Our commitment to the public in publishing this plan is to improve waiting times and patient experience. We will:
A. Increase capacity, to help deal with increasing pressures on hospitals which see 19 in 20 beds currently occupied.
1. Dedicated funding of £1 billion will pay for additional capacity, including 5,000 new beds as part of the permanent bed base for next winter.
2. Over 800 new ambulances, including 100 specialist mental health ambulances, the majority of which will be on the road by next winter.
3. ‘Same day’ emergency care services will be in place across every hospital with a major emergency department, so patients avoid unnecessary overnight stays.
B. Grow the workforce, as increasing capacity requires more staff who feel supported.
4. More clinicians will be available for 111 online and urgent call services to offer support, advice, diagnosis and, if necessary, referral. From this April we will launch a new targeted campaign to encourage retired clinicians, and those nearing retirement, to work in 111 rather than leaving the NHS altogether.
5. We will grow the workforce with more flexible ways of working and increase the number of Emergency Medical Technicians next year to respond to incidents and support paramedics.
C. Speed up discharge from hospitals, to help reduce the numbers of beds occupied by patients ready to be discharged.
6. Over the next two years, and as part of the up to £14.1 billion extra for health and social care, £1.6 billion will be focused squarely on discharge.
7. ‘Care transfer hubs’ in every hospital ahead of next winter will mean faster discharge to the right setting, so that people do not stay in hospital longer than necessary.
8. This year, new approaches to step-down care will start to be implemented so, for example, people who need physiotherapy can access care as they are being discharged from hospital before they need to be assessed by their local authority for long-term care needs.
9. New discharge information will be published, with new data collected from this April.
D. Expand new services in the community, as up to 20% of emergency admissions can be avoided with the right care in place.
10. Ahead of next winter we will offer more joined-up care for older people living with frailty, including scaling urgent community response, frailty and falls services across the whole country – meaning the right people help you get the care you need, without needing an admission to hospital if it’s not necessary.
11. Greater use of ‘virtual wards’, which allow people to be safely monitored from the comfort of their own home, will be achieved by an extra 3,000 beds to provide over 10,000 in total by this autumn, allowing staff to care for up to 50,000 patients a month this way over the longer term.
E. Help people access the right care first time, as 111 should be the first port of call and reduce the need for people to go to A&E.
12. By April 2024, urgent mental health support through NHS 111 will be universally available.
13. From this April, new data will allow the public to easily see and compare the performance of their local services.
We will also tackle unwarranted variation in performance in the most challenged local systems.
14. This April, a new clinically-led programme to reduce unwarranted variation will launch, alongside intensive support for those areas struggling the most.
Executive summary
Urgent and emergency services have been through the most testing time in NHS history with a perfect storm of pressures impacting the whole health and care system but causing the most visible problems at the front door.
Staff prepared extensively for winter, putting in place thousands more beds, more call handlers, 24/7 care control rooms and respiratory hubs, and often working at the limits of their endurance.
Despite their best efforts, problems discharging patients to the most appropriate care settings, alongside the demands of flu and COVID peaking together, has seen hospital occupancy reach record levels. This means patient ‘flow’ through hospitals has been slower.
As a result, patients are having to spend longer in A&E and waiting longer for ambulances. Hospitals are fuller than pre-pandemic, with 19 out of 20 beds occupied; up to 14,000 beds are occupied by someone who is clinically ready to leave; and the number of the most serious ambulance call-outs has been at times up by one third on pre-pandemic levels.
These pressures have also taken their toll on staff, who have had to work in an increasingly tough environment.
The challenge is not just in ambulances or emergency departments, and so neither are the solutions. Recovery will require different types of providers working together and joining up care better for patients, led by local systems and backed by additional investment.
We also know this is not unique to England, with many similar challenges faced by nations across the UK and across the world.
To support recovery, this plan sets out a number of ambitions, including:
- Patients being seen more quickly in emergency departments: with the ambition to improve to 76% of patients being admitted, transferred or discharged within four hours by March 2024, with further improvement in 2024/25.
- Ambulances getting to patients quicker: with improved ambulance response times for Category 2 incidents to 30 minutes on average over 2023/24, with further improvement in 2024/25 towards pre-pandemic levels.
These ambitions would represent one of the fastest and longest sustained improvements in emergency waiting times in the NHS’s history.
Meeting these ambitions provides a focus for recovery, but they will not be enough on their own. Successive analysis has demonstrated the importance of looking at multiple metrics to support better outcomes for patients.
We will therefore begin to publish more data on time spent in A&E, including 12 hour waits from time of arrival, and we are working with social care partners on a better measure of discharge to ensure we are measuring the whole patient journey in hospital.
Performance against these metrics will fluctuate in response to COVID and other viral illness, as well as the usual seasonal pressures.
But even before the pandemic, pressure on urgent and emergency care had been growing, with changes in demographics and new types of care available, meaning the need for services has been growing every year. And looking forward, our growing and ageing population will see this continue.
We also need to reform and provide a genuinely better experience for patients. This plan builds on the investment and actions taken this winter to increase capacity and resilience, by taking steps to embed what works for patients while also creating space for people to innovate.
It also builds on the experience during COVID, which brought out the best in the NHS – with new services scaled quickly, genuine innovation focused on improving patient care, and better working across different types of care provider centred on the needs of patients.
Through partnerships between acute, community and mental health providers, primary care, social care and the voluntary sector,¹ our ambition is a system that provides more, and better, care in people’s homes, gets ambulances to people more quickly when they need them, sees people faster when they go to hospital and helps people safely leave hospital having received the care they need.
This plan sets out how the NHS and partners will make this a reality and begin to transform patient care. It also sets out the actions being taken in social care to support improved discharge, led by the Department of Health and Social Care (DHSC).
Meeting this challenge will require sustained focus on five areas:
- Increasing capacity
- investing in more hospital beds and ambulances, but also making better use of existing capacity by improving flow.
- Growing the workforce
- increasing the size of the workforce, and supporting staff to work flexibly for patients.
- Improving discharge
- working jointly with all system partners to strengthen discharge processes, backed up by more investment in step-up, step-down and social care, and with a new metric based on when patients are ready for discharge, with the data published ahead of winter.
- Expanding and better joining up health and care outside hospital
- stepping up capacity in out-of-hospital care, including virtual wards, so that people can be better supported at home for their physical and mental health needs, including to avoid unnecessary admissions to hospital.
- Making it easier to access the right care
- ensuring healthcare works more effectively for the public, so people can more easily access the care they need, when they need it.
To support the recovery of urgent and emergency care services, the government has committed to targeted funding in both acute services and the wider system. This includes:
- £1 billion of dedicated funding to support capacity in urgent and emergency services, building on the £500 million used over this winter to support local areas to increase their overall capacity and support their staff
- £150 million to build 150 new facilities to support mental health urgent and emergency care services
- £1.6 billion of additional social care discharge funding over 2023/24 and 2024/25, building on the £500 million Adult Social Care Discharge Fund and £200 million funding for step-down care this winter, to be pooled into the Better Care Fund and used flexibly on the interventions that best help discharge patients to the most appropriate location for them – part of social care investment of up to £7.5 billion over the next two years.
Delivery will require prioritisation at a national level, but also local flexibility – there will not be a one size fits all solution, and local systems, working with social care and others, are currently developing local plans reflecting local needs.
We will ensure delivery focus over the next two years and beyond, with funding allocated as quickly as possible to give local areas the best chance to succeed.
Why we need a UEC Recovery Plan
A. Why are we seeing pressures on urgent and emergency care (UEC)?
Current pressures
COVID is having a lasting impact on NHS services. Throughout 2022 there were never less than 3,800 people in England in hospital with COVID on any given day, with more than 9,000 on average across the year.
This means not just more patients, but also knock-on impacts on the length of time patients are in hospital and more beds closed for infection control.
Occupancy levels for general and acute hospital beds have risen in recent years and have been persistently high over 2022, with around 95% of beds filled on average.
High bed occupancy is a key driver of worsening A&E performance, which in turn has a direct impact on ambulance ‘handover’ and response times.
This is because when hospitals are fuller it is harder to find free beds for patients that need to be admitted from the emergency department, which means it is harder to bring new patients into the emergency department.
The figure below provides a simplified picture of A&E patient flow, highlighting the current constraints in hospital.
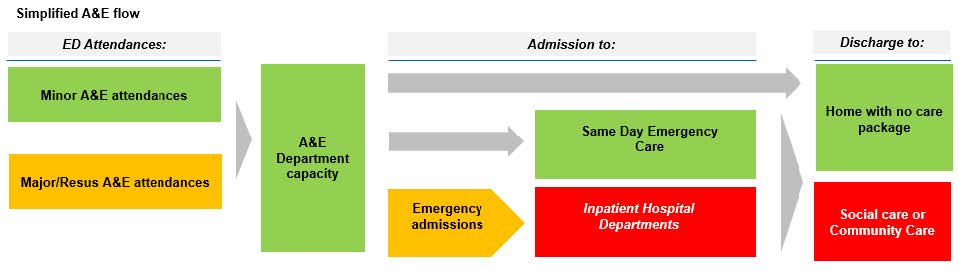
As set out in the diagram, the key driver for performance is high occupancy, with difficulty discharging patients (in particular to social or community settings) resulting in increased length of stay and knock-on difficulties admitting people as inpatients to hospital departments.
From April 2021 to October 2022, average length of stay in general acute hospitals increased by 18%. There are more than 6,000 more patients spending longer than a week in hospital compared to pre-pandemic levels.
Long length of stay has also significantly increased in mental health inpatient care, reflecting increased acuity and challenges around discharge, with 20% of all people staying for more than 60 days. Increasing length of stay is driven by several factors including:
- Increasing complexity of care with patients having more comorbidities, in part linked to COVID.
- Delayed discharge
- While the majority of people are treated and discharged within 48 hours of an emergency admission, for some discharge is more challenging.
- There have been up to 14,000 inpatients who do not clinically need to be in hospital, increasing by more than 10% over the last year – accounting for around 13% of occupied beds.
- This challenge exists across all settings, including mental health.
As set out in the diagram, the number of attendances is not the thing primarily driving performance, but they do create additional pressure. Following a reduction in activity at the start of the pandemic as fewer people came forward for care, demand has been consistently rising.
Attendances have recently been above pre-pandemic levels: December was the busiest month on record for emergency departments in England with nearly 2.3 million attendances, 18,000 higher than the previous high.
The ambulance service also responded to 18% more category 1 calls in December compared to the previous high. We have continued to see admissions from COVID as well as other respiratory illnesses, with more than 350,000 COVID admissions since this time last year.
Taken together, even though there are more beds open now than immediately before the pandemic, occupancy remains very high, reducing patient ‘flow’ through hospitals and creating longer delays for patients at the front door and in the community.
Worsening levels of UEC performance have had a disproportionate impact on those who experience health inequalities.
In 2021/22 NHS Digital reported that patients who live in the 10% most deprived areas (3.0 million people) were twice as likely to attend A&E departments in England when compared to people living in the 10% least deprived areas (1.5 million people).
Longer term trends
The immediate challenges for UEC services come on top of longer-term trends. The need for health and care is continuing to increase as a consequence of population growth, ageing in the population and greater numbers of people living with long-term conditions.
The number of people aged over 85 could increase by 55% over the next 15 years. More than 25% of the adult population in England now lives with two or more long-term conditions, increasing the likelihood of admission to hospital.
In 2019, 33% of people over 18 were estimated to be living with complex multimorbidity, having doubled from 15% in 2004.
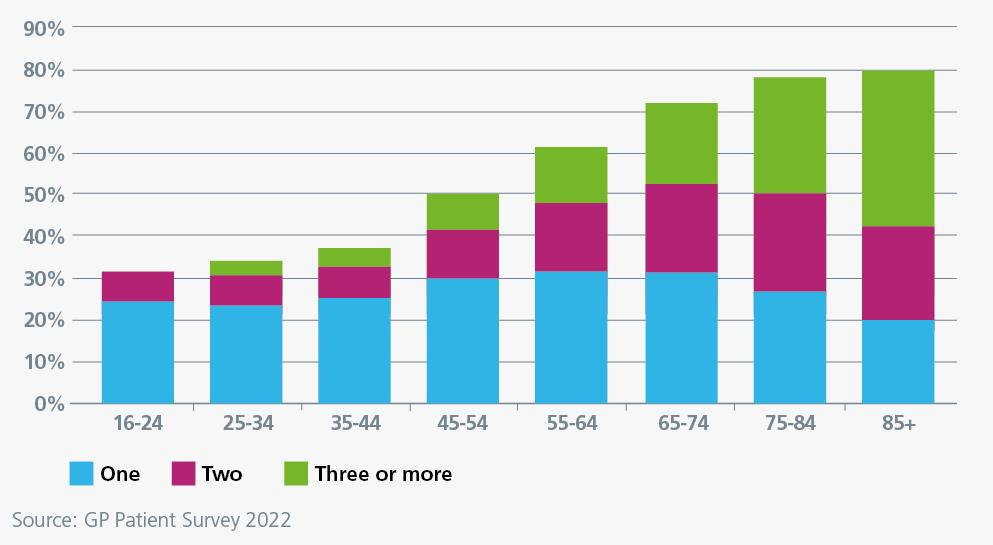
Around 8% of people aged 50 or over are estimated to be frail, as high as 16% in parts of England. England is not the only country facing these challenges, countries across Europe are seeing rising levels of multimorbidity.
A growing and ageing population, with rising morbidity means that the need for UEC services rises every year:
- Demand for NHS 111 has continually increased, with annual growth of 6% a year in 111 calls received in the five years before the pandemic.
- Pre-pandemic ambulance services have faced the challenge of 4% increase in demand year on year.
- A&E including emergency departments and urgent treatment centres have seen rising demand, with faster growth rates for older age people. Demand for major emergency departments has risen gradually but consistently since 2003.
- In 2019 there were 25.6 million A&E attendances (2.1 million a month), 20% more than in 2011. Emergency admissions grew by 28% over the same period to 6.5 million.
The need for UEC mental health services is also growing. Community-based crisis services have seen a 30% increase in referrals since before the pandemic. Long waits for people with mental health needs in A&E are increasing, and people with mental health needs often report poor experiences relating to long waits.
B. What we will deliver for patients and the public
Our vision for UEC is for patients to have access to the right care, in the right place, in a timely way. Hospitals will be appropriate for some seriously ill patients but are often not the best place for many people whose needs are better met in a different way.
Delivering this ambition will mean supporting more patient-centred, personalised care, accessed closer to, or at, home – but also more integrated services.
We will take the opportunity of new and existing technologies to enable people to access care in different ways and support staff in the NHS to deliver better care. New digital technologies provide the opportunity to change the way in which services are provided, but also transform the way in which people access services.
We will support patients to manage their own health as they build on their knowledge and skills to improve their confidence.
We recognise that patients want better communication on time spent in A&E, want a better understanding of how to access the right care to avoid multiple handovers between services, and want greater continuity of care so that they do not have to repeat their story as they go through the system.
We will ensure that services reflect the needs of different groups of people, including all age groups, people with mental health issues and dementia and people with learning disability and autism. The plan takes proactive steps to tackle known inequalities, particularly for groups who are disproportionate users of UEC services.
The plan sets out how we will achieve headline ambitions of patients spending less time in emergency departments, and ambulances getting to patients more quickly.
While these ambitions provide an immediate focus, they are only part of the patient journey. We will also need to ensure focus across the pathway, including on long waits in emergency departments and on discharge, as we deliver this plan.
Achieving these ambitions in the next two years will be challenging. However, NHS England is committed to helping develop the leadership and capacity locally to drive the transformation. We recognise that delivering this vision will not happen overnight.
These two ambitions will be the first step in the transformation required to meet our ambitions for urgent and emergency care.
Over the next two years we will also take steps to ensure that urgent and emergency care is part of a more integrated health and care system building on the Fuller Stocktake report as well as improvements in access to general practice, details of which will be set out in the forthcoming plan.
Learning from experience on the elective recovery plan, this plan will be delivered locally through integrated care systems, working with partners, and supported by clear prioritisation at national and regional level.
Meeting this challenge will require sustained focus on the five areas in the rest of the document:
1. Increasing capacity
2. Growing the workforce
3. Improving discharge
4. Expanding care outside hospital
5. Making it easier to access the right care
NHS England has engaged with a wide range of stakeholders to develop the plan, and it draws on a diverse range of opinion and experience, as well as views of patients and users.
DHSC, who produced the content on actions being taken in social care, has led on engagement with the sector.
1. Increasing urgent and emergency care capacity
We will need to increase the number of beds and ambulances if we want to reduce time spent in A&E and ensure hospitals are not as full. We will also work to make the most of the capacity we do have, with better processes and faster spread of best practice. We will increase capacity and reduce waiting times through:
A. Additional hospital bed capacity
B. Increasing ambulance capacity
C. Improving processes and productivity
A. Additional hospital bed capacity
Ambition
There is a well-established link between high bed occupancy rates in hospitals and worse A&E performance.
When hospitals are busy, it becomes more difficult to ensure patients get the care they need and can lead to longer time spent in A&E. Worsening A&E performance in turn has a direct impact on ambulance handovers and response times.
We therefore need to reduce the current bed occupancy, which over 2022/23 has consistently been above 95%, back towards the 92% level which is safer and more efficient as it improves flow through hospitals.
Hospitals have tended to have higher occupancy levels in England compared to other countries, despite historically lower lengths of stay. The need for acute care will continue to increase over the coming years, and ongoing levels of COVID are creating additional pressures on hospital capacity.
While we will act across all parts of health and care, increasing the number of staffed hospital beds to lower our occupancy levels ahead of next winter will be a fundamental part of the plan.
Through the additional funding for this winter and through the year, the NHS has already increased the number of staffed hospital beds.
This increase in capacity is to be maintained for next year and we will also put in place further physical beds ahead of next winter. We are also exploring how to make better use of procurement to bring capacity on-stream quickly.
How we will deliver:
Compared to the originally planned levels of beds in 2022/23, there will be 5,000 more staffed, sustainable beds in 2023/24. This additional bed capacity needs to be in the places that will deliver the greatest benefit to patients and allocated in a fair way across the country.
Therefore, by April 2023, systems will conduct appropriate demand and capacity profiling to identify the areas with the greatest need. The results of this profiling will be used to ensure that any increase is aligned with other capacity such as staffing and diagnostics.
NHS England will work with local areas to ensure that the new beds are put in place as sustainably as possible, to reduce the impact of surge periods on other services, including theatres and research facilities.
Local systems will maximise the use of existing estate, where possible. Systems should also make use of modular buildings where possible, building on the additional funding announced this year, given that they provide flexible capacity and can be brought on stream relatively quickly.
The additional bed capacity will also better protect beds and other spaces for planned care, including those being delivered through NHS England’s Targeted Investment Fund.
B. Increasing ambulance capacity
Ambition
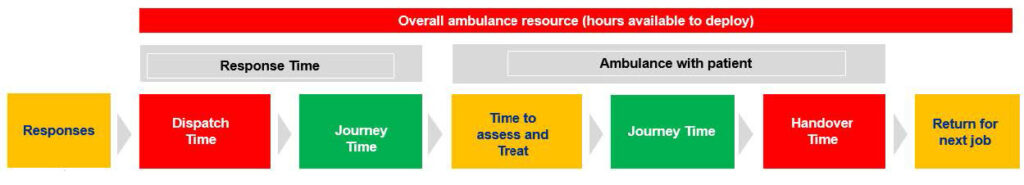
One of the main causes of longer waits for ambulances is delays handing patients over from the ambulance crew to hospital staff because the emergency department is full.
On average more than 4,000 hours a day were lost to handover delays this winter – time when ambulances could be back on the road, with significant variation across the country.
Therefore, on its own, reducing A&E waiting times will lead to an improvement in ambulance responses as flow improves out of, and therefore in to, emergency departments.
However, analysis of ambulance response times indicates that handover delays are not the only cause of slower ambulance response times. We have seen increases in sickness and other staff absence.
We have also seen the complexity of ambulance crews’ work increase meaning each incident is taking longer: the number of the most serious ambulance callouts has, at times, increased by one third since before the pandemic and there has been a long-term increase in the time ambulances are spending at the scene as crews provide more care directly with the patient.
Therefore, additional ambulance capacity, not just additional beds, is needed to meet next year’s 30-minute ambition for Category 2 ambulance response times.
The simplified ambulance flow diagram below shows the importance of handover times to ambulance performance, and the wider range of factors involved.
As well as increasing capacity, we need to ensure that ambulance services focus on emergency incidents and where ambulance services can add most value.
In some cases, it may be more appropriate for other services, including urgent community response or mental health crisis teams, to respond to patients on scene.
How we will deliver:
To respond to these pressures, grow the fleet and better support the workforce, NHS England will ask ambulance services and lead commissioners to determine, by March 2023, their capacity plans for 2023/24 and identify gaps.
As part of that process ambulance services will look at ways to reduce sickness absence and how additional support could be given to staff.
This additional capacity will be largely delivered through more crew hours on the road, but we will also release capacity through better health and wellbeing for staff meaning a reduction in sickness absence, productivity gains, and through better links between the ambulance service and community services.
Over 800 new ambulances are expected to be available during 2023/24, with the majority expected to be available ahead of winter, as part of ongoing improvement and replacement of our fleet, including 100 new specialist mental health response vehicles.
Capital investment over the next two years will also fund 150 new projects, supporting mental health crisis response and urgent mental health care.
The new projects include over 30 schemes providing crisis cafes, crisis houses and other similar safe spaces, as well as over 20 new or improved health-based places of safety which provide a safe space for people detained by the police.
NHS England will work with ambulance services and wider systems to increase capacity and ensure patients receive the most appropriate care, including:
- From April 2023, asking systems to ensure consistent and rapid access to clinical advice and alternative services, and to reduce unnecessary conveyance, by implementing single points of access for paramedics.
- Single points of access provide a single, simple route for referrals to hospitals.
- They are staffed by qualified clinicians, able to ensure patients get referred to the most appropriate service for their needs.
- By autumn 2023, increasing clinical assessment of calls in every ambulance control centre.
- This additional clinical input will ensure that the sickest patients are prioritised for ambulances and that patients who do not need a face-to-face response can be transferred quickly to services more appropriate for their needs, including urgent community response, urgent treatment centres, same day emergency care (SDEC) and primary care.
- We will work with the ambulance and community sectors to manage the electronic transfer of appropriate incidents, enabling quick transfer of patients to community services.
- Working with the sector to improve forecasting of call demand and further develop the ‘Intelligent Routing Platform’ to manage the distribution of calls throughout England when individual services are under pressure and therefore reduce 999 call answering delays.
As we increase capacity, we need to make sure that mental health patients are properly supported.
We will continue to increase mental health expertise for ambulance services, as set out in the NHS Long Term Plan, including ensuring that mental health professionals are embedded in all emergency operation centres ahead of winter, and improve training for ambulance staff to enable effective response to those in mental health crisis.
Example: Bristol, North Somerset and South Gloucestershire (BNSSG) ICS & partners, Emergency mental health dispatch pathway
BNSSG has partnered with the South West Ambulance Service, Avon and Wiltshire Mental Health Partnership and Avon and Somerset Police Constabulary to develop a multi-agency approach to supporting patients with urgent mental health needs.
Mental health professionals have been embedded in the Emergency Operations Centre (EOC), via the introduction of a mental health desk in March 2021, which was then expanded in January 2022.
An emergency mental health dispatch pathway has been developed so that all 999 mental health calls, whether they are police/fire or ambulance calls, are routed into the mental health desk. This allows partnership working to determine the most appropriate response to 999 calls.
When there are mental health professionals working jointly with ambulance colleagues in EOCs, more people with mental health needs have their needs met over the phone or are conveyed to more appropriate services.
By December 2022, approximately 65% of calls directly handled by the mental health desk could be managed over the phone, without the need for ambulance dispatch.
C. Improving processes and standardising care
Ambition
We know from patients how important it is to have a smooth experience in hospital, and to not experience too many unnecessary delays in situations like waiting for your test results or moving to a different part of the hospital.
There is still significant variation between processes in hospitals, showing an opportunity to learn from where things are being done best and have a less confusing experience for patients.
As we increase capacity, we will use existing capacity as effectively as possible by standardising processes so that patients get the right care at the right time, including when moving between organisations.
We will reduce variation in care when patients arrive at A&E, ensuring greater consistency in direct referrals to specialist care, and access to same day emergency care (SDEC) so patients avoid unnecessary overnight stays.
We will also standardise the first 72 hours in hospital so that patients are assessed, get any required scans, and start their treatment as soon as possible.
The NHS will continue to make effective use of ‘system control centres’ (SCCs). These pioneering centres use data to respond to emerging challenges and bring together experts from across the system to make better, real-time decisions.
They will ensure the highest quality of care possible for the population in every area by balancing the clinical risk within and across acute, community, mental health, primary care, and social care services.
The NHS will also work towards implementing new response time standards for people requiring urgent and emergency mental healthcare in both A&E and in the community, to ensure timely access to the most appropriate, high-quality support.
How we will deliver:
By April 2023, NHS England will establish a new improvement programme to support standardisation of care, working with clinical leadership to set out common principles for providers, including developing professional networks to support peer-to-peer learning and challenge, leadership and best practice.
This programme will be supported by national ‘improvement collaboratives’ as a mechanism for systematically adopting good practice.
NHS England will continue to support direct referral to specialty for patients, including for frailty, respiratory services and stroke. This direct referral will be enabled through personalised care plans, rapid access to hospital specialist advice and remote urgent assessment.
Same day emergency care (SDEC) means shorter stays for patients and fewer unnecessary delays to leaving hospital. Current pressures often mean hospitals need to use their same day emergency care staff and space for other emergency care.
NHS England will work with systems to spread best practice to ensure greater resilience ahead of next winter so that all hospitals with Type 1 emergency departments provide appropriate SDEC seven days a week with a minimum opening of 12 hours per day, including for medical, surgical and paediatrics as outlined in the ‘SAMEDAY’ strategy.
NHS England will set out priorities for local areas and acute providers in the delivery of acute frailty services and SDEC, both of which will support reducing avoidable admissions and provide smoother care for patients.
A new frailty commissioning for quality and innovation (CQUIN) incentive will support delivery of frailty services and link funding to quality improvement.
Paediatric early warning systems provide a consistent way of recognising deterioration in a child’s clinical status, enabling early intervention and referral to alternative services if needed.
NHS England will support national roll out of a standardised paediatric early warning system for all inpatient settings by June 2023, which will be expanded into A&E, community, ambulance and primary care services, to deliver a cross-system approach.
Example: South Tees Hospitals NHS Foundation Trust, improving processes with a frailty service within the emergency department (ED)
South Tees Hospitals NHS Foundation Trust (James Cook site) was one of eight sites across England who were part of a pilot to test a new FRAIL strategy to help establish and/or improve acute frailty services.
In October 2021, they developed a peripatetic model, based from the ED, which operates seven days per week across a 12-hour shift (7am-7pm).
Identification of frailty takes place at the front door by the triage nurse, and patients who score 5 and above, through the clinical frailty score, and who are over the age of 70 are highlighted to the team.
As a result, they see the most appropriate clinician earlier, therefore reducing their delay in the emergency department and most likely avoiding an admission (over 50% of patients are discharged home with no admission); and where specialty intervention is required, they also get this earlier.
Patients have reported positive feedback on the care they experienced within the ED and the support they received to get home quickly – and staff feedback has been equally positive, with recognition of the impact that the frailty team has had on complex discharge planning.
We will work with systems to provide streamlined pathways for mental health patients who need to remain in acute settings until their care can be transferred, with particular reference to better working with children and young people’s mental health services, working-age adults and older adults, including people with dementia.
This will be supported by access to 24/7 liaison mental health teams (or other age-appropriate equivalent for children and young people) that are resourced to be able to meet urgent and emergency mental health needs in both A&E and on the wards, within one hour and 24 hours respectively.
NHS England will work with integrated care systems to fully embed year-round the system control centres (SCCs) that were established this winter, ensuring that they become sustainable, and are appropriately resourced with autonomous clinical decision making.
Systems will work with local authorities and other partners to ensure capacity, including in care providers, is used effectively and that the NHS provides support where needed.
NHS England will work with systems to support implementation of digital tools that support decision making in near real time, including electronic bed management systems both in hospitals and across other health and care settings.
We expect the vast majority of trusts to have electronic bed management capabilities by summer 2023 and we will support all trusts to have implemented appropriate solutions by the end of the year. NHS England will also continue to develop and roll out the A&E Admissions Forecasting Tool.
2. Increase workforce size and flexibility
Ambition
NHS staff have faced immense pressures in recent years during the pandemic, and recovery will impose new ones.
The COVID pandemic showed the remarkable flexibility of our staff to step into new roles, but it has also led to fatigue.
While leaver rates reduced at the height of the pandemic, we are now seeing rates rise with vacancy rates at 11.8% across the NHS. Demand for NHS staff is likely to continue to exceed supply over the coming years without any action.
Staff in UEC have faced increasing pressures, often in time critical situations, which can be mentally and physically stressful.
Sickness absence rates are above average for many UEC staff. For example, sickness absence in the ambulance sector increased from 5% in March 2019 to 9% in March 2022, with mental health the most common reason for absence.
In addition, the leaver rate for paramedics has increased to 8.1% in September 2022 compared to 5.9% in September 2019.
Over the coming years, we will help staff by growing the workforce including with new roles, freeing up staff from the unnecessary burdens which they face in their day-to-day work, and allowing staff to work more flexibly.
We know that staff want to be able to provide the best care possible. Staff are not always able to deliver the standards of care that they would aspire to, which will have an impact on staff satisfaction and wellbeing. We will take immediate action to attend to the needs of staff to support health and wellbeing needs.
Delivering the ambitions in the plan will require not just an increase in workforce, but also a change in the way that people work and opportunities for people, including recently retired clinicians, to return to work.
We know that the scaling of out of hospital care requires rapid expansion of the community workforce and the development of more flexible and integrated teams, and that the junior doctors and nurses of the future will need experience and training in out of hospital care.
We also know that volunteers can play a crucial role delivering care, as seen so clearly during the COVID pandemic, and we want to further build on this in roles across health and social care.
How we will deliver
While all areas of the NHS workforce are under pressure, we know that there are specific areas of the UEC workforce which we need to expand. Further detail will be set out as part of the long-term workforce plan, to be published this spring, but we are undertaking further actions for this year:
- 111 clinical staff
- Starting from April 2023, we will launch a promotion campaign for working in NHS 111 and Integrated Urgent Care as a flexible option for clinicians, including returners.
- We will introduce more home working opportunities for all roles, including helping to spread the technology required.
- We will also provide a route for retiring or recently retired clinical staff, including by working with regulators to explore options for staff on the emergency registers.
- We will make recruitment easier in 2023/24 by reviewing the training and NHS Pathways licence requirements to ensure they reflect the skills and experience required and simplify and reduce the length of the training course where safe and appropriate.
- Paramedics
- We will continue to ensure that projected paramedic workforce gaps are mitigated through undergraduate student intakes, apprenticeships and a focused retention improvement plan, to be developed in agreement with ambulance services as part of the current planning process.
- Emergency medical technicians (EMTs)
- We will increase the numbers of EMTs in 2023/24 to support the planned expansion of ambulance capacity, with ambulance services developing plans based on local need.
- EMTs can respond to incidents or support paramedics on ambulances.
- They provide an entry route to the NHS and free up paramedic capacity to ensure the most efficient skill mix.
- We will increase the numbers of EMTs in 2023/24 to support the planned expansion of ambulance capacity, with ambulance services developing plans based on local need.
- Advanced practice
- We will continue to increase the numbers of advanced practitioners in priority areas including in emergency care.
- Advanced practice enables clinicians to take on expanded roles, supports the standardisation of same day emergency care and helps make the most effective use of multi-disciplinary teams.
- Mental health
- We will continue to expand the mental health workforce within UEC and mental health services.
- This includes clinical roles, such as ambulance mental health workers staffing specialist new vehicles, and innovative non-clinical roles such as peer support workers and lived experience practitioners.
- NHS Volunteer Responders programme
- We will relaunch this programme by April 2023, expanding its remit into social care.
- Health and social care providers should maximise the opportunities to use volunteers, including in the organisations themselves, and for supporting people in the community who are at risk of admission or recently discharged.
We will continue to develop the workforce mix in community services, including physiotherapists, occupational therapists, speech and language therapists and dieticians to support people to participate in daily living.
We will continue the development of advanced and consultant roles alongside the development of a strong and well-trained therapy and rehabilitation support and associate practitioner workforce. Details will be set out in the forthcoming NHS long term workforce plan.
NHS England is asking systems as part of the 2023/24 planning round to develop and implement integrated UEC workforce plans based on capacity and demand assessments in line with local population need.
These plans will need to consider wider out-of-hospital services, including community services such as rehabilitation, therapy and reablement, and community nursing.
Example: NHS 111 provider ‘Integrated Care 24’, Flexible roles for NHS 111 workforce
Offering a homeworking option to its staff means NHS 111 provider IC24 has opened up opportunities for people to work flexibly or return to the NHS.
Giving their staff the ability to work from home not only ensures a resilient and agile workforce but gives people with a disability or those who may wish to return to the NHS a way to do so.
It enables people to work within the service who may be a carer or who live in remote, rural areas, as well as improving staff satisfaction significantly.
IC24 provide services across the South and East of England, including the NHS 111 service and clinical assessment services.
As well as growing the workforce, we will support staff to work more flexibly. As an example, the digital staff passport allows for a more efficient and safe deployment of an agile and responsive workforce by reducing duplication of employment checks and mandatory training.
We will launch the new digital staff passport across early adopter sites in August this year. In the interim, local workforce sharing agreements continue to be used to allow staff to work flexibly across organisations.
We will also support trusts where there are opportunities for their staff to extend their capabilities across urgent and emergency care, including for example supporting more staff to order x-rays and blood tests.
NHS England will continue to support upskilling of staff across UEC, acute and community care to improve care for people with co-occurring mental health needs, people with a learning disability and people with autism, including ensuring the uptake of existing offers such as the Oliver McGowan training.
For our work to scale virtual wards, NHS England will develop a national workforce recruitment capacity and capability plan. This plan will include multi-disciplinary teams, including with training in frailty, access to specialist and consultant oversight required to deliver hospital level care at home, and the therapy workforce.
We will also promote working in virtual wards as a flexible option for staff, including returners with more flexible working opportunities such as rotations and working from home.
To support a more flexible workforce, we will reintroduce flexibilities that allow overseas health and care staff to work unlimited additional hours outside of their sponsor, for an initial trial period of six months, and will assess the use of this arrangement to inform a longer-term view on its effectiveness.
The Home Office will continue its plan to make the visa sponsorship system more straightforward for users and will continue their programme of work to deliver a fully digital end-to-end customer experience and a frictionless UK border by 2025.
The Home Office has already made significant changes, for example, all applications are now made online, many customers can use smartphones to provide facial biometrics (rather than attend a Visa Application Centre in person) to establish or verify their identity and it is enabling the reuse of fingerprint biometrics that have previously been captured.
Example: Tameside and Glossop Integrated Care NHS Foundation Trust, using a blended workforce, with access to digital technology
Tameside and Glossop Integrated Care NHS Foundation Trust created a community based blended workforce of medics, nurses and AHPs called Digital Health. This hybrid team works flexibly across a number of services to support patient care delivery throughout the UEC pathway.
For instance, the trust gave all their local care, residential and nursing homes a digital tablet to contact the Digital Health team virtually for advice instead of defaulting to 999 and, in many cases, the team attend the home to help deliver care.
Over the past four years, the trust has seen a significant reduction in inappropriate conveyancing to hospital from care homes.
Further, the same Digital Health team has been performing the ‘streaming’ function within the hospital’s ED (pre-triage) and since July 2022 has seen a 30-40% safe redirection of patients to alternative hospital services, reducing emergency demand.
3. Improving discharge
Although having more hospital beds and more staff will help, it is also important to make sure patients are not in hospital for longer than necessary. We know that long stays in hospital are not good for patients or their independence and can lead to poorer health and economic outcomes.
Discharge delays have increased significantly over the pandemic. This means many more patients are in a hospital bed longer than they need to be: compared to before the pandemic, there are 6,000 more patients staying more than a week in hospital.
Both delays in discharge processes and shortages of capacity in social care and community care are making it more challenging to discharge patients from hospitals and mental health services. There are currently around 14,000 patients remaining in hospital who no longer need to be there.
On average, around 24% of patients with delayed discharges are awaiting the start of home-based care, 16% are awaiting residential or nursing home placements and 24% are waiting to begin intermediate care.
To improve discharge there must therefore be an increase in capacity in step-down services (‘intermediate care’) and social care, especially domiciliary care. This requires sustained long-term investment, in particular in the social care workforce given the scale of vacancies in the sector.
This is why the government is investing up to £7.5 billion over the next two years, on top of previously committed funding to reform the adult social care system as set out in the ‘People at the Heart of Care’ white paper.
Improved processes also play a critical role in improving discharge: processes within hospitals and between hospitals, community services, local authorities and social care.
We will therefore improve discharge by:
A. improving joint discharge processes
B. scaling up intermediate care
C. scaling up social care services.
A. Improving joint discharge processes
Ambition:
As well as increasing capacity and improving the pathway within hospitals, we need to ensure that people are not in hospital unless they need to be and to improve the experience of patients when they leave hospital.
Discharge planning should begin when patients are admitted to hospital to ensure that people can get home or to a more appropriate setting as soon as possible, with services in place if needed.
We will work in collaboration with social care partners to ensure appropriate processes are in place to facilitate prompt discharge in NHS settings, including in community and mental health trusts.
These processes should include early access to senior decision-makers to ensure patients get specialist advice sooner, removing avoidable delay.
We will work with local government and the social care sector to ensure an integrated approach to building capacity, so that patients have rapid and reliable access to the joined-up health and care services they need when leaving hospital.
How we will deliver:
NHS England will continue to support implementation of the best practice interventions set out in the ‘100-day discharge challenge’ across NHS settings.
We have seen good progress so far, with the number of hospital process-related delays reducing by 25% since this approach was rolled out. This has now been extended to community and mental health settings.
One-off personal health budgets of up to £200 (£400 by exception) were developed as part of the NHS’s COVID response to allow people to pay for goods or services that support timely and safe discharge and cannot be provided through existing commissioned services. Local evaluations have shown benefits to bed days saved and patient outcomes.
All acute and community trusts should ensure that arrangements are in place, in line with NHS national guidance, to support the use of one-off personal health budgets where appropriate.
Systematic discharge planning between health and social care should start from the point of admission by identifying patients with complex discharge needs, setting an expected date of discharge, and working with families and carers to plan discharges.
Everyone admitted to an inpatient bed should, on admission, have an estimated discharge date. Systems for discharge planning and delivery need to ensure timely transfers of care throughout the week, including evenings and weekend.
Across the country, NHS trusts are developing integrated ‘care transfer’ hubs to ensure that patients who do not need a hospital bed are discharged in a safe and timely way, either to their home or to a place in which long-term care decisions can best be made with rehabilitation and recovery support.
The development of these hubs is supported by best practice guidance published in May 2022. While the local operations of the hubs will always need to be tailored to specific local services and arrangements, we will support teams to adopt, ahead of next winter, the core elements that we know are working in the most effective hubs, including:
- Clear plans for delivery, across all partner organisations, including agreed outcomes and data sharing arrangements.
- A shared process to work with patients, their families and carers, and all professionals from admission, with all staff (in and outside the hub) sharing responsibility for delivering safe and timely discharge. Hubs will be focused on the most complex discharges and working to ensure that any assessments for long-term care are not completed in an acute setting.
- Strong and shared leadership at all levels, with clear accountabilities and responsibilities. We know this works best where there is a clearly identified senior leader accountable for flow across all partner organisations.
- A multidisciplinary staff mix, including social workers, case managers and clinical staff co-located in each hub, who are empowered to make autonomous and accountable decisions that are respected across all partner organisations.
- Real-time evidence and insight into capacity and demand management planning across the local health and social care system.
Example: Sandwell and West Birmingham ‘discharge hub’
Sandwell and West Birmingham’s integrated discharge hub delivers an integrated service across seven days with a commitment from health and social care partners to cover 8am to 8pm, seven days a week.
Sandwell and West Birmingham’s integrated discharge hub also has a dedicated transport service, currently on a six-month trial basis.
This has transformed its ability to transport people home without delay and more cost-effectively, the alternative being waiting for a four-hour window via traditional transport arrangements.
Example: Walsall Manor Hospital discharge lounge
Walsall Manor Hospital has established a discharge lounge which has greatly supported in-hospital flow and safe and timely discharge for patients.
In 2019, a permanent physical space was allocated to the discharge lounge, staffed by a dedicated multidisciplinary team. The space has been designed to be homely and comfortable, to act as that bridge to home.
The trust’s commitment to the discharge lounge service means that the unit is fully protected and is never used as inpatient escalation bed capacity.
Throughout 2021 the team focused on improving pathways by identifying patients on wards who are close to being clinically ready for discharge and then working with ward staff to ensure the process is safe and timely.
In 2022 the discharge lounge also had its opening hours extended, now running 7am to 10pm on weekdays and 12-hour shifts at weekends.
Being discharged via the discharge lounge is now seen as the default pathway (unless there is a clinical reason not to), which has taken the proportion of ward discharges that leave the ward before 9am from about 6% to over 9%, and 23% of ward discharges now leave the ward before midday. This has benefits for patients across the whole pathway by improving overall flow.
Patient experience has been improved with services provided such as food parcels for patients being discharged and organising social support follow-up visits in patients’ own homes post-discharge. This also helps to prevent readmission and successful return home.
Better data across health and social care
From April 2023, trusts will start to consistently record the discharge-ready date for all patients in NHS data systems.
In addition to publishing data on overall numbers of discharges and delayed discharges, we will work with local systems to develop a new metric that measures the time from the discharge-ready date to the actual date of discharge.
We will publish the new data as soon as possible ahead of next winter following trialling and testing with local providers and patient groups, in support of collaborative action across the NHS, local government and the social care sector to improve discharge planning and capacity planning.
We will work with providers in mental health, learning disability and autism settings to make sure that we develop a metric that can help focus on reducing the longest stays.
DHSC and the Department for Levelling Up, Housing and Communities (DLUHC) will work with local government and the Office for Local Government (OFLOG) to ensure that discharge metrics are included in the wider set of metrics that OFLOG will publish from later this year to assess local authority performance.
The Care Quality Commission will also consider this metric as part of its new inspection and assessment of the performance of integrated care systems, and of local authorities in carrying out their adult social care duties under part one of the Care Act 2014.
DHSC and NHS England will also work with local systems to develop and publish data that provides clearer insights into the reasons for delayed discharges, so that these insights are reflected in local capacity plans.
This data will facilitate a focus on the combination of NHS and social care capacity needed for domiciliary care, home-based reablement, stepdown care and long-term residential care, together with the more specific capacity needed for people with more specialist needs such as those with dementia needs.
B. Scaling up intermediate care
Ambition:
NHS England has begun a programme of work to develop and pilot a new approach to intermediate care, working with local authorities and voluntary and community partners.
This expansion of ‘step-down’ care is designed to help people move from hospital into more appropriate settings for their needs, with the right wrap-around support for their rehab and reablement.
This needs to be accompanied by growing the workforce, to ensure that we can deliver more care packages and good flow through community beds where required.
As an example, for people who need physiotherapy to regain their muscle strength, assessments of any longer-term care needs would take place after this initial recovery period and could take place in the person’s own home.
Chapter 4 ‘Expanding care outside hospital’ further details action to bolster ‘step up’ care (designed to help prevent hospital and emergency admissions) and ‘step down’ care (supporting timely and appropriate discharge).
How we will deliver:
Six new ‘national discharge frontrunners’ have been announced, of which three will focus on intermediate care.
NHS England is also doing intensive work with two additional sites to test innovative approaches to intermediate care, including reablement and wrap-around care. These are in addition to the areas trialling similar approaches across the country and trying to better join up care.
Initial learning emerging from the frontrunner sites will be available by April 2023, as well as other areas across the country trialling similar approaches, which will support more widespread adoption and implementation during 2023/24.
By autumn 2023, NHS England will develop a new planning framework and national standard for rapid discharge into intermediate care, building on the learning from the frontrunner sites.
As part of this framework, NHS England will develop a national data collection to track delivery, alongside a minimum dataset for intermediate care and regional action plans to improve data quality.
C. Scaling up social care services
Ambition:
Alongside these improvements to discharge processes and intermediate care, local government, the NHS and the social care sector will work together to improve access to social care, with a particular focus on domiciliary care, supported by the Better Care Fund, additional social care funding and the government’s reforms to adult social care.
How we will deliver:
At the Autumn Statement 2022, the government made available up to £2.8 billion in 2023/24 and £4.7 billion in 2024/25 of additional funding to put the adult social care system on a stronger financial footing.
This will support an increase in capacity and improve the quality of and access to care for many of the most vulnerable in society. The funding includes:
- £1.6 billion over the next two years focused squarely on discharge. This will increase the ‘Better Care Fund’ to a record £10 billion by 2024/25, to help ensure people are able to leave hospital on time with the right care and support, freeing up NHS beds for those who need them.
- £1.1 billion over the next two years ringfenced funding as part of the new Adult Social Care Market Sustainability and Improvement Fund to deliver tangible improvements in social care capacity, workforce, care and assessment waiting lists, and fee rates, which the government will work with local authorities to ensure also further supports improving discharge where appropriate.
- £3.2 billion over the next two years through the Social Care Grant.
- The government is also allowing local authorities to increase the adult social care precept up to 2% per year in 2023/24 and 2024/25.
This funding comes on top of the government’s continued investment to reform adult social care, including to improve training and technology.
The government will set out further details as part of the Local Government Finance Settlement and guidance to local authorities in February. The government will work with local authorities and social care providers to ensure this funding will:
- increase social care capacity – providing more care packages to more people – in ways that have the greatest possible impact in reducing delayed discharge from hospitals.
- ensure local partners can plan services sufficiently far in advance and for providers to develop long-term workforce capacity plans.
- be used in ways that build on learning from evaluation of the impact of previous discharge funding
- allow local authorities, the NHS and the social care sector to streamline discharge, assessment and placement processes and help to free up greater social worker time and capacity. This will have particular benefit to patients who are likely to require a permanent care home placement or specialist housing placement, including some people with dementia and severe mental health needs.
This will require improved collaboration and data sharing across health and social care services to enable joint NHS and local authority capacity planning – identifying capacity requirements and discharge needs to target funding and workforce appropriately.
In addition to its current role in regulating and inspecting health and care providers, the Care Quality Commission will assess local areas’ performance in improving discharge through its assessment of integrated care systems and local authorities.
Growth in adult social care capacity is dependent on continued growth in the care workforce – both domestically and internationally.
- The government is running a national recruitment campaign, providing funding for local recruitment and retention activities and, through the Department of Work and Pensions (DWP), promoting social care careers to jobseekers.
- The government is investing at least £500 million so the social care workforce has access to high quality training and opportunities to improve their skills.
- Visa changes are already supporting significant additional recruitment, with 29,000 visa applications for care workers and senior care workers up to September 2022 (data sourced from the Migration Advisory Committee: annual report, 2022). The government will publish updated statistics on social care international recruitment in February 2023 and on a quarterly basis thereafter. This will help demonstrate the scale of uptake of this visa route, in line with the wider Home Office immigration system statistics.
- Regional international recruitment support hubs will be able to use this data to target areas that are most likely to benefit from international recruitment.
- New temporary workforce flexibilities will allow visa holders in the care sector to work more than 20 hours for an additional employer in the sector if they wish.
To support wider improvements in social care capacity, DHSC is establishing a new expert group. The group will start work in February and will bring together local government organisations, local authorities, social care providers and voluntary/charitable sector organisations.
In spring, the government will also publish its implementation plan for adult social care to build on the progress made so far in the ‘People at the Heart of Care’ white paper and ensure maximum benefit from the additional social care investment, especially in improving discharge.
4. Expanding care outside hospital
The challenge of recovering urgent and emergency services also presents an opportunity.
For decades we have known that many patients can receive better, safer, more convenient care outside hospital. We have seen in the pandemic the NHS’s ability to design and expand new types of care and provide better care in people’s homes.
We know that backing those models that have been shown to work can give a better experience for patients and avoid unnecessary admissions and improve discharge. We will do this by:
A. expanding and better joining up new types of care outside hospital
B. expanding virtual wards.
A. Expanding and better joining up new types of care outside hospital
Ambition:
People’s care needs can often be best met outside hospital. We know that up to 20% of emergency admissions are potentially avoidable with the right care in place.²
Care closer to, or at, home without the need for hospital admission is not only often more convenient for patients, but through timely access can help to avoid the deconditioning and prolonged recovery that can accompany a hospital stay.
Personalised care approaches such as supporting self-management, shared decision-making and one-off personal health budgets, alongside providing patients with the right information and support to make decisions, can enable them to manage their own care and avoid the need for hospital care for longer.
Community health services, including therapy services, help keep people well at home and in community settings close to home, and support people to live independently.
When community services are delivered in combination with personalised care, they can reduce pressures on hospitals and emergency services by supporting patients at home and in the community, as well as provide them with greater choice and control, leading to improved patient experience and outcomes.
Falls are the number one single reason why older people are taking to the emergency department, and around 30% of people 65 and over will fall at least once a year.
Care outside hospital is of particular importance for older people living with frailty, who are much more likely than younger people to be admitted to hospital, and likely to have a longer stay when they are admitted.
Through better joint working and sharing of information between services we can help improve care for people who fall or are living with frailty.
Continued focus on mental health crisis prevention and a joined-up community response will ensure people are accessing the best service for their needs in a timely way, reducing avoidable admissions to hospital.
Making use of new technology and better collaboration, including between ambulance services and community care, will enable care that would often currently be delivered in a hospital to be delivered closer to people’s homes.
For example, the use of ‘NHS @home’ approaches can support people to recover, keep well and manage their health and wellbeing at home, and help reduce the need for hospital care due to supported condition management at home.
Adult social care plays a vital role in working with health services to provide the community support that prevents unnecessary admissions.
Working in partnership with acute and community health services, the voluntary and community sector and care providers, local authorities will continue to promote wellbeing and prevent unnecessary hospital admissions.
How we will deliver:
Many people can be best supported by a quick response from services in their community. Urgent community response (UCR) teams provide urgent care to people in their homes which helps to avoid hospital admissions and enable people to live independently for longer.
Through these teams, people who urgently need care can get fast access to a range of health and social care professionals within two hours.
Ahead of next winter, we will improve use of UCR including consistently meeting or exceeding reaching 70% of patients referred within two hours, with a service that operates for at least 12 hours a day.
Continuing roll out will be achieved through national support and targeted funding, meaning an increase in referrals to UCR in winter 2023/24 and an increase in transfer of patients from ambulance to community services.
In addition to the planned £77 million for community health services in 2023/24, additional targeted funding to support UCR winter preparedness will be rolled out from this April.
The population has aged and has increasingly complex conditions, and so we will make sure services are better joined up – with healthcare that works for patients.
The NHS will immediately scale up falls and frailty services based on our learning from this winter, and help these services be better joined up with ambulances and existing UCR services so they can work together to provide a network of support for patients.
Local areas are developing plans to take this forward in the current planning round. Some of these will be based in hospitals, but they will bring together a range of new and existing services in the community to provide care where and when needed and avoid unnecessary admission to hospital.
The NHS will roll out adult and paediatric acute respiratory infection (ARI) hubs to provide timely access to same day urgent assessment, preventing hospital attendance and ambulance conveyances.
Our ambition is that each local area that would benefit from one has one in place ahead of next winter, learning from those already in place.
These hubs are integrated across primary, secondary and community care, and will be a key point of referral for, or to, virtual wards. Patients are identified through remote consultation as requiring face-to-face assessment but not requiring hospitalisation.
We will continue the transformation of community mental health services and build on the recent expansion of community-based crisis services to ensure that all systems have a range of open-access age-appropriate services which meet local population needs, alongside 24/7 Crisis Resolution and Home Treatment provision.
As part of this expansion, NHS England will undertake further evaluation of crisis assessment suites that have been opened in a number of areas as an alternative to emergency departments.
NHS England will support systems to build on the expansion of home treatment teams for people with acute mental health needs, with a clear focus on the quality of provision, underpinned by the use of technology and data to better manage and plan care.
The government is also investing up to £25 million to work with the sector to kick-start a change in the services provided to support unpaid carers, who play a vital role in supporting people’s health, wellbeing and independence.
Systems will continue to roll out high intensity user services, adopt good practice in supporting patients who are experiencing homelessness or rough sleeping, and embedding family support workers in A&E settings to provide additional support to children and families presenting with non-urgent issues.
High frequency users of services can also be supported to tackle social and practical issues that affect their health and wellbeing through working with social prescribing link workers, who can link them to a range of community assets depending on their needs and preferences.
This may include help to stay active, make social connections, and manage their health conditions.
Example: Integrated frailty service in South Warwickshire University NHS Foundation Trust (SWFT)
South Warwickshire University NHS Foundation Trust has created a frailty model, joining up hospital-based secondary care expertise and a dedicated assessment service with community nursing and virtual wards.
This provides an integrated service that aims to keep people with frailty safe and well at home, avoid hospital admission if possible, and provide a seamless transition to secondary care if it becomes necessary.
Ambulance crews are able to contact the Acute Frailty Service via Consultant Connect, whilst with the patient at their home, followed by a triage consultation with Consultant Geriatrician input.
The most suitable outcome for the patient is agreed, for example inclusion on a virtual ward for observation and monitoring and/or further face-to-face assessment by a consultant or community advanced clinical practitioners.
So far, this has led to a 50% reduction in ambulances conveying patients aged over 75 to ED and gives frail older adults an alternative to hospital admission. In addition, the Trust makes follow-up calls to all patients discharged over 75.
These calls provide an opportunity to see how the patient is, answer any questions they may have and have proven to reduce re-attendances from 15% to 3%. It also grows relationships with, and upskills, community teams.
B. Expand virtual wards
Ambition:
One example of better, more convenient care for patients is hospital care at home through ‘virtual wards’, which are bridging the gap between hospitals and patients’ homes.
Virtual wards combine technology and face-to-face provision to allow hospital-level care including diagnostics and treatment, using many of the same staff that work in hospitals.
In some cases, virtual wards can replace the need for admission, and in others facilitate people being able to safely leave hospital sooner.
Virtual wards enable patients to remain in their own home supported by family or carers to recover more quickly in a more comfortable environment.
The evidence base for virtual wards is growing, with clinical evidence to show that virtual wards are a safe and efficient alternative to NHS bedded care, particularly for patients living with frailty.
The NHS is currently developing virtual wards at scale through investment in community provision for conditions including frailty, acute respiratory conditions and heart failure.
The NHS has successfully rolled out 7,000 virtual ward beds, with capacity increasing by nearly 50% since the summer.
Our ambition is to scale up capacity ahead of next winter to above 10,000 with a longer-term ambition of reaching 40-50 virtual wards per 100,000 people, which would mean more than 50,000 admissions a month.
As well as continuing to increase capacity, we need to increase utilisation of virtual wards so we make more of the capacity we already have.
In the longer term as advances are made in ‘point of care’ diagnostics and remote monitoring, virtual wards will be a standard alternative to acute care in hospital across a range of conditions. We will work with royal colleges and clinicians to co-produce these pathways with patients.
How we will deliver:
We will have more virtual wards, better utilised, across a broader range of conditions, with less variation and so more people can receive high-quality care from their own home.
The NHS will scale up virtual ward capacity for frailty and acute respiratory infection, building on the evidence of what has worked well this year, to make sure that the offer exists for patients across the country.
Local areas have developed plans to deliver at scale. We will continue to work with clinical communities to drive growth in virtual ward admissions.
We will increase utilisation of virtual wards from around 65% to 80% by September 2023. ICSs will be encouraged to develop local clinical and operational teams to ensure standardisation across their area to enable referrals, build patient engagement and benefit from economies of scale.
The virtual ward programme is in its first year, and as local areas have tried different models, they have learnt about what works best for patients, and some have scaled faster or been utilised better than others.
Building on experience from GIRFT, NHS England will work with systems to establish a data-driven approach to peer review that supports implementation.
National and regional support will be provided through tools and resources to enable service review, clinical audit and approaches to diagnostics and tech enablement.
NHS England will support systems to implement new models of virtual wards, in more clinical areas, including for patients with a broader range of conditions.
Clinical advice on which areas are most appropriate for this expansion is currently being developed and clinically-led guidance and guidelines will be put in place to allow people to scale ahead of winter for priority pathways including heart failure and paediatrics.
We will support systems to build on the expansion of home treatment teams for people with acute mental health needs, with a focus on the quality of provision and therapeutic offer, underpinned by technology and data to better manage and plan care to avoid deterioration and unnecessary hospital admission.
Example: Central London Community Healthcare NHS Trust, Virtual Ward
The Wandsworth and Merton Hospital at Home team, part of Central London Community Healthcare NHS Trust, provides intensive hospital-level, holistic support for serious conditions, in a patient’s home.
‘Hospital at Home’ was one of the first community trust-led frailty virtual wards in the country. The initiative involves a team of healthcare professionals, made up of doctors, nurses and pharmacists, working together to make sure patients are managed by the right person, in the right place at the right time.
The team has quickly developed the skills to support more digitally enabled care, such as virtual assessments, heart rhythm testing and remote monitoring.
Since the initiative launched in December 2021, more than 310 patients have been directly accepted by the team from both the hospital and the community, with an estimated 2,134 hospital bed days saved between December 2021 and October 2022.
Going forward, it is estimated that this initiative will save just under 200 hospital days each month and improve patient experience of care.
5. Making it easier to access the right care
Ambition:
We need to ensure that the urgent and emergency care system is responsive to the needs of patients, and so people receive the right care in the right place, and in a timely way.
NHS 111 is crucial to this, and we know that it can reduce demand on emergency care and be convenient for patients, especially with clinical input and oversight.
But we also know that the percentage of 111 calls abandoned increased significantly this winter as pressures grew, and so we will need to provide more resilience to improve access for patients and reduce demand on UEC services.
Over the past ten years we have seen increased need for UEC services across all age groups and have heard in our engagement with patients that UEC services are complex to navigate.
We will make it easier for patients to access the care they need without feeling they have to go to A&E or call 999, and help make 111 online and calling 111 the first port of call so that patients can easily access the appropriate advice and be directed to the most effective care.
The Fuller Stocktake recommendations, and the widespread commitment to them, provides an opportunity for services to integrate closely with all parts of primary care, so that people get the care they need, regardless of how they contact services.
Many patients will need clinical advice, and we know that can make a difference to patients, and so we are looking to better use clinicians in 111 for the patients who will benefit most. New technologies should help people to get clinical advice and be directed to the most effective care.
Clinical advice to NHS 111 underpins our plan to assess and direct patients to the most appropriate point of care, whether that be self-care, pharmacy, general practice, advice from a paediatrician, mental health crisis centre, an urgent treatment centre, or another setting.
How we will deliver:
Over the pandemic we have seen the advantages of 111 online and we will further expand it through its continued promotion and development.
It will be further connected with other services to mean patients are better directed to the right place. We will work to integrate 111 online with the NHS App.
We know from our engagement the importance of 111 to families. The NHS will expand advice offered through NHS.UK and NHS 111 online to provide dedicated paediatric advice and guidance for families to support decision making around care options.
NHS England will review the NHS.UK webpage to identify opportunities to provide children and young people, parents and carers with robust advice to support self-care and management of illness.
We will roll out paediatric clinical assessment services to ensure specialist input for children and young people is embedded within 111.
NHS England will undertake an extensive review of 111 services, including intensive trials of ‘111 First’ following lessons learnt in the 2019 pilot.
It will test the models and their effectiveness at directing patients to the clinicians and services who can best meet their needs with the minimum possible delay.
This review will be aligned with priorities for primary care, including for community pharmacy, the forthcoming GP access recovery plan and implementation of the Fuller stocktake report.
The review will also explore the potential to incorporate advancements in technology, including AI and machine learning, within 111 services.
NHS England will work with ICBs to increase 111 clinical input where it will have most impact, including to confirm which care setting is best for the patient – providing better care for patients and reducing demand on emergency services.
We will ask ICBs during 2023/24 to commission the clinical assessment of a greater proportion of NHS 111 Category 3 or 4 ambulance dispositions.
Example: Bristol, North Somerset and South Gloucestershire, System Clinical Assessment Service, ‘System CAS’
The Bristol, North Somerset and South Gloucestershire system has established a system-wide Clinical Assessment Service (CAS) to remotely assess NHS 111 calls.
The CAS is staffed by experienced clinicians including clinicians with experience in general practice, integrated urgent care, paediatrics, mental health and emergency medicine who are able provide the most appropriate response and where necessary direct the patient to the best care for them.
As a result, they’ve seen real positive outcomes on patient care, including 94% of patients who would have received a Category 3/4 ambulance response being clinically assessed as able to have their care needs met elsewhere in the community.
Both patients and clinicians feel its benefits, with 93% of patients extremely likely or likely to recommend to friends and family, and 97% of clinicians would recommend working within the CAS due to the multidisciplinary approach, the ability to learn from others as well as welcoming more hybrid roles.
We will do more to support people to access mental health support. Urgent mental health support will be universally accessible by using NHS 111 and selecting ‘option 2’ by April 2024.
ICSs are now moving further ahead with their plans to sustain and enhance 24/7 open access, freephone urgent mental health helplines for all ages, and ensure these services are universally accessible using NHS 111.
This will be further supplemented by future provision of 24/7 crisis text lines, which ICSs will integrate into their local open access crisis pathways.
The Directory of Services enables referrals into the most appropriate urgent care service from 111 and 999, supporting better management of patients. A platform rebuild will make it easier for staff in the NHS to direct people to the appropriate services and supports faster innovation of new services.
Some patients that come to emergency departments would get better, quicker care if they are navigated to an urgent treatment centre. ICBs should determine where these will be most effective; this may be co-located with the local emergency department or a standalone service either on or off a hospital site.
We expect that decisions about all existing services should be concluded through 2023/24.
NHS England will work with stakeholders to agree consistent approaches for patients who walk into hospitals, which will support patients to be seen in the most appropriate setting.
Systems should ensure they have implemented streaming at the front door of ED, which will increasingly be through co-located urgent treatment centres or other primary care services.
Example: Lincoln County Hospital, Urgent Treatment Centre co-located with the emergency department
Lincoln Urgent Treatment Centre is co-located with Lincoln County Hospital’s Emergency Department and is open 24/7 365 days per year.
The UTC is a key part of the urgent and emergency care provision on site, acting as the front door to the emergency department and streaming patients to the right service for their individual care needs.
Patients are supported at the front door by a clinical navigator so that they understand what they can expect from the UTC and the initial clinical assessment.
The ICB has focused on UEC system working and building relationships – and the benefits are clear to see. On average, patients are seen, treated, and discharged within 2.5 hours, and 95% of patients have their initial assessment within 15 minutes (October 2022).
It has also meant that patient numbers attending the ED have decreased by approximately 20% (from 6000 to 5000 per month) with the UTC seeing around 3000 patients per month.
The trust is now working on a wider integrated urgent and emergency care transformation project to look at how technology can enhance our clinical assessment service (CAS) and enable UTCs to broaden their offer further.
6. Delivering this plan
We will deliver this plan by putting in place the fundamentals that are essential to successful local delivery: accountability at every level, genuine transparency, on-the-ground support, and mechanisms to spread good practice and innovation.
A. Accountability at all levels
Delivery of the UEC recovery plan will reflect the new NHS operating framework, with alignment through the national, regional and local level, including DHSC and local authorities to ensure full involvement of social care.
Integrated care boards (ICBs) will be accountable for delivery across health, able to draw together different partners and provide a cross-system view of the interventions required for delivery.
ICBs will be accountable for improving four-hour A&E waiting times and ambulance performance, through the services that they commission, recognising their links to all parts of the system that have an impact on UEC.
They will need to work with partners to agree ambitions for individual NHS providers, including stretch targets for those trusts ahead of target.
Acute trusts will be responsible for improvements in hospital handover delays and in-hospital flow.
Ambulance services will take responsibility for reducing operational variation, including working with partners to reduce conveyances.
Community providers and mental health trusts will be responsible for ensuring planned services are in place.
Local authorities will be responsible for ensuring sufficient capacity to enable flow into social care settings in line with agreed plans.
All partners will work together to improve flow through increased use of joint working such as care transfer hubs.
ICBs and local authorities will work with providers to undertake systematic capacity and demand planning, with the aim of understanding the expected levels of need for social care and intermediate care services in their local area and developing shared plans to meet this need.
This planning process will draw on real-time evidence and insight from care transfer hubs to allow local systems to plan for how expanded social care and intermediate care capacity will help reduce delayed discharges.
Delivery of local plans will be monitored by regional and national teams, providing oversight, support and intervention as appropriate to ensure delivery of the plans.
Local areas are currently developing their plans for delivering the performance ambitions on A&E and ambulances, delivery of which will depend on agreed planning assumptions.
B. Transparency
Transparent, high-quality data are important for improvement, providing insight across the whole journey but also identifying unwarranted variation.
To ensure greater transparency, more data will be made available to the public. This will be published by integrated care board area by April 2023, and new metrics to monitor the effectiveness of discharge will be put in place.
We will publish data on 12-hour delays from time of arrival in A&E from April, to support prioritisation of long waits as part of delivery. The public will be able to more easily see and compare the performance of their local services.
We will use data to help manage periods of high demand and increased pressure across systems and enable urgent system action. ‘Faster data flows’ will bring together data in a way that will reduce burdens on providers, and allow a more granular understanding of patient flow to support improvement.
C. Tiered intervention
Through national and regional teams, NHS England will work on the ground to support and challenge systems to deliver this plan. Intervention will be based on how far local areas are on track with delivery.
NHS England will identify and share good practice so that all can learn from the best. For those systems that are struggling, we will offer support to ensure that they have the best opportunities to drive improvement locally.
The support will include targeted executive leadership, clinical expertise and analytical insight. We will continue to develop the support offer to ensure it delivers what is required across both health and care, and that we focus on those interventions where national and regional action will have greatest impact.
Building on experience from elective recovery and improvement in ambulance handovers, NHS England is developing three tiers of intervention, to be in place by April 2023:
- Tier one: core offer – universal support offer for systems on track, including specialty guidance, peer review and sharing of best practice.
- Tier two: light touch – for systems largely on-track, support including regional reviews and deep-dives to diagnose challenges and drive improvement.
- Tier three: intensive support – for systems off-target on delivery, support including on-the-ground planning, analytical and delivery capacity, “buddying” with leading systems and executive leadership.
As with existing tiering arrangements these tiers will be reviewed frequently, and tiers will be publicly available information.
D. Reducing unwarranted variation
We will establish by April 2023 a complementary, clinically and professionally led programme to reduce unwarranted variation. This programme will increase standardisation of what works across different areas of urgent and emergency care.
This programme will be supported by a stronger approach to improvement collaborative development.
Building on the approaches of the Acute Winter Collaborative and Discharge ‘100 Day Challenge’, subject-specific improvement collaboratives will be established to co-develop across systems and share emerging good practice, drawing on teams of experts.
Working with DLUHC, the Local Government Association and the Association of Directors of Adult Social Services, DHSC and NHS England have developed an integrated approach to performance improvement and support in local systems, bringing together local leaders from across the NHS, local government and the social care sector to target support to the most challenged areas, and to rapidly identify and help spread innovative practice.
Tiered support to improve the adoption of fully integrated care transfer hubs across the country will help reduce variation across different systems. The government will work intensively with the most challenged local authorities to reduce delays due to lack of social care capacity.
E. Supporting innovation
We know that evidence is needed where innovative care is being developed.
Through the national collaborative, we will work with systems where an approach is being trialled and understand the benefits of scaling for spread and adoption, and work with systems to test the efficacy of entirely new models.
Early priority areas for further exploration include models of remote clinical assessment including rehabilitation expertise, intermediate care models and virtual wards.
NHS England will work with systems to develop the evidence on what works to enable informed decisions about where to prioritise local resource.
Acknowledgements
This plan has been developed with expert contributions from a wide range of partners, including but not limited to:
- A system reference group, including all integrated care boards
- An expert reference group including, but not limited to:
‒ NHS Confederation
‒ NHS Providers
‒ Healthwatch
‒ Age UK
‒ British Heart Foundation
‒ Stroke Association
‒ British Medical Association
‒ College of Paramedics
‒ Royal College of Emergency Medicine
‒ Association of Ambulance Chief Executives
‒ Royal College of Physicians
‒ Royal College of General Practitioners
‒ Royal College of Paediatricians and Child Health
‒ Royal College of Psychiatrists
‒ Society of Acute Medicine
‒ British Geriatric Society - Crowdsourcing with around 2,500 members of the public, including frontline professionals, such as doctors, nurses and allied health professionals, and patients.
We have also benefited from the insights and ideas of staff, including on enhancing staff welfare through the elective recovery process, and from contributions by clinical leaders and NHS provider organisations.
The Department of Health and Social Care has led on engagement for the social care elements of the plan, including with the Local Government Association and the Association of Directors of Adult Social Services.
We remain committed to working closely with partners as we deliver these plans, including through an engagement forum. Thank you to all the individuals and organisations who have shared their time, energy, expertise and experience so far.
¹This plan does not cover all actions to support primary care, which will be covered by the upcoming plan on access to general practice
² The Health Foundation: Emergency hospital admissions in England, Which may be avoidable and how?

