Foreword
Ambulance services play a vital role in our communities, responding to people’s most urgent needs and at their most vulnerable times. Ambulance staff work with passion and commitment, in some of the most pressured environments and across complex geographies providing compassionate care to patients.
At the same time the National Guardian’s Office report from February 2023 highlighted that there are significant challenges in terms of the culture within ambulance trusts across England.
In my time as Interim CEO at South East Coast Ambulance Service NHS Foundation Trust, I experienced both the vital work undertaken by ambulance services as well as the deep-rooted cultural issues. I had the privilege of spending time on the frontline to truly experience the complexities of the day-to-day pressures, and heard stories from many colleagues about their commitment, passion and pride at working in the ambulance sector. I also heard about how people felt when things didn’t go well, and that sometimes the negative behaviours from colleagues were deeply impactful.
That is why I was pleased to chair and undertake this review, focusing on identifying solutions that will make the biggest difference.
When I started in June 2023 it was very clear to me that engaging a wide range of stakeholders and co-designing ideas for improvement was going to be essential. Ensuring that we heard ideas from staff and leaders within the ambulance service was key, as was hearing from sector experts in academia, membership bodies, regulators and other blue light services. My commitment has always been for us to collectively identify a set of recommendations and actions that over time, we think will positively impact on the culture and lived experience of the people working in ambulance trusts.
My experience has highlighted to me that the ambulance sector is different to other parts of the wider NHS. Therefore, this review was an opportunity to shine a light on that fact and to consider how the local, regional, and national NHS architecture can work differently with ambulance trusts and in a way that is more enabling of cultural improvement. A focus on operational performance often overshadows a focus on people and culture, creating a disconnect between the two, and this is an opportunity for change. That is why the recommendations include actions for us all, and not just for ambulance trusts.
I would like to thank everyone involved in the review. Thank you also to everyone that committed time and many valuable contributions in the meetings, focus groups and interviews.
The establishment of a monthly working group with a broad range of stakeholders became an engine room for testing and evolving the recommendations, and the energy and thought leadership was incredibly powerful. At the last meeting colleagues were very clear in their feedback that the process had been engaging, that cultural change takes time and commitment, and that the outcome of this review should never be a tick box exercise. These three points have stayed with me and can provide excellent guiding principles for how the recommendations are implemented.
Siobhan Melia, Chief Executive, Sussex Community NHS Foundation Trust.
1. Executive summary
The ambulance service, a cornerstone of our healthcare system, is currently facing significant challenges related to workplace culture. The National Guardian’s Office report, ‘Listening to workers: a speak up review of ambulance trusts in England‘, highlighted deeply concerning cultural issues. These included leadership styles that do not adequately support staff to speak up and instances where those who voiced concerns faced intimidation or inaction.
These finding are consistent with the 2022 NHS Staff Survey, which benchmarks performance in the seven People Promise elements. This shows that ambulance sector is below the NHS national average across all elements, although some indicators have seen the biggest improvements on the previous year.
Other blue light services such as the National Fire Service and the Metropolitan Police Service, offer valuable paradigms for the ambulance sector. These services, despite their distinct challenges, have implemented strategies that emphasise collaboration, transparency, and continuous improvement.
This independent review, commissioned by NHS England, considers the prevailing culture within ambulance trusts in England. It considers the core factors impacting cultural norms and offers actionable recommendations for improvement.
Based on insights from key stakeholders, this review has identified 6 key recommendations to improve the culture in ambulance trusts:
- Balance operational performance with people performance at all levels.
- Focus on leadership and management culture and develop the ambulance workforce.
- Improve the operational environment, line management and undergraduate training.
- Translate the NHS equality, diversity, and inclusion improvement plan into a bespoke plan for the sector.
- Target bullying and harassment, including sexual harassment and enable freedom to speak up.
- Prioritise, support and develop human resources and organisational development functions.
Summary of key recommendations and actions
Balance operational performance with people performance at all levels
- NHS England to embed culture improvement alongside operational targets in planning and delivery oversight; and to work with the Association of Ambulance Chief Executives (AACE) to review the role they play in embedding culture improvement in the ambulance sector.
- Integrated care boards (ICBs) to review lead ICB commissioning arrangements.
- Ambulance trusts to routinely review workforce culture alongside operational performance.
Focus on leadership and management culture and develop the ambulance workforce
- NHS England to develop a bespoke leadership and management offer and review existing career frameworks to develop the ambulance workforce.
- ICBs to enable cultural change through facilitating shared learning across ambulance trusts.
- Ambulance trusts to develop clear vision and values, have a registered paramedic on the Board, and provide protected time for individuals to receive leadership and management training and development.
Improve the operational environment, line management and undergraduate training
- NHS England to review health and wellbeing frameworks taking account of operational context.
- ICBs to offer portfolio working opportunities to ensure paramedics are supported to work across organisational boundaries.
- Ambulance trusts to review the paramedic operating environment and management models, and ensure all staff have access to line managers and health and wellbeing schemes.
Translate NHS equality diversity and inclusion (EDI) improvement plan into a bespoke plan for ambulance trusts
- NHS England to collaborate with AACE on a bespoke ambulance sector EDI improvement plan, identifying short, medium and longer-term actions.
- ICBs to monitor the implementation of ambulance trust EDI plans.
- Ambulance trusts to deliver EDI priorities, including tackling barriers to recruitment.
Target bullying and harassment, including sexual harassment and enable freedom to speak up
- NHS England to monitor delivery of the national sexual safety charter, paying particular attention to the ambulance sector.
- ICBs to monitor bullying and harassment including sexual harassment and take action where needed.
- Ambulance trusts to uphold policies and provide training to all staff including managers, an ensure effectiveness of Freedom to Speak Up (FTSU) functions.
Prioritise, support and develop human resources and organisational development functions
- NHS England to partner with trade unions on a collaborative statement to support cultural change and empower human resources and organisational development functions.
- NHS England/ICBs to develop a bespoke human resources and organisational development offer accounting for the cultural and employee relations challenges within ambulance services.
- Ambulance trusts to implement appropriate infrastructure for effective speak up culture, including trained investigators for the most complex cases.
2. Background
2.1 Introduction
The National Guardian’s Office (NGO) report Listening to Workers: A Speak Up Review of Ambulance Trusts in England published in February 2023, called for an independent review of the ambulance sector culture. The report found that the culture in ambulance trusts was having a negative impact on workers’ ability to speak up, impacting worker wellbeing and patient safety. Those who did speak up, often faced intimidation, ostracisation or inaction as a result and the culture of speaking up was not prioritised by leadership. The report summarised its key findings into five themes:
- Culture of ambulance trusts.
- Leadership and management.
- Experience of people who speak up.
- Implementation of the Freedom to Speak Up guardian role.
- Role of system partners and regulators.
The NGO report is consistent with wider findings regarding the ambulance service which includes Care Quality Commission reports, Chief Allied Health Professions (AHP) Officer ‘grey literature’ exploring sexual harassment and misogyny in the ambulance sector (July 2022), recent culture assessments of 3 ambulance trusts undertaken by NHS England teams and the recent NEAS review.
2.2 Scope of the review
The NGO report recommended the cultural review should consider management and leadership behaviours and focus on worker wellbeing, as well as:
- The effectiveness of governance/leadership structures, particularly considering the complex geographical footprint of ambulance trusts.
- Models/expressions of leadership, including ‘command and control’.
- Defensiveness and ‘just’ culture.
- Arrangements for appointments, including fair and open recruitment and values-based recruitment.
- Operational and workforce pressures.
- Bullying and harassment including sexual harassment.
- Discrimination, particularly on the grounds of ethnicity, gender and gender identity, sexual orientation, and disability.
Additionally, the NGO report advised that the review should incorporate insights from other blue-light sector organisations and agree an action plan with specific actions for delivery and organisations assigned to make improvements.
2.3 Methodology
In response to this, NHS England commissioned an independent review, centred around a solutions-based approach.
Underpinned with quantitative findings from the NHS staff survey, this rapid review has mainly centred on the qualitative insights from a range of stakeholders. These were obtained through a set of tailored semi-structured interviews, covering topics across the scope of this review. Key stakeholders were asked to call out challenges as well as potential solutions.
Additionally, background literature has been reviewed including both published and grey literature, with references provided at the end of this document.
A dedicated working group was assembled to develop and review recommendations and actions. The review team has updated both the NHS England Executive and Department of Health and Social Care ministers at set points.
Key stakeholders included:
- ambulance trusts
- human resources directors and organisational development leads from the ambulance trusts
- employee engagement panels with ambulance service staff
- Association of Ambulance Chief Executives
- Care Quality Commission
- NHS Employers
- Chief of Allied Health Professionals at NHS England and wider NHS England senior leads
- Fire and Police services
- Defence Medical Services
- Academics
3. Main findings
The ambulance service profession has developed rapidly in recent years with an increasing scope of practice and increased clinical procedures and protocols. Care Quality Commission (CQC) reports have noted the compassion, dignity and care taken by ambulance staff when treating patients. However, organisational culture has been a consistent area of challenge.
The 2022 NHS Staff Survey benchmarks ambulance performance in the seven People Promise elements, which define what is most important to staff. The ambulance sector is below average in all categories compared to the NHS national average.
2022 NHS staff survey results: overview of national average scores
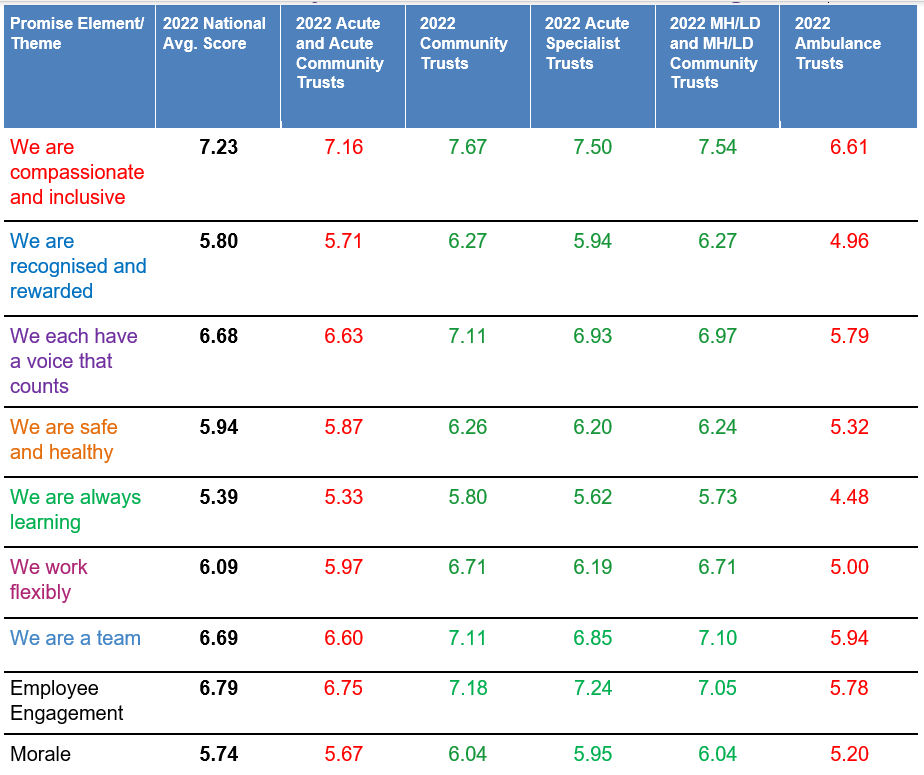
Green numbers show a score higher than the 2022 NHS national average score.
Red numbers show a score lower than the 2022 NHS national average score.
The table above shows how different types of trusts compare against the national average score for results of the 2022 NHS Staff Survey in key areas of the NHS People Promise. Green numbers show a score higher than the 2022 NHS national average score. Red numbers show a score lower than the 2022 NHS national average score.
Each of the seven elements of People Promise is made up of a set of sub-scores. Although most ambulance trusts lag those of the NHS average, there is progress being made. While the compassionate leadership sub-score remains highest in mental health and learning disability and mental health, learning disability and community trusts (7.4) and community trusts (7.4), the biggest improvements this year were seen in ambulance trusts, where the sub-score increased from 6.2 in 2021 to 6.3 in 2022. The inclusion sub score of ‘we are compassionate and inclusive’ also saw ambulance trusts making the biggest improvement – whilst still below average.
3.1 Governance and leadership structures
Ambulance trusts have reported improved relationships with NHS England, noting a shift from top-down messaging to a more collaborative approach that acknowledges operational pressures. However, a focus on operational performance often overshadows a focus on people and culture, creating a disconnect between the two.
Ambulance services also face distinct governance and leadership challenges due to their extensive geographical reach and the need to collaborate with multiple integrated care boards (ICBs).
Key insights from stakeholder interviews include:
- The need to balance the focus on operational performance with people metrics and place patient outcomes on an equal footing to staff experience, recognising the link between good organisational staff culture and patient experience.
- Ambulance service leaders have called for clearer delineation of roles and responsibilities between regions and ICBs, citing challenges in delivering emergency services through a localised model. Ambulance services are instrumental in developing urgent care models that emphasise system-wide collaboration. There is therefore a need to review the commissioning model for ambulance services with ICBs.
- Ambulance services face unique complexities compared to the wider NHS, particularly in their interactions with trade unions, which play a pivotal role in the sector. Effective collaboration is essential for implementing cultural changes, as evidenced by the successful partnership working during industrial action. Opportunities for alignment and policy agreement have been identified through collaboration with the National Ambulance Strategic Partnership Forum (a subgroup of the Human Resources Director Group of Association of Ambulance Chief Executives (AACE)).
3.2 Leadership and management behaviours
Leadership and management is fundamental in shaping organisational culture. The Messenger review recognises the difference that good leadership can make in health and social care and recommends consistency and coordination in the way that leaders and managers are trained, developed, and valued. Concurrently, the Allied health professions strategy for England (2022-2027) highlights the importance of diverse leadership to bolster patient safety, address health disparities and provide equal opportunities for individuals with protected characteristics.
The Paramedic leadership in English ambulance trusts 2023 report specifically focused on strengthening paramedic leadership development and management, promoting values such as equity, diversity, inclusion and belonging, as well as having a registrant paramedic role on the ambulance trust board. Paramedics should also be able to access clinical supervision opportunities as set out in the Clinical Supervision: A Framework for UK Ambulance Services 2021 to encourage aspiring, developing, and established paramedic leaders.
Research by Michael West and colleagues underscores the importance of compassionate leadership in healthcare, advocating that staff must be treated with the same care, respect, and compassion that is expected in patient care. This approach is linked to higher patient satisfaction, lower staff burnout, and increased engagement with organisational change.
CQC reports highlight key areas needing improvement in ambulance services. These often include inconsistent staff appraisals and frequency of supervision by managers, varied approaches to behaviour management, and challenges in effectively managing large staff numbers. The 2022 NHS staff survey further emphasises the need for managers to focus on staff wellbeing, ensure effective communication, and provide clear career progression paths.
Key insights from stakeholder interviews included:
- Support for the promotion and translation of Michael West style of ‘compassionate and inclusive leadership’ into the operational context of the ambulance service.
- The two-way dialogue needed between front line staff and management to provide a greater understanding and promote respect and accountability.
- The need for leadership development training – with core offer nuanced dependent on local context and culture.
- Having a registrant paramedic role on ambulance trust board – in order to provide representative views of the workforce and ensure that cultural issues are given due attention.
- Clarity on career development in the job profiles present in the ambulance service, creating a career framework. The existing AHP Career framework aims to upskill clinical staff and highlights available pathways for staff as well as establishing the different portfolio working opportunities that should exist within the local system. There is also a need to create further opportunities for the unregistered workforce, particularly in control rooms.
- Changing management models. One trust reported moving from one member of staff line managing 40 individuals to 13. This allowed for more one-to-one supervision time with team members.
3.3 Models/expressions of leadership, including ‘command and control’
In the ambulance sector, the prevailing leadership model has traditionally been ‘command and control’, a reflection of how the ambulance service has evolved from its emergency services roots (McCann 2022) [10]. This model, characterised by a strict hierarchy and adherence to established protocols, is symbolised by the rank insignia on uniform epaulettes. However, as the sector changes to encompass patient demand, there’s a growing recognition of the need for a more adaptive management style.
Leaders within the ambulance service during the stakeholder interviews recognised that the command-and-control model only works effectively over a short period of time for a specific purpose but is not sustainable for day-to-day practice. The Paramedic leadership in English ambulance trusts 2023 report acknowledges that organisational leadership should differ to ‘on scene’ command control.
3.4 Operational and workforce pressures
The Pulse survey results, gathered from April to September 2022, have emphasised substantial operational and workforce challenges in the UK’s ambulance sector. A notable 14.7% of respondents reported that excessive workloads adversely affect their emotional well-being and contribute to stress. Many struggle to maintain a work-life balance and call for more managerial support to manage their tasks effectively. Furthermore, 7.0% of participants feel stressed or demotivated, often attributing this to overwhelming workloads. Some perceive the current NHS situation as crisis-like, with little sign of improvement, further fuelling their demotivation.
NHS England’s culture assessment of three ambulance trusts revealed that competing pressures often lead to poor behaviours, with capacity prioritisation overshadowing misconduct management. Staff shortages and limited opportunities for development mean that any work beyond direct clinical care is seen as a luxury or is rushed. Despite this, there is a clear link between positive organisational culture and improved patient outcomes. However, trusts often focus on meeting response time standards for urgent calls, whilst side-lining training, professional development, and research.
The Health Safety Investigation Branch within the NHS patient safety strategy refresh (2023) emphasises the importance of staff safety, including psychological and physical aspects, in supporting patient safety. Factors like staff engagement, fatigue, burnout, and presenteeism are crucial considerations due to their potential impact on both patients and staff.
Key insights from stakeholder interviews include:
- NHS England and the Culture and Leadership Network in Ambulance Services have implemented several initiatives to enhance staff wellbeing and workplace culture. These include a national strategy, a suicide register, a consensus statement for mental health promotion, timely support access, and efforts to create stigma-free organisational cultures prioritising mental health. Although these have made progress, there is still more work to do.
- Ambulance services are using various tools and interventions, including wellbeing guardians, who play a crucial role in promoting health and wellbeing. They meet quarterly under NHS England to share best practices and ensure board-level prioritisation of wellbeing.
- New team working interventions and multidisciplinary collaboration addressing cultural challenges are being explored and have been implemented in certain ambulance trusts. Efforts are also being made to ensure people-centred operational rota processes improve paramedics’ working environment, reduce isolation, and establish portfolio working opportunities.
- Hospital handover delays are negatively impacting staff morale and efficiency, leading to potential burnout and frustration. These systemic issues are also affecting pre-registered paramedic education and training.
- Staff, including students, volunteers, and contractors, are encouraged to act professionally and integrally. The changing nature of the field calls for updated undergraduate curricula to reflect patient demands, potentially including specialised modules like trauma or mental health.
- Finally, staff wellbeing support is essential, with interventions such as the ‘Staying Well Service’ and accessible managerial support.
3.5 Equality, diversity and inclusion, including fair and open recruitment
The Workforce Race Equality Standard (WRES) and Workforce Disability Equality Standard (WDES) have illuminated persistent disparities, particularly concerning ethnicity and disability.
The 2022 WRES report indicates that as a profession, ambulance staff (operational) were least likely to believe that their trust acts fairly with regards to career progression and promotion (53.7%); with especially low levels of belief amongst ethnic minority women (42.9%), ethnic minority men (38.9%), and white men (41.2%) in this profession.
The WDES 2022 data analysis report also shows that the proportion of disabled and non-disabled staff experiencing harassment, bullying or abuse from patients, service users or the public is significantly higher in ambulance trusts.
Ambulance trusts are actively addressing these concerns. Certain trusts have implemented mentorship programs and culture initiatives to support ethnic minority staff, and improved feedback mechanisms are a positive step towards inclusivity. A trust has implemented a ‘Differently Abled Buddy Scheme’ to enhance job retention and foster a positive organisational culture.
These initiatives underscore the urgent need for strategic, policy-driven action to cultivate an inclusive, equitable work environment in the ambulance sector. While the recently published NHS equality, diversity, and inclusion improvement plan is welcome, key feedback from ambulance trusts is that it needs to be translated into a bespoke plan for the sector.
The NHS Long Term Workforce Plan also recognises the need for a significant increase in the paramedic workforce to meet future demands across various care settings. This will need to include tackling barriers to recruitment. Feedback from semi-structured interviews with human resources directors across ambulance trusts highlights several initiatives. These include increasing workforce flexibility, introducing diverse and independent interviewers at recruitment centres to minimise biases, and implementing psychometric testing to assess candidates’ mental resilience. However, inconsistencies in internal secondment policies and advertising methods have been noted.
3.6 Bullying and harassment including sexual harassment
The issue of bullying and harassment, including sexual harassment within ambulance trusts is deeply rooted, and exacerbated by both organisational and psychological barriers. The Association of Ambulance Chief Executives and NHS England have previously published documents including Reducing misogyny and improving sexual safety and NHS England Sexual safety charter based on extensive research and stakeholder input to respond to the widespread issue of sexualised behaviour and underreporting.
Despite efforts in this space, ambulance staff have reported that they continue to face harassment, discrimination, and bullying, often met with scepticism and delayed action. This not only affects current staff but also impacts trainee retention. Trusts often prioritise operational capacity over addressing misconduct, leading to delayed investigations and actions. Human resources and organisational development functions within these trusts often struggle to manage the complexity and quantum of these challenges, indicating a need for significant cultural change.
Interviews revealed that while there are concerns about potentially alienating the sector, there is a consensus that staff safety at work should be prioritised. Clear expectations of behaviour for all staff to act with integrity in order to achieve an inclusive and respectful culture are needed in order to uphold all ambulance trust policies in their treatment of staff, volunteers, students, and contractors.
For the ambulance services to truly embrace a ‘just culture’, it is essential that staff understand the approach taken post-incident. The pressures of the organisation can sometimes amplify a blame culture, where raising concerns might be seen as a sign of weakness or even a threat to one’s job. This can lead to issues such as non-compliance with the statutory duty of candour. When concerns are raised, they must be addressed promptly and effectively, ensuring staff confidence and upholding confidentiality. Integrating a just culture within ambulance services in the UK is not just about addressing errors but fostering an environment where learning and improvement are at the forefront, where colleagues are free to discuss concerns about mental health and wellbeing with each other (Phung V et al, 2022).
Key insights from stakeholder interviews include the need to:
- Ratify the consensus statement of the Reducing misogyny and improving sexual safety workstream and establish a sexual safety charter and embed the principles into practice.
- Ensure the effectiveness of FTSU services and improve anonymous reporting mechanisms, to allow staff to report discrimination and harassment without fear of reprisal.
- Ensure all ambulance staff have sexual safety training and bystander training, building moral self-efficacy and self-regulation within the workforce (Searle R et al, 2017).
- Ensure ambulance staff have access to their managers to provide staff opportunities to resolve issues and equip managers to have ‘difficult conversations’ about behaviour with staff.
3.7 Human resources and organisational development teams
Different methods of conflict resolution are being explored in the sector. One trust has implemented a pre-action review meeting (Pre-ARM) following investigations, chaired by an executive team member, while another uses a resolution hub. The advantages of digitising and streamlining human resources processes were emphasised, along with the necessity for all ambulance services to have trained investigators. This would help manage expectations from the start and clearly communicate the consequences of inappropriate behaviour.
Recognition that effective speak-up cultures lead to a direct impact on human resources development teams, the following suggestions have been made:
- Harmonisation and consistency of human resources policy across all ambulance services.
- Bespoke human resources and organisational development package of support to reflect the large employee relation cases and complexity of the ambulance service.
- Suitable infrastructure for an effective speak up culture – trained investigators and consistent practice with regards to misconduct within an ambulance service.
- Implementing resolution hubs and digitising of processes to streamline and save time and to be able to replicate processes at a national level.
- Guidance on the ‘right’ ratio of human res HR Business Partners, in terms or caseload and/or workforce headcount (to assist with building internal cases for investment.
- Clear reporting and escalation pathways offered to students.
4. Findings from other sectors
4.1 Learning from the Fire Sector
The National Fire Chiefs Council (NFCC) Culture Action Plan has key elements that can be extrapolated and applied to the ambulance sector, particularly in the context of fostering a positive organisational culture. The NFCC’s strategic focus on cultivating an environment that is both inclusive and supportive offers a blueprint that can be tailored to the unique challenges faced by ambulance services.
Central to the NFCC’s strategy is the vision of a workplace where every individual feels valued, protected from discrimination, bullying, and harassment, and is empowered to excel. This vision, while crafted for fire and rescue services, is universally applicable and particularly resonant for the ambulance sector. Given the high-pressure nature of emergency medical services, the emphasis on staff well-being and mental health becomes even more paramount.
The collaborative ethos championed by the NFCC, which involves extensive stakeholder engagement, offers a model for the ambulance sector. By fostering partnerships with staff bodies, governmental agencies, and other relevant entities, a more holistic and encompassing approach to cultural improvement can be achieved. Such collaborations can ensure that initiatives are both comprehensive and tailored to the specific needs of ambulance professionals.
Moreover, the governance structure proposed by the NFCC, which includes both internal committees and an independent external panel, provides a balanced mechanism for oversight. Adopting a similar structure in the ambulance sector can ensure that initiatives are transparent, accountable, and subject to rigorous scrutiny. Regular progress reports, as practiced by the NFCC, can further enhance this transparency, offering stakeholders a clear view of ongoing improvements. The NFCC culture action plan, while designed for a different sector, offers valuable paradigms that can be adapted for the ambulance sector. By embracing a similar strategic approach, emphasising collaboration, transparency, and continuous improvement, the ambulance sector stands to make significant strides in fostering a positive, inclusive, and supportive work environment for all its professionals.
4.2 Learning from the Police Service
The Casey review into the Metropolitan Police Service (Met) offers a comprehensive examination of the challenges and issues the police force faces. Parallels can be drawn with the National Guardian’s Office report into ambulance services and similar learning can be applied. The report explains that the Met is seen as insular, defensive, and resistant to culture change; with entrenched issues such as racism, bullying, misogyny and homophobia.
Recommendations include embedding ethical values from recruitment all the way through careers and holding staff to account for misconduct to signal commitment to integrity. Acknowledging that the misconduct system is inconsistent and fails to tackle repeat offenders; a recommendation included streamlining the misconduct system with clear standards, timeframes and sanctions. Focusing on discrimination, sexual misconduct and abuse of powers. Themes around leadership are also prevalent; requiring regular frontline immersions for all senior staff, empowering middle managers to drive culture change initiatives, introducing surveys, focus groups, and exit interviews to understand frontline experiences and equipping supervisors to have difficult conversations about behaviour. Another key recommendation is to bring in external expertise to drive cultural change and establish a policing Bboard for governance and democratic accountability.
The Met’s leadership appears fragmented, with a discernible disconnect between senior leadership and frontline officers. This emphasises the need for robust leadership in the ambulance sector, fostering open communication and ensuring strategies resonate with on-the-ground realities. Persistent issues of discrimination and bias within the Met, coupled with an inconsistent misconduct system, highlight the importance of accountability mechanisms in public services. The ambulance sector must establish clear standards and procedures to address misconduct.
In summary, the insights from the Casey review hold significant relevance for the ambulance sector, emphasising the importance of culture, diversity, trust, training, and accountability in bolstering its efficacy and public perception.
5. Recommendations
Six recommendations have been identified through this review with actions for NHS England, integrated care boards and ambulance trusts. NHS England is invited to respond to this review and co-develop an action plan with relevant timelines.
Balance operational performance with people performance at all levels
NHS England
- Embed expectations of cultural improvement in the ambulance sector alongside operational delivery using policy levers, such as the urgent and emergency care recovery plan, and maintain grip on cultural progress through an effective oversight process in line with the corporate position set out in the NHS oversight framework.
- Work with the Association of Ambulance Chief Executives to review the role they play in embedding culture improvement in the ambulance sector.
- Ensure people and operational performance is reviewed in the round via national and regional quality and performance committees. Oversight should consider key metrics and qualitative insights (eg peer-reviews), across the main themes for improvement.
Integrated care boards
- Review effectiveness of lead integrated care board commissioning arrangements.
Ambulance trusts
- Ensure Boards routinely review workforce culture alongside operational performance, taking account of the main themes for improvement.
Improve leadership and management culture and develop the ambulance workforce
NHS England
- Collaborate with ambulance trusts to develop and deliver a bespoke ambulance leadership, management and cultural offer, to include Michael West style of ‘compassionate and inclusive leadership’.
- Review existing career development frameworks for the ambulance workforce and develop pathways for ambulance staff to improve retention.
Integrated care boards
- Prioritise and enable cultural change through greater collaboration and shared learning between ambulance and integrated care board teams.
Ambulance trusts
- Develop clear vision and values and role model these from board to floor.
- Have a registrant paramedic on every ambulance trust Board to represent the paramedic voice.
- Provide protected time for individuals to receive appropriate leadership and management training and invest in specialist management skills and training programmes.
Improve operational environment, line management and undergraduate training
NHS England
- Review national health and wellbeing frameworks to ensure they take account of the operational context of ambulance trusts and impact on patient safety.
- Continue to collaborate with partners/college of paramedics to ensure undergraduate training fully represents the patient case mix.
Integrated care boards
- Provide opportunities for portfolio working to ensure paramedics are supported to work across organisational boundaries.
Ambulance trusts
- Review the operating environment of paramedics, ensuring the operational rota is people-centred and collaborative.
- Review management models and bring teams together in more collaborative way, eg team-based working.
- All staff to have clear and direct access to a line manager.
- Continue to develop and deliver health and wellbeing schemes for all staff.
Translate the NHS equality, diversity, and inclusion (EDI) improvement plan into a bespoke plan for ambulance trusts
NHS England
- Collaborate with the Association of Ambulance Chief Executives to translate the NHS equality, diversity, and inclusion (EDI) improvement plan into a bespoke ambulance sector EDI improvement plan and include short, medium, and long-term actions.
Integrated care boards
- Monitor and oversee the implementation of ambulance trust EDI improvement plans.
Ambulance trusts
- Deliver EDI priorities. To include tackling barriers to recruitment, working on adverts and job profiles to improve diversity.
Target bullying and harassment, including sexual harassment and enable freedom to speak up
NHS England
- Monitor delivery of the national sexual safety charter and consensus statement for reducing misogyny and improving sexual safety, paying particular attention to the ambulance sector
Integrated care boards
- Prioritise tackling bullying and harassment including sexual harassment and continue to take action where needed.
Ambulance trusts
- Uphold all ambulance policies and take appropriate action and ensure all ambulance staff act with integrity to their colleagues, students, volunteers, and contractors.
- Ensure all staff receive sexual safety and bystander training, and equip managers to have difficult conversations, building moral self-efficacy and self-regulation within the workforce.
- Boards to ensure the effectiveness of Freedom To Speak Up (FTSU) functions to allow staff to report discrimination and harassment without fear of reprisal.
Prioritise, support and develop human resources and organisational development functions
NHS England
- Partner with national trade union leaders on a collaborative statement to support cultural change and empower human resources and organisational development functions.
- Work collaboratively with integrated care boards to develop and deliver a bespoke human resources and organisational development offer accounting for the cultural and employee relations challenges within ambulance services. To include guidance on the right ratio of human resources business partners.
Integrated care boards
- Work collaboratively to develop and deliver bespoke human resources and organisational development package of support accounting for the complexity of the ambulance service and large employee relation cases.
Ambulance trusts
- Implement appropriate infrastructure for an effective speak up culture which includes trained investigators for the most complex of cases.
6. Next steps and measuring success
Changing the culture of ambulance trusts will take time, commitment, energy and action from all parts of the system. Success can be measured through the lived experience of people who work in ambulance trusts, both quantitively via the staff survey and aligned People Promise themes and metrics referenced earlier in this review, and through more qualitative approaches. Specific areas of focus should be the reduction of the number of formal employee relations cases in ambulance trusts, retention rates, the improvement in staff survey staff engagement scores, an increase in the number of staff who state that their organisation has taken positive action to improve wellbeing in the survey, and an improvement in recommend as a place to work survey scores.
NHS England is invited to respond to this review and to work with integrated care boards and ambulance trusts to implement the recommendations and actions.
7. References
1. Speak Up Review of Ambulance Trusts – National Guardian’s Office
3. Health and social care review: leadership for a collaborative and inclusive future – GOV.UK
4. The Allied Health Professions (AHPs) strategy for England – AHPs Deliver
7. What Is Compassionate Leadership? – The King’s Fund
8. Developing the role of AHP Support Workers – Health Education England
9. Paramedics workforce – Health Education England
10. McCann, 2022, The Paramedic at Work: A Sociology of a New Profession – Oxford Academic
11. NHS England » The National Quarterly Pulse Survey
12. NHS England » The NHS Patient Safety Strategy
13. NHS England » NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts
15. NHS England » NHS equality, diversity, and inclusion improvement plan
16. NHS England » NHS Long Term Workforce Plan
17. Reducing Misogyny and Improving Sexual Safety in the Ambulance Service
18. NHS England » Sexual safety in healthcare – organisational charter
19. Phung, VH., Sanderson, K., Pritchard, G. et al. The experiences and perceptions of wellbeing provision among English ambulance services staff: a multi-method qualitative study. BMC Health Serv Res 22, 1352 (2022).
20. Searle R, Rice C, McConnell AA, Dawson J. Bad apples? Bad barrels? Or bad cellars? Antecedents and processes of professional misconduct in UK Health and Social Care: insights into sexual misconduct and dishonesty. Professional Standards Authorisation. 2017.
21. NFCC publishes the Culture Action Plan – NFCC
22. The Baroness Casey Review – Metropolitan Police
Publication reference: PRN01042

