Glossary of Acronyms
AoMRC Academy of Medical Royal Colleges
CCT Certificate of Completion of Training
EDWL Enhancing Doctors’ Working Lives
DME Director of Medical Education
FPT Flexible Portfolio Training
GMC General Medical Council
HEE Health Education England
IMT Internal Medicine Training
LED Locally Employed Doctor
LTFT Less Than Full Time
MDRS Medical and Dental Specialty
Recruitment
MSC Medical Schools Council
NETS National Education and Training
Survey
NHSE National Health Service England
OOP Out of Programme
PGDiT Post-graduate Doctor in Training
RCEM Royal College of Emergency Medicine
RCoA Royal College of Anaesthetists
RCP Royal College of Physicians
SAS Specialty and Associate Specialist
UKFPO United Kingdom Foundation
Programme Office
WT&E Workforce, Training and Education
(Directorate)
Forewords
‘The Enhancing Doctor’s Working Lives (EDWL) programme recognises the significant importance of work and training systems on the lives of postgraduate doctors in training. Working with partners across the health system who share a vision for improvement, the programme has delivered a huge range of initiatives. This year we celebrate the expansion of the flexibility initiatives, improvements to the recruitment processes and initiatives to improve the training experience.
The bringing together of Health Education England and NHS England has provided the opportunity to reflect on the programme and consider what more we should be doing. We now have a responsibility for the workforce that covers doctors in training programmes, Locally Employed Doctors, Specialty and Specialist doctors and the consultant, Public Health, and GP workforce. Our future work will reflect this, building on both this programme and the work to deliver the People Promise to improve the working environment for doctors in the NHS.’
Dr Navina Evans CBE
Chief Workforce, Training and Education Officer, NHS England
‘With Health Education England and NHS England coming together to lead both healthcare education and training and the delivery of care from one organisation, it is great to see the work of the Enhancing Doctor’s Working Lives Programme and acknowledge our potential to do more in the new organisation.
I am looking forward to working with colleagues within the new NHS England Workforce, Training, and Education directorate to shape the future of this work within the new organisation we have become. Thank you to all who have contributed to the programme and this report. It is a helpful reminder to celebrate what we have achieved and set ambitious aspirations for the future.’
Professor Sir Stephen Powis
National Medical Director, NHS England
Note from the editors
‘On behalf of the NHS England Workforce, Training and Education (WT&E) Directorate, it has been our pleasure to produce this year’s Enhancing Doctors’ Working Lives report. In this report we highlight some of the improvements in this area of work that have been achieved over the past 12 months, building on the work of the last few years in Health Education England.
We would like to thank all the internal and external report contributors, and the organisations and committees represented on the membership of the working group for Enhancing Doctors’ Working Lives. As ever, we hope this year’s report is a useful and informative resource for doctors, educators and system colleagues.’
Dr Kavir Matharu and Dr Jack Haywood
Clinical Fellows to Professor Wendy Reid, Director of Education and Quality, WT&E Directorate of NHS England, and to Professor Stephen Powis, National Medical Director of NHS England.
Introduction and summary
‘The safe delivery of care by NHS services is dependent on a workforce of UK doctors in postgraduate training programmes. These doctors deliver essential care in community and primary care, in acute and mental health and Public Health and Local Authority settings. We need to value and support this workforce, especially after the impact of the COVID-19 pandemic. Over the last 7 years the Enhancing Doctors’ Working Lives (EDWL) programme has delivered improvements in medical education and training, aiming to have a positive impact on the wellbeing and working lives of doctors training in England.
As we explore the new ways to expand our work within the Workforce Training and Education Directorate at NHS England, we are pleased to share this annual update report highlighting some of the work of this programme during the last year.
Improving flexibility in training has always been a key theme of the programme, recognising that this is important for both wellbeing and retention. The expansion of access to Less Than Full Time training, Flexible Portfolio Training and Out of Programme Pause along with developments in the Supported Return to Training (SuppoRTT) programme enable a much more individualised approach to the training pathway.
The Medical and Dental Recruitment and Selection programme has continued its focus on improving the quality, consistency, and equity in recruitment processes and reducing the risks associated with human error, while evaluating the changes to ensure we build better processes.
The report details new and developing initiatives which support the delivery of more integrated and person-centered care and highlights those developed to reduce the impact the pandemic has had on training progression and wellbeing.
We continue to focus on the quality of training, informed by our National Education and Training Survey (NETS) and work to streamline processes for doctors and reduce the administrative burden in training rotations.
We know there is still much to do and will continue to work to find improvements that support doctors in training and positively impact their wellbeing.
I would like to thank the editors, the many teams whose considerable work is reflected in this report, our system partners and especially the many educators and supporting our training programmes and processes. Through their continued collaborative working we can improve education and training, enhance doctors’ working lives, and in doing so benefit patients.’
Prof Sheona MacLeod
Programme Senior Responsible Officer, NHS England (Workforce, Training & Education)
1. Flexibility
1.1. Less than full time (LTFT) training
Less than full time (LTFT) training and the option to take up this training have now been mainstreamed; there are no longer categories for LTFT, simply an indicative list. This means that all doctors in training can apply to work LTFT, but it ensures that we continue to comply with the Equality Act, give priority to doctors in training who have a protected characteristic, and broaden access to LTFT.
This is a major change as LTFT training was traditionally only available to those with caring or health needs (LTFT Category 1) or those with unique opportunities for personal development (LTFT Category 2). Responding to valued trainee perspectives, HEE introduced a new flexibility initiative in 2017: LTFT Category 3.
This allowed doctors in training to opt to train on an LTFT basis for an individual, professional or lifestyle need, only constrained by local service pressures.
This initiative was externally evaluated by RSM-UK, with the results demonstrating:
• an overwhelmingly positive impact on work-life balance – reported by 100 per cent of
doctors who trained LTFT Category 3 in year two and 99 per cent in year three,
• 86 per cent saying they are very likely to complete their training.
1,780 doctors trained under the auspices of the LTFT Category 3 pilot, and training LTFT for personal choice has now been embedded in the Gold Guide (the reference guide for Postgraduate Foundation and Specialty Training in the UK). Following a lead-in year in 2022-23, where Foundation doctors were able to apply to train LTFT Category 3 for a four-month period at 0.8 whole time equivalent, all Foundation doctors are now able to apply to train LTFT from August 2023.
Read our guidance on giving doctors in training greater flexibility.
NHSE led the development of new four-nation guidance to support the programme management of LTFT doctors in training, which emphasises the importance of individualised decisions at ARCP.
[There is] better morale within the whole cohort of doctors in training if [doctors in training] are happy in [the] workplace.
Head of school at a LTFT Category 3 pilot specialty
My general wellbeing, physical health and relationships have significantly improved.
LTFT Cat 3 doctor in training
My supervisor is aware that LTFT is exactly what I need to stay working in the NHS.
LTFT Cat 3 doctor in training, expansion specialty
1.2. Flexible portfolio training (FPT)
Flexible Portfolio Training (FPT) is a flexible, individualised opportunity within medical postgraduate specialty training to devote one day a week (or 20 per cent full time equivalent) to additional professional development that supports local educational, academic and service aims. There were initially four pathway options, each of which connected the trainee to different individuals, teams and networks that are not always visible in traditional, daily clinical work as a medical registrar.
These pathways were:
• clinical informatics
• medical education
• clinical service/quality improvement
• research
Having been run initially as a pilot with the Royal College of Physicians (RCP), after positive findings from an evaluation the programme has now been expanded so that from August 2023 FPT can be offered in all specialties across England.
Read our new guidance for doctors training in all specialties.
You get out of the scheme what you put in – if you make the most of it, you can follow your dreams and really achieve as part of the scheme. I think having more FPT posts available would be a great idea with the upscaling of the scheme. FPT has lots of benefits for trusts – it helps trainees gain experience and knowledge, allows trainees to follow their passion, and can be used to improve pathways and the patient experience.
FPT trainee on clinical informatics pathway
1.3. OOPP and recognition of training outside of training programmes
Out of Programme (OOP) is a key flexible training mechanism. Previously, doctors in training could step out of their training programme for research (OOPR), development experiences (OOPE), approved training (OOPT) or career breaks (OOPC). In 2019, HEE introduced a further option: the Out of Programme Pause (OOPP).
OOPP enables doctors in training, who have had at least two years of full registration with the GMC and are progressing satisfactorily, to apply for a new category of Out of Programme and undertake clinical work within a UK-based organisation, but without the training assessment burden. Significantly, any competencies gained during OOPP can be assessed on the trainee’s return to the programme and, if appropriate, counted towards their CCT. This differentiates OOPP from other forms of OOP.
The first phase of this initiative was launched in spring 2019, and because of the pandemic impact, it has now been extended until the end of July 2024, when a three-year external evaluation of OOPP is due to be published. Trainees in England who have two years’ post-full registration experience are eligible to apply for OOPP.
We are working to broaden this opportunity to allow for variable time out of training, depending on individual development, and for it to be an accepted part of the training pathway, while also expanding it across the devolved nations.
1.4. Supported return to training (SuppoRTT)
NHS England continues to fund this initiative, which helps remove – as far as possible – the
disadvantages to those who take time out of training.
Evaluations showed improved wellbeing, confidence and competence upon return to training. This provides an agreed, consistent, standard offer for returning PGDiT across England, which could include:
• coaching/mentoring
• accelerating learning/specialty-specific refresher courses including simulation/human factors
• enhanced supervision
• supernumerary working
• personal development courses
Local ‘Quality and Innovation Fellows’ in each local office work with local SuppoRTT teams. Over the last year, a ‘Building a More SuppoRTTive Culture’ eLearning module has been developed, which explores the significance of organisational culture in shaping the experience of postgraduate doctors in training returning to work after a break. It also offers guidance on the measures that individuals can take to bring about positive culture change.
Developed with contributions from experts in the field, such as Professor Michael West CBE and Professor Jim Barrie, the 40-minute session is an engaging, interactive learning resource, which includes videos and practical advice about improving the culture in your own workplace.
2. Recruitment and placements
2.1. Recruitment and reform of recruitment to medical specialty training
Medical and Dental Recruitment and Selection (MDRS) are running several workstreams to assess the fairness and effectiveness of recruitment with external partners (e.g. the GMC). The reform of recruitment will aim to make the processes fair for all candidates and increase flexibility of progression through postgraduate training programmes.
Specialty recruitment processes have remained digital while further analysis is undertaken to determine how recruitment should be delivered in the future. There are two projects currently underway: one is reviewing the complexity of the selection processes in operation, and the other is a statistical analysis of recruitment outcome data from 2021 and 2022. Both are due to report back in June 2023. Recommendations from these two projects will aid long-term decisions on specialty recruitment delivery.
Virtual recruitment offers many benefits to applicants, including (but not limited to) being able to attend multiple interviews on the same day and not having to travel. Prior to this year’s recruitment process, one of the limitations was not being able to hold multiple mini interviews in a virtual environment. Following a successful pilot in late 2022, a bespoke recruitment system has now been rolled out that has allowed many specialties to adopt a multiple mini interview process this year for the first time since before the pandemic.
An Application Programming Interface (API) has been rolled out to allow the transfer of scores between recruitment systems without the need for manual manipulation. This will reduce the risk associated with human error in the recruitment processes.
A systematic review of the Multi Specialty Recruitment Assessment (MSRA) has been undertaken, focusing specifically on equality, diversity and inclusion. A working group has been constituted to look at ways to operationalise the recommendations, with a full-length practice paper already having been created in response to doctors’ concerns when this was introduced into new specialties.
Future plans include developing a set of principles for person specifications that should ensure that only the required and assessed criteria are included.
Future considerations for specialty recruitment include advertising posts as less than full time
and reviewing the accessibility of all recruitment documentation.
3. Improving the quality of training
3.1. Training recovery
Following the major disruption to postgraduate medical training caused by the COVID-19 pandemic, the Training Recovery Programme was established to lead and drive a system-wide effort to mitigate the impact of the pandemic on the progression and wellbeing of doctors in training and their educators.
£22 million of new funding was invested in 2022/23 into bespoke and innovative solutions that were shared, adopted and adapted across specialties and geographies, setting the direction for future education reform. Interventions have provided trainees with the opportunity to catch up on competencies that were inaccessible during the pandemic, and to address wellbeing issues and reduce the confidence/competence gap, while aligning this activity closely with service delivery.
An Educator Toolkit was developed, informed by a series of national events with best practice examples and funding principles. This encouraged learning through the building of an accessible community of practice.
The training progression of England’s doctors in training continues to be critical to doctor wellbeing and to managing the significant NHS care backlog. We continue to support and evaluate the effectiveness of training recovery interventions to ensure the medical education and training pathway and wider medical workforce can develop, and can support full-service recovery.
There are several urological emergencies trainees rarely see but may be faced with as consultants. The course gave me excellent opportunities to go over open approaches to, for example, the ureter or to the kidney, which I don’t get to do often. It’s really invaluable to do this in a controlled manner with experts supervising, and it gave me a number of tips that I will use in the clinical environment.
Sophia, urology postgraduate doctor in training, East of England
I have attended a few courses [related to] sleep deprivation, stress and fatigue. They were very helpful, they definitely worked.
Trainee
Overall, [the wellbeing interventions] were helpful and the practitioner health programme was good. Such drawn-out period of time means that these were not fixes but they were helpful at the time.
Trainee
The sense that some of the educational endeavours are being invested in provides a degree of energy for trainers to keep going: people are burnt out but this helps to refresh everyone.
DME
[My] Trust has a fabulous medical education team, led by [the DME], who genuinely cares about us trainees, and our wellbeing is at the heart of everything they do with and for us. They deserve huge
EIA Survey quote
praise as they kept us all going with little disruption throughout the pandemic.
I feel I was fortunate enough to have access to a training infrastructure that supported trainees in their professional development and their wellbeing.
EIA Survey quote
3.2. Quality and patient safety
The 2022 multi-professional National Education and Training Survey (NETS) received an increased response, with 39,855 learners across healthcare professions taking part and sharing feedback on their experience of training across England. This included responses from 25,087 postgraduate medical and dental learners. The NETS reporting tool and a suite of reports are published here.
This year’s NETS describes a challenging situation for our learners, with increased levels of stress, burnout and feeling overwhelmed. We are working to address the concerns raised and the NETS 2022 National Key Findings Report provides examples of how the NETS feedback, both positive and negative, is helping to improve the experience of the current and future healthcare workforce.
Recognising the importance of hearing from educators, in 2023 we will start work to develop a survey for trainers and educators, supporting our recently published Educator Workforce Strategy.
We launched the first placement provider self-assessment to triangulate data on the quality of clinical education and training, and to encourage quality improvement. The first self-assessment report can be found here.
In 2022, HEE undertook a first national thematic review, focusing on cardiothoracic surgical training. This review was triggered by direct feedback to HEE, and by media reports raising concerns about the culture of the learning environment at two training units and the possibility that this reflected wider problems across England.
The required actions that resulted from the review include:
• HEE’s ongoing support with improvement plans
• training programme directors to promote completion of NETS by their trainees, to enhance
the evidence base for this small specialty
• visits to training units to seek feedback
• drawing on examples of good practice from other specialties and/or colleges; feeding back to HEE’s COVID Training Recovery Programme to support the specialty where able
We have launched Speak Up, Listen Up, Follow Up – a new e-learning package that is aimed at anyone who works in healthcare. Divided into three modules, it explains in a clear and consistent way what speaking up is and its importance in creating an environment in which people are supported to deliver their best. Importantly, this e-learning package is available to anybody, no matter where they work in health. Access is via the e-Learning for Healthcare Hub.
4. Cost of training
4.1. The cost of medical postgraduate training examinations
Specialty training presents significant financial pressures for doctors and, amid the cost of living crisis, several doctors reported difficulty, for example in undertaking exams, due to financial pressures.
The Academy of Medical Royal Colleges (AoMRC) Trainee Doctors Group (ATDG) has been exploring options for changing the way examinations are funded and further information will be published later this year.
4.2. Relocation / travel expenses
NHS England has a relocation and travel expenses policy, which outlines the claims PGDiTs can make when they have to move to begin a new post or are required to travel long distances as part of their day-to-day work.
Given that many doctors didn’t know about this, a communications campaign has begun to ensure doctors are aware of the policy, including a drive in summer 2023 for the August/ September 2023 rotation. We are also going to include details of the policy on Oriel job offer emails and letters, with links for further information if required.
Read the full relocation and travel expenses policy on our website, and take a look at our recently updated FAQs.
4.3. Study budget
The Study Leave Working Group was formed in 2018 in response to feedback that previous processes made access to the study budget difficult and inequitable. It serves as a national and centralised group with the main focus of addressing issues of operationalising NHSE’s approach to study leave. The working group is made up of Postgraduate Deans and external stakeholders (including Heads of Schools, Royal Colleges, AoMRC and trainee representatives) who meet regularly to discuss the study leave and budget policy, issues in interpreting this policy, and the impact of it on local systems.
This year the working group will explore how to improve consistency in the implementation of the policy across the country, and how to ensure doctors’ training needs are being met. It will also increase transparency in how study leave decisions are made.
5. Improving information systems
5.1. Trainee information systems (TIS) and trainee self-service (TSS)
We have launched the Trainee Self-Service (TSS) application to provide an improved and equitable experience for doctors when completing and managing some of the mandatory activities required as part of their training programme.
TSS currently provides an online Form R for doctors to complete for their assessments and has recently released an online Conditions of Joining Form for doctors to submit each time they start a new programme, in order to make the process of form filling easier for doctors and more efficient.
Our next focus is to digitise paper-based processes, making it easier for doctors to complete forms on TSS and helping to speed up the process time so that doctors then get faster responses. The first process we will look to develop is an LTFT application giving doctors an easier way to manage and apply for LTFT. There are other processes, such as OOP, that we will also look to develop. To help improve doctors’ training journeys, we are also looking to build the notification capability to remind doctors, who frequently have multiple sources of pressure, about upcoming events and to remind them to complete forms.
As TSS matures, we want to build a well-designed service that involves various users in the codesign of the application and really makes a difference.
Our vision is to make TSS the single national system for the doctors training service. As of May 2023, we have granted access to 39,000 doctors. To improve transparency and provide a common and simpler experience for doctors when applying for study leave, we have commenced a project to expand access to a system that manages study leave applications (these are typically managed by Trusts). This is a phased project currently covering 40 per cent of doctors in training.
We have been working to support the Digital Staff Passport, as part of the NHS-wide Enabling Staff Movements Programme, aiming to improve onboarding processes when postgraduate doctors rotate between employers. We have developed the capability for a postgraduate doctor to download information about their placement and programme from TSS onto their smartphone, which they can then share with their employing Trusts during their onboarding or induction process.
5.2. Digital staff passport
The Digital Staff Passport (DSP) aims to use technology to simplify staff movement between NHS organisations, as outlined in ‘We are the NHS: People Plan for 2020/21 – action for us all’. The DSP will enable the transfer of trusted information from one NHS employer to another.
The benefits include:
• better experiences – speed and simplicity, improving the onboarding experience for both doctors and HR, helping to increase job satisfaction, wellbeing and retention
• saved time and effort – spending less time repeating recruitment checks and verifying training requirements and hence removing barriers and inefficiencies
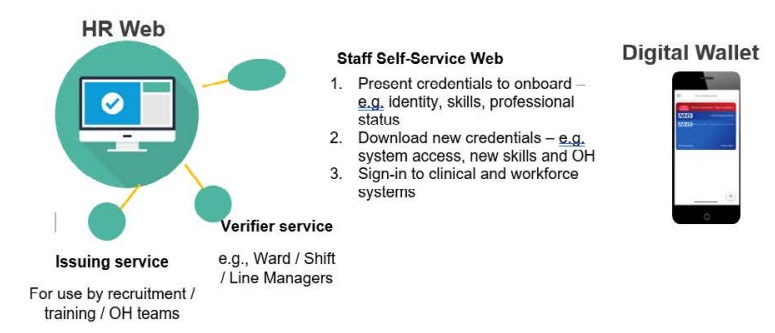
The NHS Digital Staff Passport operates across three integrated platforms shown below that can be accessed by all NHS staff who are involved in the process of staff moving between NHS organisations.
The DSP is currently under development and will be tested by a number of postgraduate doctors in training during the pilot phase later this year. The long-term goal is that every staff member in the NHS will hold an NHS Digital Staff Passport, to support them in their NHS employment and to facilitate a wider range of staff movements.
6. Individualised opportunities
6.1. The national population health fellowship
The National Population Health Fellowship, established in February 2020, achieved Royal Society of Public Health accreditation in March 2023, following an in-depth review of the learning programme. The fellowship provides a sustainable model for increasing the number of frontline healthcare professionals who have the skills and capabilities to:
• improve health outcomes for populations
• improve the wellbeing of populations
• prevent long-term conditions through population-level interventions
• reduce health inequalities and unwarranted variation in health outcomes
A third cohort began in September 2022, after expanding the eligibility to cover those from the wider workforce as well as GP trainees doing the fellowship as part of their training, and they will now be provided with added recognition through this accreditation.
Information on current projects is on the programme’s website.
6.2. Clinical artificial intelligence fellowship
Doctors in training have had a unique opportunity to undertake a Clinical Artificial Intelligence Fellowship. This integrated year-long programme, developed by the AI Centre for Value Based Healthcare, allows fellows to undertake immersive deployment-based AI projects, and to our knowledge it is the first of its kind globally. It is now in its second year with 17 fellows appointed across England.
7. Engaging with doctors in postgraduate training
7.1. GP specialty training (GPST) reform programme
A combination of an evidence review, place-based pilots and extensive engagement has led to the publication of the ‘Training the future GP’ report. This report outlines the importance of helping to best prepare GPs for future practice in different models of care, addressing health inequalities, and enhancing key areas of clinical practice such as mental health. Clear actions have been identified on enhancing generalist skills, equity in training, social accountability, improving quality of training, wellbeing, cancer detection, population health, technology in practice and leadership. This now moves to local implementation with matching of the doctor in training to population need. Through implementing these actions, we want to give GP trainees more control over their lives and work, and make training in general practice as worthwhile, rigorous in quality and future-facing as possible, to prepare learners for rewarding careers in primary care.
8. Thinking differently
8.1. Enhancing generalist skills srogramme (‘Enhance’)
Enhance is a universal development offer designed to augment the generalist skills of healthcare professionals across England. Over the last year, Enhance has been delivered to more than 250 learners through seven regional trailblazer sites and has supported the delivery of more integrated, person-centred care.
Local design and delivery has ensured the programme aligns with the needs of the learners, service and population. In the sites at Gloucestershire and at North East and Yorkshire, multiprofessional programmes in association with third sector partners cultivate cross-system relationships alongside learning. In the Midlands, East of England and North West regions, specific trainee groups of Foundation doctors and Internal Medicine trainees have been provided with bespoke programmes and allocated time to align the Enhance syllabus with their current interests and future aspirations. Some of this work can be viewed through champions videos.
The national educational offering has evolved as the trailblazer sites have progressed. The wellbeing and transformative reflection resource guides have been released to excellent response.
The upcoming release of the digital guide will have an emphasis on the critical appraisal and championing of digital health innovations through a digital mindset, whilst the leadership guide acknowledges the work of The Messenger Review with a focus on equality, diversity and inclusive leadership, in addition to the healthcare professional as a steward for the environment, an advocate for change and a leader at every career stage.
The year one evaluation of the programme is underway and will be published in August. Trailblazers will continue to expand in the coming year, fostering increasing engagement with Integrated Care Systems and furthering access to Enhance for all Foundation doctors.
It’s been inspiring to know what else I can do in my practice in future to improve the life of patients beyond just the knowledge of their diseases.
London Enhance participant
“I want to pinch myself – I can’t believe I am being given the time and space to think differently.”
North East and Yorkshire Enhance participant
We are talking about the opportunity to nurture some of the most prominent global and national health doctors to lead us into the future.
Midlands Enhance faculty member
8.2. NHS staff and learners’ mental wellbeing commission wellness inductions, wellbeing guardians, and mental health disclosure and support / NHS staff and learner mental wellbeing commission
The HEE NHS Staff and Learner Mental Wellbeing Commission was published in February 2019. This informed and enabled the rapid NHS staff wellbeing response to COVID, including support packages, staff safe and rest spaces, and a Samaritans-style service for the NHS. Board-level Wellbeing Guardians have now been introduced in more than 90 per cent of Trusts, with responsibility for board-level leadership on employee wellbeing.
Professional Support and Wellbeing Services (PSWS) have continued with a more open practice for accessing services, with the opportunity to self-refer becoming a commonly used option over the pandemic that continues to be used by some doctors. Various online wellbeing services are offered, for example mindfulness and yoga, and the option to access was extended to educators who may have also become isolated compared to pre-pandemic.
This year we have provided the first local office Guidance on Neurodiversity to create consistent assessment and support for doctors in training and have been engaging with other organisations including the GMC, MSC, and AoMRC, to bring about a more consistent and joined up approach for doctors.
Over the next year we will be launching a train the trainer programme on Neurodiversity for educators and doctors in training to then cascade across all regions. This aims to increase both recognition of neurodiversity in self and others and knowledge about how to signpost and access available support.
HEE/NHSE National Medical Director’s clinical fellows have supported this work through the identification and dissemination of good practice.
9. Milestones for the year ahead
9.1. Scope and purpose of EDWL as we enter NHSE
As of 1st April 2023, HEE has merged with NHS England and a new Workforce, Training and Education (WT&E) Directorate has been formed. This provides us with an opportunity to expand the scope of the Enhancing Doctors’ Working Lives programme to include our Locally Employed Doctor (LED) colleagues and to explore the needs of Specialty and Specialist (SAS) doctors, consultants and GPs.
We will also work with the wider system to promote action to address the many basic factors in the working environment that benefit the lives of all doctors, such as rest areas, access to hot food out of hours, and much more.
9.2. Self-development time (SDT): the benefits and provision
Self-development time (SDT) is the provision of protected non-clinical time for engagement with development activities.
As part of the Foundation Review, it was recommended this time be created and used for activities including reflection, e-Portfolio input, preparing/delivering teaching, quality improvement, or career exploration. This was successfully implemented in the Foundation Programme, and has proved very beneficial to trainees. Foundation doctors and educators in the North West Foundation School were surveyed, looking at whether foundation doctors had been receiving their SDT time. While there was some discrepancy across different Trusts, there was also a difference between the foundation doctors’ experience and the educators’ perceptions; it was reported that educators thought access to SDT was easier than the foundation doctors reported.
Similar schemes are seen in specialty training in general practice (Self-Directed Learning) and in psychiatry training. Emergency medicine trainees have Educational Development Time. The Royal College of Anaesthetists fully support and have been promoting educational development time, and the Royal College of Paediatrics & Child Health developed a ‘supporting professional activities’ document which has been helpful for the provision of SDT.
The AoMRC is exploring in greater depth the successes and challenges of providing self development time and will use the case studies derived from this work to encourage further engagement and provision.
Case Study
Self-Development Time (SDT) at Buckinghamshire Healthcare NHS Trust (BHT)
In 2021, a PGDiT and the Director of Medical Education (DME) at BHT developed and implemented a self-development time (SDT) policy across all grades and specialties. Agreement was sought from multiple stakeholders including clinical leads and operational and financial teams during the development. The policy was based on guidance from the UKFPO* and Royal Colleges (including RCEM*, RCP* and RCoA*).
|
Grade
|
Time provided
|
|---|---|
|
Foundation Year 1
|
2 hours per week
|
|
Foundation Year 2
|
2 hours per week
|
|
Core Training
|
2 hours per week
|
|
Higher Training (including IMT Year 3)
|
4 hours per week
|
NB these hours are pro-rata for LTFT PGDiTs
The Trust took a pragmatic approach to SDT, encouraging PGDiTs to use it flexibly and productively to benefit their personal development, career progression and quality improvement objectives. The SDT policy has also been an important lever in ensuring parity of access for Locally Employed Doctors.
The introduction of SDT has been well received by all Doctors, who reported that “SDT has been phenomenally useful”, with colleagues finding that “It’s been a fantastic way for me to be able to get good quality QIPs done and study for exams”. There has been particular success in Medicine & Emergency departments, where all PGDiT respondents had received their self-development time allowance in full. Proactive support is provided for the small number of departments struggling to implement the policy, and clarifications have been made following feedback.
9.3. E-rostering
E-rostering refers to the use of electronic software to view and manage rotas. Utilisation of these systems can enhance PGDiT working lives through the use of features such as accessing a rota through a remote application, live rotas, acting as a single source of truth, and automatic approval of leave and swap requests.
E-rostering can also facilitate new approaches to creating and managing rotas that allow greater flexibility of working hours for PGDiT. Approaches include the creation of personalised rotas through the use of self-rostering, annualisation, and self-preferencing. The use of personalised rotas is being used in a small number of trusts already.
NHSE has collaborated with the EDWL programme to increase awareness of e-rostering and its functionality amongst doctors through the use of webinars. Future work will focus on seeking doctors’ opinions on the functions that matter most, and encouraging software developers to create rostering programmes that prioritise these features and maximise the benefit to PGDiT.
9.4. Inter-deanery transfer (IDT) process
The National Inter-Deanery Transfer (IDT) process was initially established to support medical trainees who have had an unforeseen and significant change in circumstances since accepting an offer of a post in a training programme. In August 2022 the National IDT process was expanded, and a new Criterion 5 was introduced. Criterion 5 allows trainees to apply for a transfer for any reason without having to demonstrate any change to personal circumstances.
To increase the number of vacancies and therefore the number of transfers that can happen, the implementation of facilitated direct swaps has been introduced. This will allow two eligible trainees, who are in the same specialty at the same training grade within complementary regions, to swap.
NHSE continues to work with trainee representatives to review the process and open up the process further with improvements for future IDT rounds.
9.5. Flexibility in training oversight group
A Flexibility in Training Oversight Group (FTOG) has been established with stakeholders to further develop the flexibility initiatives and explore new models of flexible training. Over the next year the group will work to develop new initiatives in flexible portfolio training, to consider new training opportunities for example with industry partners, and to broaden the out of programme opportunity to make it an accepted part of the training pathway so that many more doctors can have competencies gained outside training programmes counted to CCT when they return.
The Workforce Training and Education function in NHSE will also explore how to support progression in alternative career pathways and support individuals to access training and assessment opportunities, such as short term posts to benchmark their progression.
10. Equality, diversity and inclusion
This key element of all our programmes is not specifically covered here as this was brought under closer oversight when NHSE’s Postgraduate Deans established an Equality, Diversity and Inclusion Committee in 2020, committed to considering all the issues raised in multiprofessional education and training, in line with the HEE Quality Framework.
An inaugural report, detailing how we can learn from examples of existing good practice, as well as plans for future Quality Improvement, was published in January 2022 with a further annual progress update report published in 2023.
Acknowledgements
We would like to thank the following for their contributions to this report:
Hatim Abdulhussein – National Clinical Lead of Artificial Intelligence and Digital Workforce,
NHS England
Maslah Amin – Associate Clinical Director, NHS England
Matthew Clarke – Chair of Academy Trainee Doctors’ Group, Academy of Medical Royal
Colleges
Jonathan Corne – Postgraduate Dean, NHS England
Dr Melanie Coulson – Postgraduate Doctor in Training, Bolton NHS Foundation Trust
Charlotte Dainter – Improving Employment Models Lead, NHS England
Dr Marc Davison – Director of Medical Education, Buckinghamshire Healthcare NHS Trust
Dr Diluxshy Elangaratnam – Lead Education Fellow, Buckinghamshire Healthcare NHS Trust
Simon Gregory – Medical Director, Primary and Community Care and Freedom to Speak up
Guardian, NHS England
Jon Hossain – Postgraduate Deputy Dean, NHS England
Helen Harth – Education & Training Policy Manager, NHS England
Richard Higgins – Quality Transformation Manager, NHS England
Jonathan Howes – Programme Lead for National Recruitment & TIS, NHS England
Rose Jarvis – Director of Education and Quality, Academy of Medical Royal Colleges
Dr Mark Johnson – Medical Registrar, Buckinghamshire Healthcare NHS Trust
Emma Jones – Head of Portfolio for Quality, NHS England
Joanne Marvell – Head of Education Policy & Regulation, NHS England
Tahreema Matin – Associate Clinical Director, NHS England
Andrew Milner – Programme Manager, NHS England
Andrew Sharman – NHS England Graduate Scheme, NHS England
Ruth Silverton – Clinical Fellow, Enhance Programme, NHS England
Geoff Smith – Postgraduate Dean, NHS England
Cathrina Tierney-Reed – Delivery and Improvement Lead, NHS England
Nicholas Turner – National Medical Director’s Clinical Fellow, NHS England
Kieran White – Senior Project Manager, Medical Education Reform, NHS England
Claire Wright – National Specialty Recruitment Manager, NHS England

