A national project in England on aligning quality improvement (QI), experience of care and co-production
Classification: Official
Publication reference: PAR1498_iv
Why?
- Quality improvement and improving experience of care are often in separate silos in NHS organisations.
- Few NHS organisations are co‑producing improvement with people with lived experience.
- We wanted to understand how some organisations had gone about making progress in aligning quality improvement, improving experience of care and co‑production, in order to share that learning.
Who?
- NHS England’s Improvement directorate and Experience of Care team.
- Initial Advisory Group – people with lived experience, We Coproduce, NHS provider staff, Health Foundation, The King’s Fund, Coproduction Collective (University College London).
- Deep‑dive team included someone with lived experience, We Coproduce and NHS England Improvement directorate and Experience of Care team members.
What?
- An evidence review.
- Deep-dive site visits to six healthcare organisations, covering acute, community, mental health and primary care services:
- East London Foundation Trust
- Humber Teaching NHS Foundation Trust
- (Belfast) South Eastern Health and Social Care Trust
- South London and Maudsley NHS Trust
- Tower Hamlets Clinical Commissioning Group
- Western Sussex Hospitals Trust
A model for co-production
“Co‑production is a way of working that involves people who use health and care services, carers and communities in equal partnership; and which engages groups of people at the earliest stages of service design, development and evaluation.
“Co‑production acknowledges that people with ‘lived experience’ of a particular condition are often best placed to advise on what support and services will make a positive difference to their lives. Done well, co‑production helps to ground discussions in reality, and to maintain a person‑centred perspective. Co‑production is part of a range of approaches that includes citizen involvement, participation, engagement and consultation.”
Values
For co‑production to become part of the way we work, we will create a culture where the following values and behaviours are the norm:
- Ownership, understanding and support of co-production by all
- A culture of openness and honesty
- A commitment to sharing power and decisions with citizens
- Clear communication in plain English
- A culture in which people are valued and respected
What is meant by the term co-production?
Our shared starting point is that co‑production is fundamentally different from previous forms of engagement or involvement. Including:
- Recognising people as having assets, strengths, resources and networks that reach beyond the labels we use to describe their ‘position’ within a system or hierarchy.
- Building mutual and reciprocal relationships in which all parties are recognised as having expertise.
- A way of ensuring change/improvement/transformation starts from what matters most to people who use services.
- Founded on genuine partnerships from the very first conversation where we establish what question we are exploring together.
- Sharing power and decision‑making with organisations often ‘stepping back’’’ while communities ‘step up’.
These themes are drawn from publications including ‘Implementing Recovery through Organisational Change (ImROC)’, ‘New Economics Foundation/Nesta’, ‘NHS England/Coalition for Personalised Care’, ‘Social Care Institute for Excellence’, ‘Think Local Act Personal’; quotes taken from ‘Co-production – Sharing Our Experiences, Reflecting on Our Learning (ImROC 2017)’.
What we did
At the start of the project we conducted a literature review in order to better understand how quality improvement, experience of care and co‑production could be better aligned. We asked:
- What evidence is there about how co‑production is used to improve the quality of services and people’s experience of care?
- What makes co‑production successful?
- What are the challenges and barriers in using co‑production to improve quality of services and people’s experience of care?
- How does co‑production work in different settings/situations, and for different groups?
There was lots of interest in co-production and related concepts in both peer-reviewed and ‘grey literature’ (information produced outside of normal publishing and distribution channels, such as policy documents, internal documents, etc.)
- 64 papers selected after full text reviewed: 37 in UK, 11 in USA and Canada, three in Australia, and 13 from other countries.
- Type of publication: 10 grey literature, 54 journal articles.
Summary overview: Influencing factors for alignment of QI, experience of care and co-production
We identified themes and key findings, and have co‑produced some practical recommendations based on what we found.
System level
National and organisational drivers have focused on performance and efficiency improvements
- Give attention to improvements in people’s experience and not just focus on clinical outcomes.
Organisational requirements
Strong senior leadership commitment and sponsorship of QI and co-production
- Leaders need to be open to rapidly translating co‑production outputs into strategic decision making.
- Leaders need to provide sufficient dedicated time and resourcing for service redesign.
Identify and build capacity
- Address preconceptions about the capacity and motivation of people with lived experience to contribute to improvement.
- Develop people’s capacity and confidence to engage in co‑production.
- Identify and address resistance to change.
Point of care requirements
Engage the right people at the right time
- Ensure early involvement and genuine partnership to identify and shape the changes.
- Ensure relevant communities have a say in prioritising and shaping
Communicate openly and formalise participants’ roles
- Create a non‑hierarchical structure.
- Clearly define roles and responsibilities.
Make it easy for people to contribute, be valued and have their input respected
- Consider formal facilitation of the co‑production process.
- Pay attention to the group and power dynamics.
Share responsibility for delivery of the changes/outcomes
- Invest in participants – nurture confidence to co‑deliver improvements.
Valuing all
Co-production values different forms of knowledge and evidence
- See qualitative, narrative and storytelling approaches as having equal value to traditional, quantitative evidence. Value all perspectives.
Our key findings from the six site visits
QI and co-production – a continuum
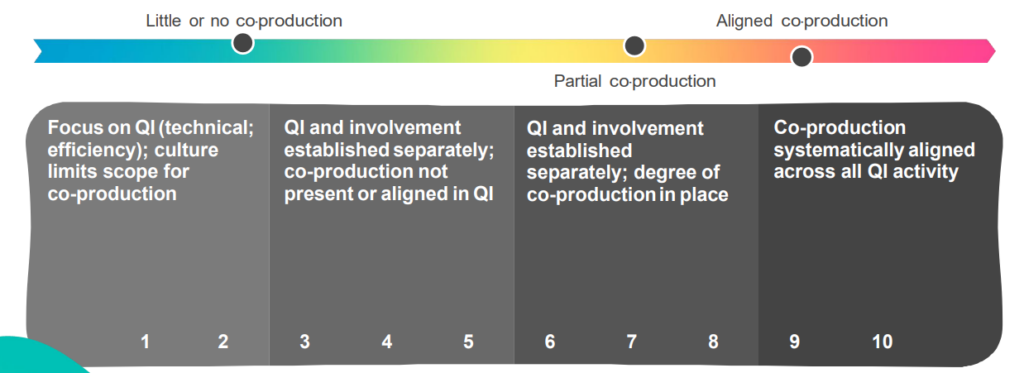
Our key findings
Doing improvement together in a different way involves:
- An intentional shift in culture to systematically align co-production with quality improvement.
- Putting what matters to people at the heart of improvement work.
- Power needs to be shared equally between people with lived and learnt experience.
Deep dive reflections – learning themes from the site visits
This includes a combination of what we observed, our interpretation of what we heard, and the evidence from the literature.
Strong leadership and culture change
- Going beyond one formally responsible director to full board ownership.
- Being comfortable with the uncomfortable.
- Celebrate success.
The successful alignment of co‑production, quality improvement and experience of care requires a cultural change and needs to be driven from the highest level in an organisation or system.
Effective, strong leaders need to explicitly align co‑production and QI priorities together as part of an organisation’s strategy.
All members of the executive team need to own and be committed to the alignment, and successful co‑production and QI work needs to be recognised and celebrated.
Cultural change can be uncomfortable but leaders should model being comfortable with discomfort and recognise it as a natural part of the process.
Starting from what matters to people
- Defining the questions and solutions together.
- Using improvement methodologies and other tools to focus on ‘what matters to people’, for example Always Events®, EBCD, storytelling.
Just as successful alignment of co‑production and QI requires ‘top‑down’ cultural change, change also has to come from the ‘bottom up’, starting from what matters to people.
Far too often QI projects are determined by senior managers and only involve staff when true co‑production requires that the questions and focus for improvements are defined together in partnership.
Methodologies that are built around what matters to people can provide an approach, direction and structure for the process of working together.
Co-production at the heart of QI
- Exploring the opportunities and challenges.
- Improvement focuses on improving experiences of care.
- Rewarding people with proper reimbursement or development opportunities.
Co‑production needs to be at the heart of quality improvement as the default approach with the aim of improving experiences of care.
People with lived experience and staff who are co‑producing quality improvement projects should have the opportunity and space to both learn how to co‑produce as well as develop in their roles.
Proper reimbursement should be provided for people with lived experience who are working with staff in partnership.
Power sharing
- Being curious about resistance and valuing all feedback.
- Reflexivity on the process not just outcomes.
- Being uncomfortable with the uncomfortable and expecting differing outcomes.
- Identify and explore hidden power.
If co‑production and quality improvement are effectively aligned, sharing power will be inherent in how the work is undertaken.
Taking a curious and reflexive approach allows for a non‑defensive exploration of why people may resist sharing power and building new and different types of relationships.
People may feel uncomfortable as individuals with shifts in power but need to accept both discomfort in not knowing the answers and solutions at the start and in accepting differing opinions as a natural part of the process.
Conversations about power can enable people to identify and explore what is hidden or implicit.
Nurturing capability
- Systematic capability building for staff and people with lived experience, including learning together.
- Avoid relying on a small number of key people; build sustainability.
- Network building and knowledge sharing.
- Assets-based approach.
For co‑production and quality improvement to effectively align, people have to learn about how to co‑produce and the tools and techniques of improvement. Capability‑building has to be systematic, equitable and ideally undertaken together.
People’s assets should be recognised and matched to the focus of the work. Far too often, small pockets of excellence exist, relying on a few committed individuals.
There needs to be a focus on wide‑scale capability‑building as well as long‑term sustainability. Building networks between organisations and communities can enhance sustainability along with sharing of knowledge and learning
Community, system and organisational alignment
- Connect with community assets and be responsive to community-initiated ideas.
- Promote and lead capability at system level.
- Improving experience of care and co-production are fully aligned within the organisation.
It is important for the successful alignment of co‑production and quality improvement that work is undertaken at community, system and organisational levels with connections between each.
Organisations and systems need to connect with communities and community assets and be responsive to community‑initiated ideas.
Capability development needs to be led, promoted and delivered at system as well as organisational level.
Working at the community and system level makes it easier to fully align co‑production and QI at the organisational level.
Our initial thoughts and ideas
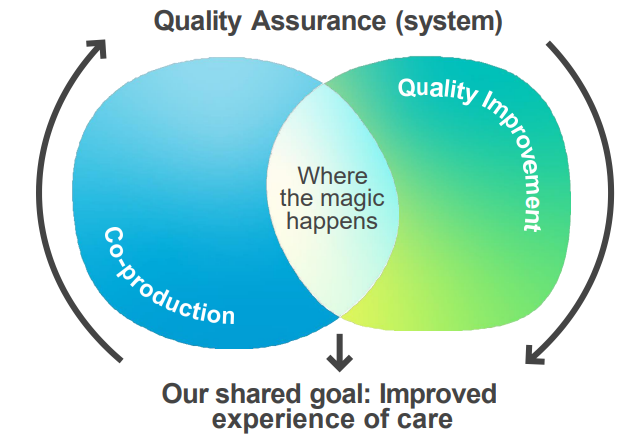
Getting to the third curve
A number of years ago the IHI developed this model to reflect the evolution from an assurance focused healthcare service, to a quality improvement and co‑produced quality improvement focused one.
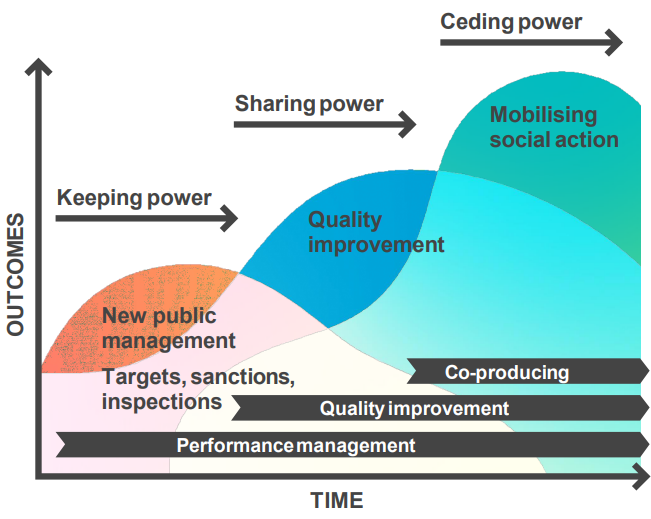
People looking to develop their culture often interpret this in a staged linear way where quality assurance must be addressed before moving on to developing a quality improvement culture, which once established can then evolve into a co‑produced quality improvement culture.
This wasn’t the intent as all three elements are required at the same time all the time. Systems and organisations beginning their journey need to pay attention to all three elements at the same time. We developed the visual on the next page to illustrate this in a different way.
Co-production and beneficial changes: learning from the Covid pandemic
Co-production in our learning from the pandemic response
- Beneficial Changes Network — capturing the innovations made during the pandemic that we don’t want to lose.
- Independently evaluated — ‘Co-production as default’: a critical ingredient for change in implementing COVID-19 related beneficial changes and recovery.
- A paper went to the Quality and Innovation Committee at NHS England (then NHS England and NHS Improvement) in March 2021 and there is now work underway to co‑produce how we bring this recommendation to life and shift the culture to improve the way we co‑produce.
Critical ingredients for change
- Co‑production as default
- Prioritise reducing inequalities
- Leadership for innovation
- Innovation‑friendly environment
What are your next co-produced improvement actions and commitments?
- As an individual?
- As a leader?
- As a system?
For further information and support, contact england.eoccoproduction@nhs.net.

