Accessible image text
Improving lipid management by pro-actively identifying people at-risk and optimising their management is one of the principal ways the NHS can contribute to improved population health by preventing death and disability from cardiovascular events.
What’s the opportunity?
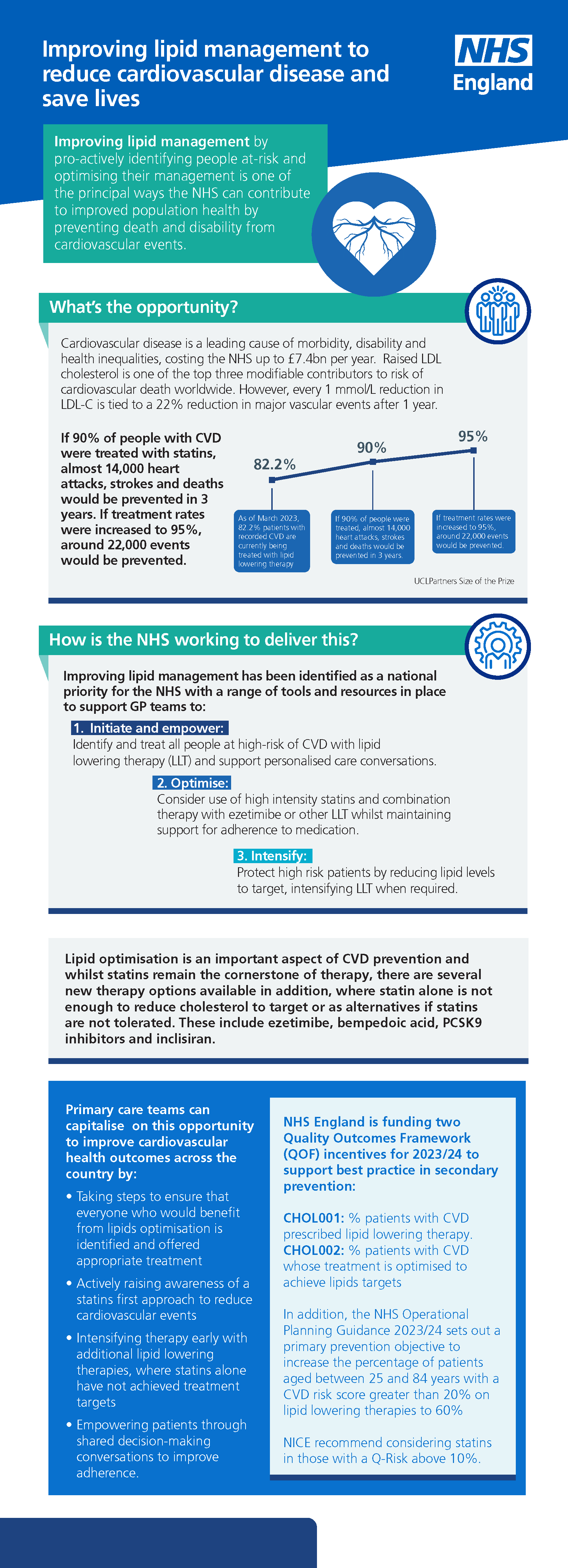
Cardiovascular disease is a leading cause of morbidity, disability and health inequalities, costing the NHS up to £7.4bn per year. Raised LDL cholesterol is one of the top three modifiable contributors to risk of cardiovascular death worldwide. However, every 1 mmol/L reduction in LDL-C is tied to a 22% reduction in major vascular events after 1 year.
As of March 2023, 82.2% patients with recorded CVD are currently being treated with lipid lowering therapy. If 90% of people with CVD were treated with statins, almost 14,000 heart attacks, strokes and deaths would be prevented in 3 years. If treatment rates were increased to 95%, around 22,000 events would be prevented.
Source: UCLPartners Size of the Prize
How is the NHS working to deliver this?
Improving lipid management has been identified as a national priority for the NHS with a range of tools and resources in place to support GP teams to:
1. Initiate and empower: Identify and treat all people at high-risk of CVD with lipid lowering therapy (LLT) and support personalised care conversations.
2. Optimise: Consider use of high intensity statins and combination therapy with ezetimibe or other LLT whilst maintaining support for adherence to medication.
3. Intensify: Protect high risk patients by reducing lipid levels to target, intensifying LLT when required.
Lipid optimisation is an important aspect of CVD prevention and whilst statins remain the cornerstone of therapy, there are several new therapy options available in addition, where statin alone is not enough to reduce cholesterol to target or as alternatives if statins are not tolerated. These include ezetimibe, bempedoic acid, PCSK9 inhibitors and inclisiran.
Primary care teams can capitalise on this opportunity to improve cardiovascular health outcomes across the country by:
- Taking steps to ensure that everyone who would benefit from lipids optimisation is identified and offered appropriate treatment
- Actively raising awareness of a statins first approach to reduce cardiovascular events
- Intensifying therapy early with additional lipid lowering therapies, where statins alone have not achieved treatment targets
- Empowering patients through shared decision-making conversations to improve adherence.
NHS England is funding two Quality Outcomes Framework (QOF) incentives for 2023/24 to support best practice in secondary prevention:
- CHOL001: % patients with CVD prescribed lipid lowering therapy.
- CHOL002: % patients with CVD whose treatment is optimised to achieve lipids targets.
In addition, the NHS Operational Planning Guidance 2023/24 sets out a primary prevention objective to increase the percentage of patients aged between 25 and 84 years with a CVD risk score greater than 20% on lipid lowering therapies to 60% NICE recommend considering statins in those with a Q-Risk above 10%.