemented.
To reduce the risk of antimicrobial resistance, providers should follow antimicrobial stewardship and prescribing guidance, including helping patients understand when antibiotics are appropriate.
Further information on remote prescribing can be found on the General Dental Council’s website.
6.7 Workforce
Urgent dental treatment in primary care can be undertaken by dentists who have completed NHS foundation training or equivalence and are on the NHS performer list. Triage can also be completed by dental care professionals (DCPs) following appropriate training and experience. Consider redeployment plans and indemnity arrangements for staff involved both within and out with regional boundaries.
Dentists should be able to demonstrate experience treating people with urgent problems and advising on pain management. This will include skills in the management of dental trauma, pulp treatments and dental extractions. They should also have experience in providing care for people with special care needs, including people with disabilities and dental anxiety. Skills should be maintained by undertaking relevant continuing professional development. This will include training in treatment of urgent conditions and keeping up to date with appropriate prescribing.
7. Emergency Preparedness, Resilience and Response
The standards expected for the provision of urgent dental care, outlined previously in this document, must be maintained during all situations. Commissioning teams must therefore ensure UDC services have the flexibility to adapt to changes in demand. The ability to increase capacity, in response to local, regional and national incidents, is paramount in maintaining a constant provision of urgent dental care.
In the NHS, incidents are assigned to one of the below classifications defined by the EPRR Framework:
- business continuity incident
- critical incident
- major incident.
Each occurrence has the potential to impact upon service delivery and therefore contingency plans to safeguard service continuity must be designed and available. NHS commissioning teams maintain the responsibility for alerting local dental systems of such incidents and its consequence and subsequent management.
Business continuity incident
A business continuity incident is an event or occurrence that disrupts, or might disrupt, an organisation’s normal service delivery, below acceptable predefined levels, where special arrangements are required to be implemented until services can return to an acceptable level (this could be a surge in demand requiring resources to be temporarily re-deployed).
Critical incident
A critical incident is any localised incident where the level of disruption results in the organisation temporarily or permanently losing its ability to deliver critical services, patients may have been harmed or the environment is not safe requiring special measures and support from other agencies, to restore normal operating functions.
Major incident
A major incident is any occurrence that presents serious threat to the health of the community or causes such numbers or types of casualties, as to require special arrangements to be implemented. For the NHS this will include any event defined as an emergency.
An example of how different level of incidents may affect urgent care services is shown in figure 1.
As an event evolves, if deemed a national incident it may be assigned a national incident level. For clarity these formal EPRR incident levels must be used by all organisations across the NHS when referring to incidents. The EPRR incident levels outline the geographical nature of incidents in a local, regional and national sense.
To ensure that commissioners can respond to incidents they must ensure that they receive local, regional and national incident alerts in a timely way and are linked into Local Resilience Forums (LRF). They must be able to communicate the alert status, and the impact this has on the provision of dental care in the area and the subsequent impact on demand for urgent dental care services.
Commissioners of NHS urgent dental care services must ensure that they have contingency plans in place for urgent dental care services which can be implemented if an incident arises.
Support for contingency planning can be found in the NHS England Business continuity management framework.
Contingency plans for urgent dental care services must consider actions which would need to be taken at each level of incident to ensure that access to urgent care is maintained. The level of service available will depend on the incident and the local situation. Commissioners should consider the below key areas:
Contingency Planning
- Plans
Contingency planning should be undertaken by each commissioning team and urgent dental care system. This should outline the policies and procedures to follow if and when an unexpected incident occurs. - Coordinated mechanisms
Contingency plans should be drafted and coordinated with neighbouring systems and regions. This will allow a coordinated response if and when needed.
Capacities
- Risk assessment
Assessment of any potential risk to the service, staff and patient cohort is essential. Requirement and delivery of urgent dental care should be assessed on an individual patient basis. - Information management
Efficient and secure methods of communication and effective transfer of patient records between providers and services will improve patient journey and should be designed and implemented to assist with incident response.
Resource
- Financial resource and contingency funding
Increased demand for urgent dental care during incidents results in increased financial requirement. - Logistics and supplies
Availability of essential supplies, for example, personal protective equipment (PPE) will determine the provision of urgent dental care. Commissioners should consider availability and procurement of supplies. - Workforce
Workforce is essential in delivery of dental services. During a national, regional or local incident, workforce capacity and resilience may be reduced. It is therefore important to plan availability and incorporate contingency. Consider redeployment plans both within and out with regional boundaries.
Although the NHS is not responsible for commissioning private dental services the impact of an incident on these services, and consequently the impact this has on access to dental care, must be considered when contingency planning.
Figure 1. Illustrative example of how incidents may impact delivery of urgent dental care
Incident classification: Business continuity incident
Example of incident(s): PPE shortage or emergency drug shortage
Example of contingency plan requirements:
- regionally procured supplies
- consider sharing agreements with neighbouring regions
- business continuity planning.
Incident classification: Critical incident
Example of incident(s): Power outage or flood
Example of contingency plan requirements:
- increase in demand for urgent dental care sites in unaffected zones (could be a neighbouring region)
- increase flexibility across the urgent dental care system
- effective and timely means to update UDC availability on DoS.
Incident classification: Major incident
Example of incident(s): National COVID-19 lockdown
Example of contingency plan requirements:
- increase in demand of urgent dental care sites with provision of routine/elective care reduced
- increase flexibility across the urgent dental care system to meet increased demand
- re-deployment policy including crown indemnity arrangements for activities outside of usual scope of practice, eg fit testing of respirators.
8. Quality improvement
Providers of urgent dental care service should be encouraged to improve continuously the quality of care delivered to service users. This should include monitoring of significant events, annual antimicrobial audits and seeking feedback to improve the quality of services. Key performance indicators should be included in the specification for the service and these should be patient-focused and include public involvement, clinical and organisational indicators.
Resources for support involving people and communities can be accessed on the Get involved section of NHS England’s website or by emailing the NHS Public Partnership Team: england.engagement@nhs.net.
Patient reported outcome and experience measures should be included in the specification:
- A suggested patient reported outcome measure is ‘was the problem resolved by your visit to the urgent dental care service?’
- A suggested patient reported experience measure is ‘did you understand what treatment you needed?’
As part of the service monitoring and quality improvement process an evaluation of the service should be undertaken by the commissioners. This is particularly relevant
when considering extending the contract for the services or prior to any re-procurement of the service. Dental Public Health advice and support should be sought to support any service evaluation.
Appendix A: Key definitions
Urgent dental care system:
This term describes the network of urgent dental care providers, incorporating those involved providing care within working hours and those providing care out-of-hours. The system also includes urgent dental care provided by emergency services, secondary care services (for example, oral and maxillofacial surgery (OMFS)) and community dental services and triage and call handling services.
Urgent dental care
Urgent dental care is care provided to manage a patient condition/illness that requires urgent attention, but which is not life threatening. This care can be provided both within usual operational hours and outside of normal working hours. Care can range from telephone advice to dental treatment in a surgery.
Out-of-hours care
Out-of-hours care (OOH) is defined as urgent dental care, provided exclusively outside of normal operating/working hours. This time will vary between region and local systems.
Figure 2 illustrates the services which may be part of an urgent dental care system
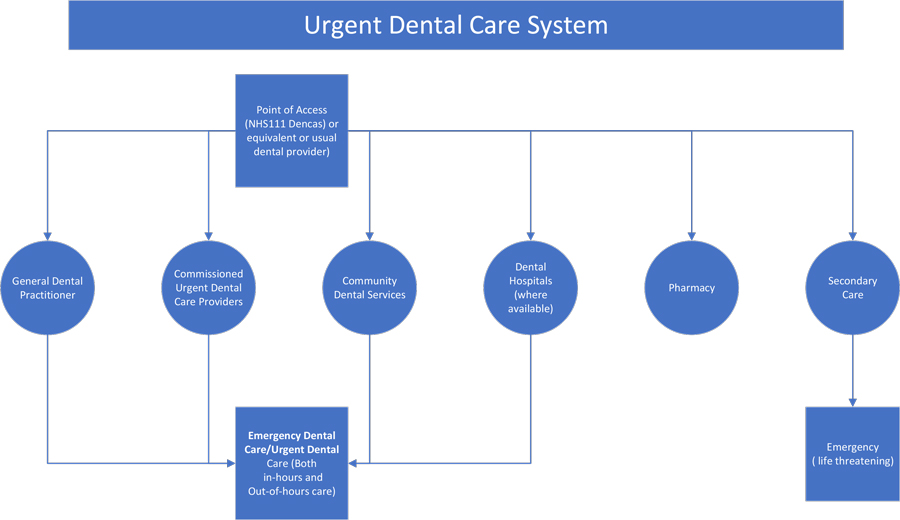 Urgent dental care needs assessed by 111 should be provided by an appropriate dental care settings such as general dental practices, UDC providers, community dental services or dental hospitals (were available). Emergency care should be sought for life threatening condition.
Urgent dental care needs assessed by 111 should be provided by an appropriate dental care settings such as general dental practices, UDC providers, community dental services or dental hospitals (were available). Emergency care should be sought for life threatening condition.
Appendix B: Case studies
Case study 1: London
NHS England London team inherited the legacy of 31 urgent dental care models in April 2013. Inconsistencies existed in provision and not all boroughs had a dental nurse triage service in place.
A pan-London needs assessment was undertaken in 2014/15, modelled on the areas of London that historically had dental nurse triage services. Call volumes were estimated and assumptions made about patient end-points, for example telephone advice given and booked into an urgent dental care treatment slot).
In 2015/16 three new dental nurse triage services (North and South London plus an overnight service) were procured and went live in April 2016. Running in tandem to the dental nurse triage project was another project to ensure that sufficient urgent dental care treatment slots were available.
A competitive procurement exercise took place in 2016/17 to seek dedicated urgent dental care slots in existing general dental practices.
NHS England London team regularly meets with its dental nurse triage provider to ensure that urgent dental care treatment capacity meets demand. The current system has proven to cut dental presentations at London emergency departments. Both commissioning projects have driven a consistent patient offer for Londoners and make full use of the national NHS 111 number for a single point of access.
The dental nurse triage service is commissioned through a standard NHS contract which is demarcated into three areas, north London, south London and an overnight service. The dental nurse triage contract is an amalgamation of a block of 145,000 calls per year and £10.50 per call above this volume. It is very difficult to ascertain how many calls are received per year. The urgent dental care treatment slots are commissioned through a combination of a fixed retainer (145,000 calls), units of dental activity, which is 1.2 for an urgent treatment, and sessional costs. During bank holidays, costs are doubled.
The challenge for the region has been assessment of local needs, which will be reported on imminently, and service evaluation, which will go through the emerging integrated care systems.
Case study 2: Cumbria and North East
NHS England Cumbria and North East teams reviewed unscheduled, urgent and emergency dental care provision following concerns raised by the dental profession, patients, CCGs and NHS 111 that patients were finding it difficult to secure reliable and responsive access to urgent dental care, particularly via NHS 111. The local dental network executive established a review team during 2015/16, jointly led by a local dental network clinical lead and NHS England dental commissioner, to conduct a whole pathway review in accordance with the principles outlined in Securing excellence in commissioning dental services.
The findings from the review highlighted significant gaps in provision and areas of non-compliance when benchmarking the local pathway and services against emerging national urgent care guidance and standards.
This resulted in a need to re-model and re-engineer the whole system locally on a phased basis:
- Phase 1 (2017/18) resulted in the procurement of a small number of dedicated NHS 111 in hours unscheduled care pilots, which have proven successful.
- This led to implementation of Phase 2 (2018/19), which includes the procurement of a Cumbria and North East wide NHS 111 fully integrated dental clinical assessment service that will be compliant with national urgent care standards alongside the introduction of further dedicated NHS 111 in hours unscheduled care services.
- The final phase (2019/20) will result in the re-modelling and re-procurement of out of hours treatment services based upon the learning drawn from Phase 1 and 2 and the impact this has had on patient flows.
The aim is to ensure that in future patients can reliably and responsively access urgent dental care in hours, reducing the demand on out of hours treatment services and providing an improved outcome for all patients presenting with urgent dental needs across Cumbria and the North East.
Case Study 3: North Yorkshire and Humber: COVID-19 UDC response
North Yorkshire and Humber is geographically large with rural areas. In responding to the COVID-19 pandemic, a decision was made to provide urgent dental care using a less centralised and more devolved strategy, reducing distances for patients to travel. A single urgent dental care treatment centre (UDCTC) for suspected or confirmed COVID-19 patients was established centrally with 48 UDCTCs set up to support 36 clusters (groups of local practices), with a number established to provide treatment to callers to NHS 111 and community dental services patients. Additional activity was commissioned to support the urgent dental care provider who supports calls to NHS 111.
This system allowed for groups of practices to manage urgent dental care collaboratively and for all practices to be able to contribute to the service and have experience of working protocols. The system also allowed PPE to be concentrated to active treatment centres where it was most needed.
Dental practices were divided into clusters of 4-12 practices depending on geography and each cluster had an active UDCTC. All the cluster practices delivered remote triage, only referring those patients requiring urgent and essential face-to-face care to the UDCTC.
A local operating model was drafted, which was circulated to providers, alongside the Office of the Chief Dental Officer’s (OCDO) standard operating procedures. This local operating model included a standard referral form to be used for all callers to determine the most appropriate clinical setting for their onward referral, where necessary. Patients seen for face-to-face care in an UDCTC were discharged back to the cluster practices for follow up care requirements, ensuring continuity of support for patients at cluster level and allowing the UDCTCs to focus on urgent care interventions.
Clear protocols were provided in written form and also communicated through weekly webinars. Effective communication channels using email and encrypted messaging services were used to advise and inform. Health Education England (HEE) and Public Health England (PHE) worked in support of the local NHS England commissioning team, with HEE setting up a webpage for local and national documents. Weekly mailouts were sent to all providers keeping them informed and a communication plan established to liaise with external stakeholders.
HEE also worked with UDCTCs to develop localised delivery protocols and systems were set up to audit referrals, capacity, workforce and PPE. The regional dental clinical assessment and booking service provider, which forms part of the NHS 111 pathway across Yorkshire and the Humber, was supported to signpost callers to practices closer to the caller’s home, which with the intention that this would reduce call handling delays, improve triage and offer a more convenient offer of care to the for patient.
Appendix C: Flow-process and monitoring for disruption to business as usual (BAU) activities
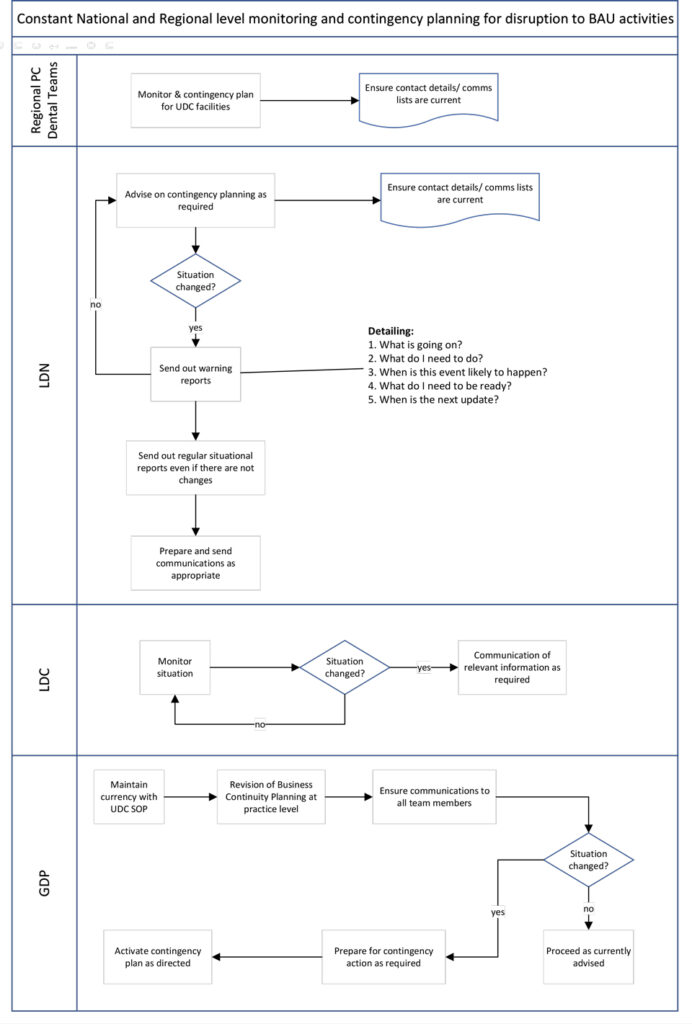
Current contact details and effective communication lines should be established between regional primary care (PC) dental teams, local dental networks (LDNs) and local dental committees (LDCs) to allow a coordinated response if and when needed.
This would ensure UDC services have the flexibility to adapt to local or national incidents and resultant changes in demand. The ability to increase capacity, in response to local, regional and national incidents, is essential in maintaining a constant provision of urgent dental care.
Appendix D: Standard Operating Procedure (SOP) for domiciliary services
Appendix E: Commissioning Cycle
- A local needs assessment has been undertaken to identify levels of need for urgent dental care and identify any gaps and/or inequities in service to inform the level of service commissioned.
- Consideration has been given to establishing an urgent dental care managed clinical networks (MCN) to assist in implementation of these commissioning standards, quality assurance and ongoing monitoring and review of urgent dental care services.
- The local arrangements for urgent dental care have been publicised widely across the local health and social care economy and to patients and the public.
- There is a mechanism in place to ensure the NHS website for dental services is up to date.
- There is a mechanism in place to ensure all directories of services are up to date.
- A personal dental service agreement has been used to contract the service on a sessional basis and ensure service provision in hours where possible.
- Access to the urgent dental care service is via NHS 111 and NHS 111 online.
- Direct booking into the urgent dental care service has been established where possible or, until this is possible, a local mechanism for booking has been developed to ensure service users are required to make one phone call only.
- Urgent dental care services are inclusive and able to meet the urgent dental needs of all people, either directly through an urgent dental care provider or through an alternative pathway that is included in the directory of services (DoS).
- Treatment slots within the urgent dental service are of sufficient length to enable management of individual urgent care needs and provision, wherever possible, of definitive treatment.
- There are mechanisms in place to capture patient reported outcomes and experiences.
- Plans are in place to ensure the service will cope at periods of higher demand, for example public holiday periods.
- All providers of urgent dental care have business continuity plans in place.
- A service review date has been set by the commissioner.

