To:
- Integrated care board (ICB) chief executives
- ICB medical directors
- ICB chief nursing officers
cc:
- Dame Lesley Regan, Government Women’s Health Ambassador
- Royal College of Obstetricians and Gynaecologists
- Faculty of Sexual and Reproductive Healthcare
- Care Quality Commission
- NHS England regional:
- chief nurses
- medical directors
- directors of finance
- directors of commissioning
- directors of public health
Dear colleague,
Improving abortion care
We are writing to you to set out the NHS’ objectives and vision for abortion services, with the aim of improved access and care for all women who need abortion services.
Abortion care is an essential service. More than 200,000 abortions were performed in 2021, and the Office of National Statistics reports that more than 1 in 4 conceptions resulted in abortion that year, a record high rate for England and Wales[1].
These services are currently under great pressure. Demand has increased to unprecedented levels: up 17% in the first 6 months of 2022 (the latest published data).
National Institute for Health and Care Excellence guidelines state that patients should get assessment within a week of request and procedures should be completed within a week of assessment (NG 140). As a result of significant service pressures, providers tell us wait times for surgical abortions (circa 13% of procedures) do not meet these standards – often being 3 weeks or longer[2].
This is an important issue for everyone who needs these services – including some of our most vulnerable patients. A small but important number of service users will have experienced crime, including rape, domestic abuse, coercion, modern slavery or sexual exploitation. In addition, those living in the areas of highest deprivation are twice as likely to use these services.
Integrated care boards commission the majority of these services, with the independent sector delivering about 80%, mainly through 2 charities: MSI Reproductive Choices and the British Pregnancy Advisory Service. In the past 7 years, Care Quality Commission inspections have surfaced quality and leadership issues requiring national intervention and support at these providers.
There is some evidence that some contractors are being funded below the level of core costs (particularly for surgical procedures) and the overall position highlights significant continuity risks given the small numbers of providers we rely on.
The nature of the abortion sector means that there are national and regional risks if the fragility we are seeing in services is not addressed.
[1] Where conception does not include miscarriages or illegal abortions
[2] MSI UK Quality Account 2022/23
Actions for integrated care boards (ICBs)
We are requesting ICBs work with system partners and providers (and through existing commissioning boards and networks) to take the following actions by the end of July 2024:
- Agree and adopt appropriate local referral pathways and procedures to ensure smooth transfers of care between independent and NHS providers when required.
- Establish shared plans with trusts and independent providers to respond to cases of acute service disruption and instances where rising wait times risk limiting access to services.
- Ensure that contracts for 2024/25 are sustainable and follow guidance in the NHS Payment Scheme (Guidance on currencies section 2.2). Where contracts are pending for the current year, these should be agreed in line with the guidance as soon as possible. We believe the guidance will ensure commissioners strike the right balance, paying realistic prices that reflect costs and ensure sustainability.
- Commission in alignment with the vision in annex A and update NHS England on forthcoming tendering exercises, considering where services should be commissioner-requested services.
National action to support systems and improve care
NHS England regional teams will be working with you to implement steps to stabilise provision locally.
Local commissioners have said they want greater support from NHS England, including clarity on our objectives and joint work to address shared challenges. Today, we are sharing a vision for the sector (annex A). This includes a goal to maintain and increase NHS surgical provision to strengthen resilience and help tackle prolonged waiting times for those accessing these services.
We are also sharing case studies of improvement (annex B). Both the vision and the case studies are based on conversations with local teams. NHS England will continue working with systems on rolling out women’s health hubs, many of which will provide greater access to contraception. We will continue specialised commissioning work to develop a network of trusts in every region to deliver care for those with medical complexity in their abortions, and we will engage with you on opportunities to grow the surgical workforce. We will also work with independent providers to collect data on the financial costs of abortion care to support the continued development of prices in the NHS Payment Scheme.
Next steps
We will continue to contact integrated care boards (ICBs) about what we can do to help and we request that you nominate a point of contact for your organisation by emailing TOPS.nhse@nhs.net.
NHS England will shortly ask systems for an update on commissioning arrangements and progress against these actions in the summer (a similar exercise was conducted earlier in 2023).
Further details will be shared with you in the coming weeks.
We understand that services are under intense pressure and that systems are facing acute financial challenges. However, we know you will agree that high quality abortion services are a vital part of the NHS.
Thank you for the work your teams do to ensure these services help thousands of people every day.
Yours sincerely,
Steve Russell, Chief Delivery Officer, NHS England
Professor Janice Rymer, Consultant Gynaecologist and National Speciality Advisor for Gynaecology, NHS England [2019-2023]
Annex A: Objective and vision for the abortion sector
Objective
Improved access and care for all those who need abortion services
Vision
- A more managed and collaborative approach between independent sector providers and the NHS to meet and manage demand, including coordination of provision at the most appropriate geographies to bring wait times in line with National Institute for Health and Care Excellence standards, expanding training to ensure we grow surgical skills and improve access to services.
- Appropriately funded, financially sustainable services supported by an NHS Payment Scheme that promotes sustainability for both independent and NHS providers.
- Commissioning practices that support sector resilience and development, promote quality and collaboration, and take a whole-pathway approach to sexual health and abortion services.
- Enhanced NHS provision, workforce training and support, particularly in relation to surgical abortions, to create additional capacity within the system and meet patient needs.
Annex B: Cases studies of improving abortion services and promoting sector resilience
These case studies set out examples of how integrated care boards, trusts, and independent sector providers have taken action to address local challenges with abortion services.
If you would like to share examples of good practice, or would like more information on any of the case studies, get in touch: TOPS.NHSE@nhs.net.
Case study 1: Commissioning for quality and resilience
West Yorkshire Integrated Care Board (ICB)
Abortion services in West Yorkshire are delivered by a number of providers: MSI Reproductive Choices (MSI), British Pregnancy Advisory Service (BPAS), and National Unplanned Pregnancy Advisory Service (NUPAS), in addition to services offered by the NHS.
Commissioners and quality leads at West Yorkshire ICB have worked with these providers to develop a range of plans and pathways to improve experience and quality of care for abortion patients in the system. This includes the development of a quality improvement plan for services, to enhance accessibility, ensure quality and safety, reduce waiting times, improve patient experience, strengthen communication in the system, and increase the uptake of long-acting reversible contraceptives.
West Yorkshire leads have developed the plan to be robust. It is linked to Care Quality Commission domains, sets out specific actions for ICBs and providers, and outlines monitoring arrangements and the identification and ongoing reporting of quality improvement metrics. This includes the development of a dashboard for which all providers must report all clinical incidents and complications, to enable system improvement and learning from adverse events.
As part of this focus on quality improvement, work is also underway to reduce out-of-area travel for patients and manage acute service disruptions. To reduce out-of-area travel, the ICB is working collaboratively with providers to ensure geographical spread of services, set benchmarks for reducing out-of-area travel, and expectations around responsive service adjustments if demand requires clinics to be amended for out-of-area patients. A shared contingency agreement, standard operating procedure, escalation tool and pathway are also being developed to provide guidance on managing acute service disruptions, setting out clear responsibilities for ICBs and providers for ensuring the safe and timely management of termination of pregnancy surgical lists during unexpected disruptions. As well as improving the quality of services, the ICB aims to improve the resilience of abortion services in West Yorkshire through these initiatives.
The ICB has also been capturing data for a demographics dashboard. It is interactive and provides anonymised but highly segmented data. Commissioners use the dashboard to understand the needs of their population and – by working with other system partners (primary care, local authority commissioners) – develop targeted approaches to meet patient needs across the whole abortion pathway.
Working with providers (both independent sector and NHS) to develop plans to improve the quality of care can be a basis for encouraging collaboration between abortion providers. Collaboration can help providers manage demand across a footprint, ensure a smooth transfer of patients, and improve patient experiences and outcomes.
Case study 2: Surgical training collaboration between independent providers and the NHS
South West region
National shortages in the surgical abortion workforce are leading to capacity pressures. This is particularly the case at later gestations, where there is increased clinical risk. In the South West region, the independent sector has been working with the NHS to address these workforce shortages and this has increased surgical capacity.
In 2021, MSI Reproductive Choices UK launched a training curriculum to teach qualified professionals to perform later stage gestation surgical abortions. 10 doctors have either completed or are nearing the end of the training.
These trainees represent a range of clinical backgrounds. Many have specialised in obstetrics and gynaecology, some are sexual and reproductive health trainees, and some are already delivering abortion services and want to expand their provision to offer services up to the legal limit.
The first surgeon to be trained has gone on to become the lead clinician for the South West Complex Termination of Pregnancy Network. The network is hosted at North Bristol NHS Trust and has been commissioned to provide abortions for patients with significant medical or surgical complexity. Its main aim is to ensure patients who require an abortion receive it as close to home as safe and practicable. It provides care across 6 counties, stretching from Gloucestershire to Cornwall.
Good collaboration between the NHS and the independent provider sector can relieve pressure on services. By expanding the clinical workforce, we can improve sector resilience, increase patient access and improve experiences.
Case study 3: Integrated approach to commissioning sexual and reproductive health services, and abortion services
Sussex Health and Care Integrated Care System (ICS)
Rising demand for abortion services is a national challenge that commissioners and providers are having to respond to. Some systems, such as the Sussex Health and Care Integrated Care System, have worked to understand the local drivers for increasing demand and assess the needs of their local populations, which has helped support a targeted approach to service delivery.
In Sussex, ICB commissioning leads have collaborated with Sussex local authorities, public health, GPs, and local sexual health and abortion providers to analyse data across abortion and wider sexual health pathways. The aim has been to identify which services have the highest levels of demand, who is accessing them, and what is driving demand.
The ICB’s data analysis shows a strong correlation between deprivation and the use of abortion services. There is a similar correlation between deprivation and demand for long-acting, reversible contraception and emergency hormonal contraception prescriptions, although demand for these services has not matched the increase in demand for abortion. This indicates that there may be scope to increase access to contraception. There has also been a shift toward accessing contraception from community and online pharmacies, rather than GPs.
In response to these findings, local partners have worked together to ensure intervention earlier in the pathway. This includes a Sussex-wide communication and engagement plan to promote the availability and benefits of contraception (including the availability of emergency contraception) and clarify routes of access. Leads in Sussex have also been considering how the age of service users may impact how they seek information about sexual health services and abortion services, and whether they are at risk of reading misinformation on contraception online. Work is underway to explore how to improve online access to education tools and create more online access to contraception. This could include, for example, online communications that target populations with higher rates of use of sexual health and abortion services. The aim is to ensure that the population of Sussex is not only informed about services but are also aware of the range of contraceptive options available and their benefits.
Commissioners are also responding to greater need in areas of higher deprivation by working with the Women’s Health Hub to support access to contraception in these locations. The ICB will also conduct a locally developed women’s health survey to understand patients’ views on and use of contraception. Additionally, NHS and local authority commissioners are working together to make changes in local pathways to improve patients’ experiences and access to care.
Taking a whole-system, whole-pathway approach to assessing population needs and behaviours helps commissioners to understand drivers for increasing demand and trends in access in their local area. This, in turn, supports the development of targeted interventions. Access to, and choice of, all forms of contraception are important aspects of reproductive health and a key component of the abortion pathway.
Abortion services model
This model is intended to support collaboration between abortion providers and system partners arranging and delivering sexual and reproductive health services.
The sections of the pyramid (see image and description below) represent the volumes of patients that access each category of services. There is also a correlation between volumes of activity and clinical complexity.
Services can be split into 4 categories:
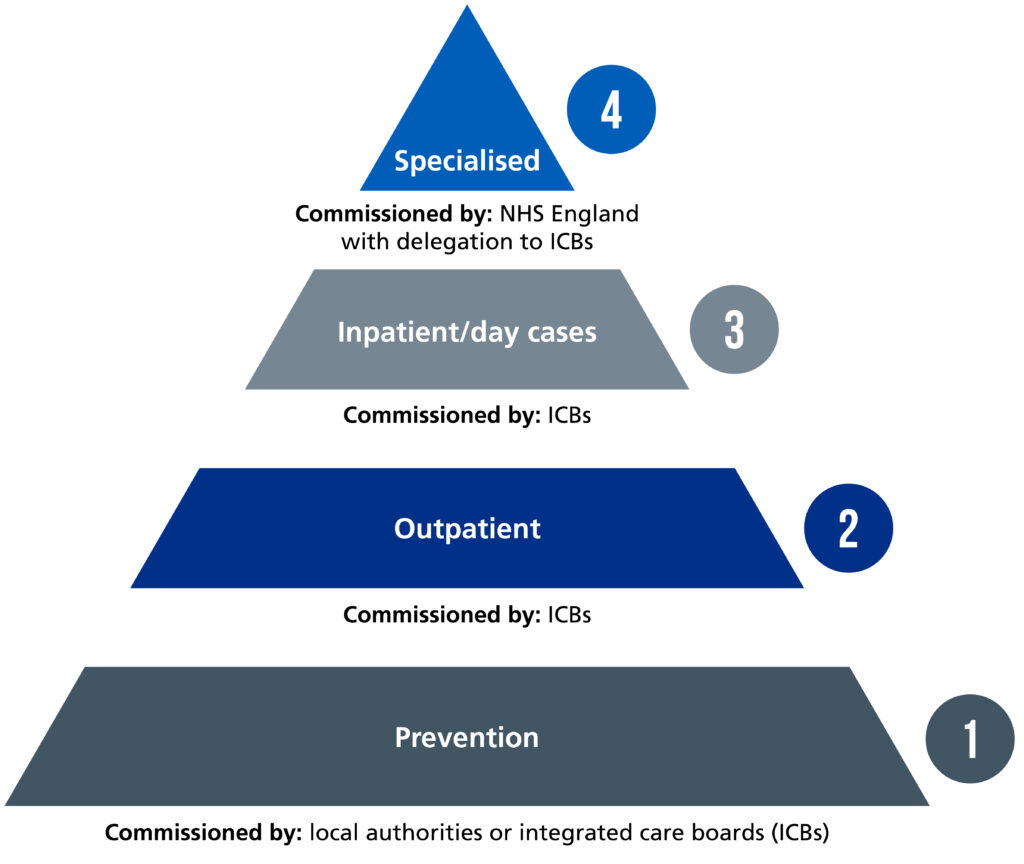
1. Prevention
Provision that prevents unplanned pregnancies by providing access to a choice of contraception (including long-acting, reversible contraception).
Commissioned by: local authorities or integrated care boards (ICBs).
Accessed through: sexual health services, primary care (including pharmacies), women’s health hubs, NHS and independent abortion providers.
2. Outpatient services
This includes procedures in a community or clinic setting, as well as home management. Services include one-stop appointments in clinics, a combination of in-clinic consultations (and scans) and remote interventions, and fully remote interventions. Early medical or telemedical interventions under 10 weeks and some early surgical interventions are also in this category.
Commissioned by: ICBs
Accessed through: NHS and independent providers
3. Inpatient or day cases
This includes surgical interventions up to the legal limit of 24 weeks and, in very limited cases, beyond that limit. It also includes some later gestation medical interventions.
Commissioned by: ICBs
Accessed through: NHS and independent providers
4. Specialised services
Specialist cases accessed through NHS providers.
Commissioned by: NHS England with onward delegation to ICBs
Accessed through: NHS providers
Publication reference: PRN00896

