What is the purpose of this publication?
This publication is designed to support organisations in improving how enhanced therapeutic observations and care (ETOC) is provided and managed.
It focuses on how to use ETOC data to understand current provision, improve workforce deployment and enhance patient safety. As part of this, the guide outlines 10 core ETOC metrics.
It has been co-produced with clinical leaders to contain guiding principles and good practice examples in key areas that contribute towards effective ETOC.
Background
Demand for enhanced therapeutic observations and care – often called enhanced care, 1:1s, cohorting or specialing – has been increasing, predominantly due to an ageing population and greater health complexities. Nursing leaders have emphasised the need for clearer guidance on best practice for delivering effective ETOC.
In September 2024, NHS England launched a multi-year ETOC programme to support trusts make local, clinically led, patient-centred improvements to their ETOC provision. This aims to:
- improve patient experience and support our most vulnerable patients by promoting therapeutic, safe care and ensuring the workforce is effectively engaged, trained and deployed
- embed good governance processes to ensure effective oversight on the delivery of care to patients, and plan for future demand and efficient staff deployment models
- support wider NHS England commitments to promote sustainable, safe staffing models that drive forward high-quality care and improves workforce efficiencies, including reducing temporary staffing costs
For further information and resources, please join the Nursing Directorates ETOC FutureNHS page (FutureNHS login required).
ETOC strategy
Working with nurse leaders, NHS England has co-developed a programme strategy focusing on high-quality, patient-centred ETOC.
Through testing with key stakeholders, we have identified the following 4 pillars that systems are looking for support with to achieve this:
- effective leadership and oversight
- effective, person-centred and safe therapeutic care
- effective education and training of staff
- effective workforce planning and deployment
Each pillar has been supported by a co-design advisory group to develop this improvement resource, with the aim of helping organisations with their ETOC provision.
The diagram below outlines what the system has told us links to good-quality ETOC and what support the system needs to make these 4 pillars effective.
Diagram 1: Strategy overview
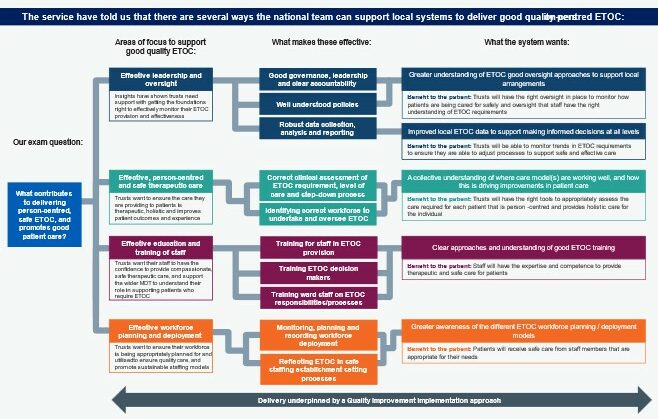
This diagram shows how national support for local ETOC systems flows from left to right through 3 stages:
- Focus areas: Leadership, commissioning frameworks, staff training and workforce management.
- Effective practices: These include governance structures, needs assessment, staff training programs and workforce planning.
- System outcomes: Each focus area leads to specific improvements, including better oversight, data-informed decisions, consistent training and appropriate staffing models.
Each outcome includes a patient benefit, such as better monitoring of service delivery, safer care processes, person-centred support and appropriately skilled staff.
The elements interconnect rather than existing in isolation. For example, effective leadership supports appropriate training, while good workforce planning depends on strong leadership and commissioning.
All activities are underpinned by a quality improvement transformation approach to deliver better patient care.
ETOC data improvement
Across the system, we have consistently heard about the importance of effective oversight in improving ETOC delivery models and transforming insights into ETOC drivers.
An area of particular focus is data reporting and analysis and how it can be used locally to improve decision-making to support improved workforce deployment and enhance patient safety.
This guide has been designed to:
- support the development of a core set of ETOC metrics with clear inclusion criteria, definitions and an explanation of their benefits and potential outcomes
- provide guiding principles for local data collection, including real-world examples from organisations that have successfully implemented these practices
- offer examples of local reporting and governance to ensure effective oversight of ETOC from ward to board
Core ETOC metrics
While local variation in data collection is inevitable, 3 essential components allow greater insight into an organisation’s ETOC provision:
- ETOC demand
- workforce deployment
- clinical quality intelligence
By leveraging these components, organisations can use ETOC data intelligence to assess clinical and workforce risks, patient safety impacts and financial implications.
This insight provides a comprehensive view of care quality and enables proactive decision-making to enhance workforce planning and deployment (as outlined in diagram 2 below).
Diagram 2: Data-driven approach to ETOC provision
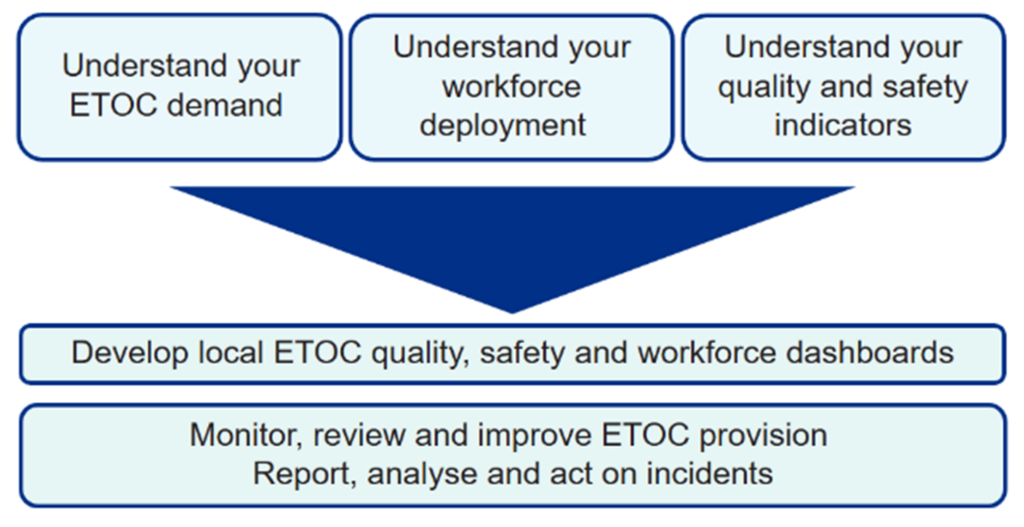
This diagram shows how the 3 essential components (understanding ETOC demand, workforce deployment, and quality and safety indicators) provide the basis for developing local ETOC quality, safety and workforce dashboards. These help organisations:
- monitor, review and improve ETOC provision
- report, analyse and act on incidents
Getting started
- Establish a network of local stakeholders to ensure a collaborative approach to ETOC metric development. Key stakeholders could include operational leaders, e-rostering teams, temporary staffing, finance, HR, health informatics, corporate nursing, and performance and improvement teams.
- Engaging a diverse stakeholder group from the beginning ensures effective guidance and supports data quality verification, triangulation with other sources and informed decision-making. This leads to continuous data improvement.
- Establish and capture data metrics that integrate both manual and electronic records.
- Develop dashboards using system builds that consider interoperability across various data reporting fields.
- Apply a quality improvement methodology, such as NHS Impact, to ETOC data quality projects. Clinical leaders highlight this is fundamental.
Data collection considerations
Before collecting and reporting the core ETOC metrics, it’s important to ensure effective safe staffing and workforce planning processes are in place.
Core ETOC metrics explained
Inclusion criteria
It’s helpful to define the types of care that fall within the ETOC umbrella. The following definition or inclusion criteria may help to ensure all aspect of ETOC are considered:
Enhanced therapeutic observations and care include care requiring a higher level of intervention, supervision and support (including continuous, within eyesight or within arm’s length observations).
This may be required due to the patient being at risk of either injury or harm to themselves* or to other patients or staff.†
*for example, due to a fall, self-harm, deteriorating mental health condition, physical health deterioration requiring more frequent observation, emotional dysregulation or behavioural disturbances, dementia, substance misuse, delirium secondary to a mental health or organic presentation, and absconding.
†for example, physical violence, damage to property or equipment.
Our clinical leaders developed 10 core ETOC metrics. These are broken down into the 3 components (ETOC demand, workforce deployment and clinical quality metrics), providing a definition, reason and methods for collection.
When reviewing the below metrics, please refer to the above inclusion criteria and consider registered and non-registered workforce groups where appropriate.
ETOC demand
Please refer to the inclusion criteria and include registered and non-registered workforce groups.
1. ETOC demand
Definition
Total number of hours unfilled and filled by substantive or temporary staff for all aspects of ETOC.
Reasons for collection
An assessment of demand will enable organisations to review trends, hot spot areas, plan, benchmark and forecast for the future.
Methods of collection
Aggregated total of filled substantive hours, filled bank hours, filled agency hours and unfilled hours. See workforce deployment for more details about collection.
Case study – establishing a live dashboard using ETOC demand data
Manchester University NHS Foundation Trust has taken all their ETOC data elements and several other safety and quality metrics to establish a live dashboard.
In consultation, a local agreement was made on a core data collection and desired analysis and reporting format.
The data collection was sourced from multiple sources, including workforce deployment systems (substantive, bank and agency), NHS Professionals reporting (bank and agency), SafeCare dataset (number of patients receiving ETOC) and incident reporting system (unfilled ETOC and patient and staff incidents).
At the time, the trust was unable to report volume and frequency of ETOC activity, so they developed an electronic patient record (EPR) report and a Power BI dashboard to combine this data and establish an ability to monitor on a ward or even patient level.
The dashboard can be accessed by all tiers of nursing staff.
The added insight resulted in the ability to monitor ‘high use areas’, the primary reason for ETOC (such as falls risk, confusion or mental health condition) and the type of ETOC initiated (such as 1-to-1, security, bay tag).
This identified potential and actual areas of variation, such as:
- ETOC risk tool not aligned to outcomes (trust is underway with research of clinical risk assessment tools)
- escalation and de-escalation delays
Known high-use areas have been identified from each hospital to be part of the ETOC wards pilot.
Workforce deployment
Please refer to the inclusion criteria and include registered and non-registered workforce groups.
2. Substantive hours
Definition
Hours of substantive staff time spent providing ETOC to patients meeting the inclusion criteria, including dedicated ETOC team if appropriate.
Reasons for collection
Organisations can effectively understand their staffing demands, themes and trends, including what clinical areas are managing well and what clinical areas require further support.
Methods of collection
Organisations can calculate their ETOC substantive staffing in several ways. Some organisations include ETOC staffing in their substantive numbers, some have dedicated ETOC teams, and others have some ETOC staffing provision in their establishment while the rest is used by temporary staffing.
All the above data items can be collected from a manual system or through electronic means, such as HealthRoster.
Case study – calculating substantive hours
Sandwell and West Birmingham Hospitals NHS Trust have budgeted ETOC staffing for wards with frequent use.
This was determined through a workforce planning process that included twice-yearly establishment reviews.
Using their workforce systems, the trust can calculate substantive staff hours.
3. Bank hours
Definition
Number of hours bank-only staff, or substantive staff if doing shifts on a secondary bank contract, spend providing ETOC to patients.
Reasons for collection
Organisations can effectively understand their staffing demands, themes and trends, including what clinical areas are managing well and what clinical areas require further support.
Methods of collection
The number of bank hours used can be gathered from internal bank records, where staff have undertaken a shift designated as ETOC provision.
Additionally, where organisations use external services, such as NHS Professionals, can capture their bank hours by using a unique code.
4. Agency hours
Definition
Number of hours agency staff spend providing ETOC to patients.
Reasons for collection
Organisations can effectively understand their staffing demands, themes and trends, including what clinical areas are managing well and what clinical areas require further support.
Methods of collection
The number of agency hours used can be gathered from workforce records on agency request and use, based on local policies.
This can be from a manual or automated record (EPR or organisations using HealthRoster) where the agency resource was requested and coded for a specific ETOC allocation.
Some organisations have seen a benefit from coding for role type, such as registered mental health nurse (RMN), which allows for further analysis of demand, deployment and any unfilled need.
Case study – using coding to collect bank and agency hours
Maidstone and Tunbridge Wells NHS Trust collect and monitor their bank and agency data on a weekly basis.
This data is gained from HealthRoster where the reason for use of this resource has been designated ‘ETOC’.
They have added a specific ETOC code to HealthRoster and removed ‘not specified’ and ‘other’ from the reason options to improve the accuracy of recording.
The coding has also allowed for reporting on a role, bank, agency and ward basis to monitor demand and combinations with patient and staff incident reporting and the organisations wider use of ETOC outside mental health situations.
The trust noted discrepancies between finance (monthly) and HealthRoster (shift date) data when first looking at improving data collection.
They decided to use the HealthRoster data, with its higher accuracy, to understand the need for ETOC and identify high-spend areas.
5. Unfilled hours
Definition
ETOC unfilled staff hours (staffing request not filled).
Reasons for collection
Organisations can effectively understand their staffing demands, themes and trends, including what clinical areas are managing well and what clinical areas require further support.
Methods of collection
This can be collected via either manual or automated roster systems, where a request is made and is unfilled due to the absence of a planned substantive resource (such as sickness or uncovered annual leave) or the lack of available temporary staff (bank or agency).
Additionally, SafeCare can offer the opportunity to “red flag” instances of unfilled hours which cause unmet need in advance of the occurrence or allow the provider to monitor trends.
Case study – tracking unfilled hours through incident reporting
Birmingham and Solihull Mental Health NHS Foundation Trust is tracking unfilled hours using incident reporting.
Where an ETOC need is unmet, this is logged as an incident.
The accuracy of the hours is assured by cross-referencing the incident log with SafeCare reporting and a record of unfilled hours reported.
Additionally, tracking where bank or agency backfill was not possible to address the unfilled hours (direct ETOC need or ETOC substantive or dedicated team sickness), is another way to record and assure the unfilled hours.
6. Dedicated ETOC team
Definition
If your trust has a dedicated ETOC team, the number of hours they have spent providing ETOC to patients.
Reasons for collection
Organisations can effectively understand their staffing demands, themes and trends, including what clinical areas are managing well and what clinical areas require further support.
Methods of collection
Where a dedicated ETOC team has been established, the number of hours can be gained from the local electronic staff record system and rostering system where appropriate role and team coding has been completed.
Case study – harnessing data on a dedicated ETOC team
East and North Hertfordshire NHS Trust has a dedicated ETOC team. They use HealthRoster to provide a daily view of available ETOC team staffing.
On a ward basis, the ETOC team establishment figure is compared with the ETOC demand (number of patients receiving ETOC) and the level of additional temporary staff for the next day ascertained.
This allows for flexible management based on the actual requirements, reducing temporary staffing to a minimum.
Additional factors, such as red flags and recommendations from acuity tools and SafeCare, are included in the consideration of the most appropriate staffing level.
To ensure accuracy, unfilled hours are taken into consideration, and the count adjusted accordingly.
All the above data items can either be gained from a manual system or through electronic means such as HealthRoster.
Clinical quality metrics
Please refer to the inclusion criteria.
7. Number of patients receiving ETOC
Definition
Number of patients requiring ETOC during any point of their care, including in A&E.
Reasons for collection
Understanding the number of patients receiving ETOC will mean organisations can better manage future demand and ensure adequate workforce is available and deployed to ensure quality and safety are maintained.
Methods of collection
This can be taken from manual referrals and care plans or patients coded on the electronic patient record (EPR) receiving ETOC.
Data can be triangulated with sources such as patient moves from referral to patient list and active care plans for accuracy.
Case study – collecting and using the number of patients receiving ETOC data
Royal Devon University Healthcare NHS Foundation Trust uses its EPR system to collate the total number of patients receiving ETOC.
Patients referred for ETOC are firstly categorised under local criteria and recorded appropriately on the EPR, which then feeds to an approval workflow. Approved patients then feed to a live dashboard of patients by criteria.
A suite of EPR reports enhances the consideration of this metric by combining other data elements such as reason for referral, referrals requiring a registered mental health nurse (RMN), declined ETOC details and patients by ward.
From this single metric, it has also been easier to monitor the average length ETOC is required and clinical causes of ETOC, such as delirium and associated falls.
8. Safety incidents associated with a lack of ETOC provision
Definition
Number of reported incidents when a patient is identified as requiring ETOC, but there is no available staff to provide this level of care.
Reasons for collection
Understanding the safety incidents associated with a lack of ETOC provision, broken by type of incident, level of harm and frequency, will mean that organisations can analyse and triangulate against other sources and take appropriate action.
Methods of collection
This can be taken from manual or electronic incident systems, such as Datix or Ulysses. Organisations may also request that staff record when safety incidents are associated with a lack of ETOC provision on their incident reporting system.
9. Patient safety incidents during ETOC
Definition
Number of incidents reported that involved a patient receiving ETOC.
Reasons for collection
Understanding patient safety incidents during ETOC, broken by type of incident, level of harm and frequency, will mean that organisations can analyse and triangulate against other sources and take appropriate action.
Methods of collection
This can be taken from manual or electronic incident systems, such as Datix or Ulysses. Organisations may also request that staff record when patient safety incidents happen during ETOC on their incident reporting system.
10. Staff incidents during ETOC
Definition
Number of incidents reported that involved a member of staff providing ETOC.
Reasons for collection
Understanding staff incidents during ETOC, broken by type of incident, level of harm and frequency, will mean that organisations can analyse and triangulate against other sources and take appropriate action.
Methods of collection
This can be taken from manual or electronic incident systems, such as Datix or Ulysses. Organisations may also request that staff record when staff incidents happen during ETOC on their incident reporting system.
Case study – learning from incident reporting
Frimley Health NHS Foundation Trust have enhanced their incident reporting to include 2 additional questions:
- was the patient under ETOC at the time of the incident?
- was an appropriate staffing resource in place?
This approach ensures data is collected about safety incidents that happen due to lack of ETOC provision, as well as patient safety incidents and staff incidents that occur during ETOC.
This has allowed the trust to triangulate the incident reports with unfilled hours data.
Leaders are now able to interrogate the incidences and review patient safety impacts and the learning, if necessary, through a policy-driven governance loop.
Case study – streamlining reporting
The Leeds Teaching Hospitals NHS Trust, through its Violence and Aggression Training Programme, recognised that incident reporting (for patient and staff) during ETOC delivery was low and did not represent the actual level of incidents.
The team streamlined the reporting system by replacing text entry with drop-down menus and checkboxes in consultation with ETOC delivery teams.
This has led to a 3-fold increase in reports and greater data assurance.
Reporting, monitoring and oversight
Our clinical leaders report good quality ETOC data collection, reporting, and the subsequent monitoring and oversight is a shared responsibility across the provider from ward to board.
Establishing the escalation, frequency of monitoring and thresholds for escalation will enable a consistent approach and continuous improvement that drives forward quality care.
These processes should also be aligned to the Patient Safety Incident Response Framework.
Diagram 3: Local example shared by Frimley Health NHS Foundation Trust of their local ETOC data process underway:
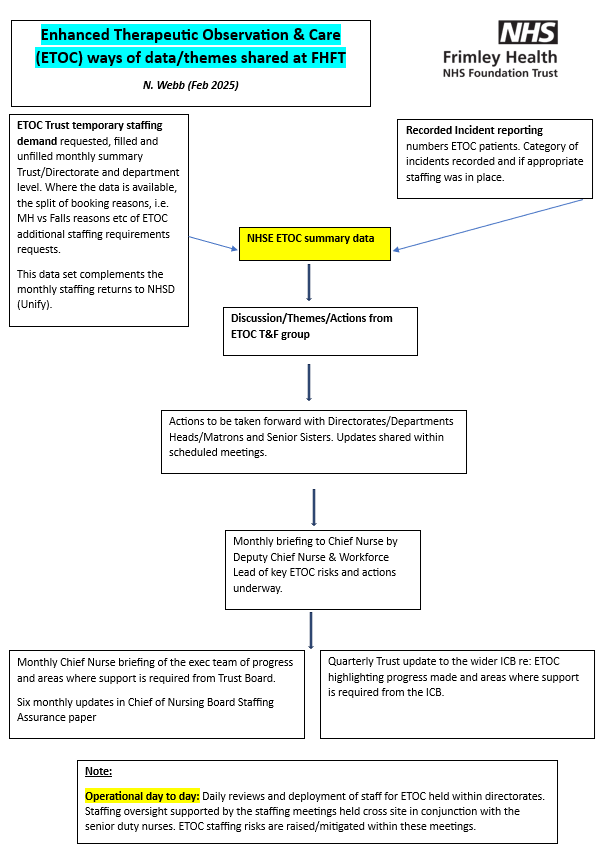
This diagram outlines how data on ETOC is shared and used within Frimley Health NHS Foundation Trust (FHFT). It is taken from February 2025.
Key points
1. Data collection:
- ETOC trust temporary staffing demand is recorded monthly, including filled and unfilled positions, at a trust, directorate and department level.
- Incident reports track ETOC-related patient incidents and whether appropriate staffing was in place.
2. Data summary and discussion:
- NHS England ETOC summary data consolidates this information.
- A task and finish group reviews trends, discussions, and actions needed.
3. Decision-making and reporting:
- Actions are shared through scheduled meetings with directorates, department heads, matrons and senior sister roles.
- The deputy chief nurse and workforce lead briefs the chief nurse on key ETOC risks and actions.
- The chief nurse updates the executive team on progress and any support needed from the trust board. Update in Chief of Nursing Staffing Assurance paper every 6 months.
- The trust provides quarterly updates to the integrated care board on progress and areas needing support.
4. Operational oversight:
- Daily staffing reviews ensure ETOC risks are identified and addressed.
- Cross-site staffing meetings, involving senior duty nurses, help manage workforce deployment effectively.
Classification: Official
Publication reference: PRN01862

