Guidance for integrated care systems
Introduction
Individual placement and support (IPS) is an evidence-based model of supported employment. It has been rigorously trialled and has consistently outperformed all other tested forms of support for job seekers with severe and enduring mental health problems.[1] The implementation of IPS has been part of the NHS Long Term Plan and preceding strategies for national mental health improvement for over 8 years and is a fundamental part of the ongoing transformation of community mental health (CMH) services. IPS should be embedded within integrated models of primary and CMH services for patients with severe mental illness (SMI).[2]
Integrated care systems (ICSs) can have a positive impact on the mental health of their populations and reduce health inequalities by ensuring that investment into IPS services is sufficient to meet the ambitions of the NHS Long Term Plan, that services are integrated within transformed CMH models, and that they will continue to be available for anyone who can benefit from this unique and highly effective intervention.[3]
“I feel so happy to be working after so many years of not being well. I see myself in this job for a long time. Being in work means so much to me.”
Debrah, IPS for SMI
“With the employment specialist’s support, in less than a year my client has transformed. Since starting her job, I have seen her blossom.”
Debrah’s clinician
IPS services have a core role in supporting ICSs to achieve each of their four fundamental purposes:
1. Improving population health and healthcare
- Supported employment programmes are recognised by the National Institute for Health and Care Excellence (NICE) as an essential aspect of mental health care (NICE: QS80; QS95; CG178 & CG185).
- For those who want it, paid employment in “good work” positively contributes to mental health outcomes, with the Royal College of Psychiatrists confirming that “supporting individuals to work, wherever possible, can positively contribute to the recovery of individuals who have mental health conditions. Therefore, all mental health professionals should… view being in appropriate work as a key treatment outcome.”[4]
- In part through increasing access to social networks and improving social inclusion, suitable paid employment has been shown to lower an individual’s risk of suicide[5] and risk of relapse.[6]
- Moreover, better mental health lowers the likelihood of poor physical health. People living with SMI die 15 – 20 years earlier than the general population.[7]
2. Tackling unequal outcomes and access
- People with mental health problems (mild or severe) have employment rates between 25 and 40 percentage points lower than for people without such conditions, depending on where they live (Money and Mental Health Policy Institute (2022) No one left behind: Making levelling up deliver for people with mental health problems).
- Only 6% – 8% of people with SMI are in paid employment,[8] compared to 75% of the general population;[9] however, approximately 80% of people with SMI want to work.[10]
- The Care Quality Commission (CQC) CMH survey 2022 found that 50% of respondents would have liked support to find or keep work but were not offered it.
- The Royal College of Psychiatrists (2021/22) National report for England EIP audit Clinical Audit of Psychosis (NCAP) 21/22 report found that 26% of patients are not being offered supported employment and education, in spite of NICE guidance affirming that they should (NICE QS80 & QS102).
- IPS can play a vital role in tackling health inequalities and delivering on the Core20PLUS5 For example, 27% of patients accessing IPS services between April 2021 to October 2022 are from the most deprived 20% of communities (MHSDS).
- Research has also shown that IPS is effective for people from different ethnic groups, with people from Black, Asian and minority ethnic communities “not differentially disadvantaged in relation to either access to or outcomes of IPS employment services.”
3. Enhancing productivity and value for money
- A recent systematic review, based on 28 studies, found that “there is a strong economic case” for the implementation of IPS programmes, indicating that the true value is likely even higher owing to only limited evidence on the long-term impacts at present.
- Research has found that people helped into employment are likely to need less support from CMH services in the future and are less likely to have further inpatient admissions.
- A five-year study of IPS from Switzerland reported that 44% of those receiving IPS were employed for at least 50% of the time over five years, compared with just 11% in a control group who received traditional vocational rehabilitation. Those in the IPS group also had over 50% fewer days in hospital which equates to a saving of at least £20,000 per person over five years.[11]
- Research comparing IPS with other vocational services in six European countries concluded that IPS achieves twice the rate of job outcomes for people with SMI versus traditional employment support and that IPS clients have reduced relapse and spend fewer days in the hospital.
4. Helping the NHS to support broader social and economic development
- As the largest employer, and key anchor institution, in every part of the country, the NHS has a key role to play in creating an inclusive economy and tackling inequalities in access to good work. As the NHS Confederation has observed “an engaged ICS can not only broaden its own traditional prevention and population health planning to include new partners, such as the private sector…they can themselves… influence the future direction of local social and economic development – moulding an economy and place that supports health in everything it does” (Unlocking the NHS’s social and economic potential (2022)).
- Investment and support for IPS services is one of the key ways that an ICS can support broader economic and social development. Through the provision of intensive support to both clients and employers, IPS employment specialists (ESs) support those with SMI to gain or retain sustained employment.
The expansion of IPS in England is world-leading, with ambitions for access growing from 10k per year in 2017 to a target of 55k per year by the end of 2023/24. However, the expansion of IPS has been slower than anticipated in some parts of the country as there are system challenges impacting on the delivery of supported employment for people with SMI. These challenges vary from system to system but include:
- Limited investment in IPS services impacting services’ ability to recruit more staff and see more clients to achieve Long Term Plan ambitions.
- Contracting arrangements that limit the ability of services to expand, attract staff, access clinical systems and integrate with clinical teams.
- Insufficient referrals from clinical teams to meet local need and fill capacity.
- Workforce recruitment and / or retention to deliver IPS expansion, with lots of competition for staff and paucity of well-developed IPS role profiles.
- Poor data quality and flows resulting in under-reporting of access and an inability to reconcile local systems’ data with nationally recorded data in the Mental Health Services Data Set (MHSDS).
- Confusion linked to the presence of different employment support programmes including IPS for SMI, primary care and drugs and alcohol (D&A), and the roll-out of employment advisors (EA) in NHS Talking Therapies (formerly IAPT).
This guidance has been developed based on the feedback from commissioners and services on the information they require to inform their commissioning of IPS services. It has been developed in partnership with commissioners, systems, providers, researchers and experts of the IPS model, and service users. It is intended to be a useful resource to support local areas to effectively commission IPS services in line with the NHS Long Term Plan ambition. It includes:
- Information to support development of local service specifications to enable commissioners to ensure that services are fit for purpose and offer value for money.
- Guidance on contracting with trusts and voluntary organisations, charities and social enterprises (VCSEs).
- An overview of different national employment support initiatives including IPS.
- Practical solutions for systems to support workforce recruitment for IPS.
- Guidance for embedding IPS into transformed CMH models, supporting integration within clinical teams and increasing IPS referrals from outside of secondary mental health teams (eg from primary care, voluntary sector and self-referral).
- Improving data quality and ensuring that data flows accurately to the MHSDS.
In addition to this guidance, during 2022 members of an NHS England advisory group took evidence on how best to improve access to supported employment for people with mental health conditions. From a population health management perspective, the advisory group concluded that the ratio of ES to general population needed to address access numbers and have an impact on employment rates within mental health services for people with SMI was approximately 1 ES per 42,000 general population. The recommendations resulting from their work, and the list of members of the advisory group, can be accessed on FutureNHS (log in required).
Developing local service specifications
Cohort
People with SMI or complex mental health who want to gain or retain employment. SMI covers a range of needs and diagnoses, including but not limited to: psychosis, bipolar disorder, ‘personality disorder’ diagnosis, eating disorders, severe depression and mental health rehabilitation needs –some of which may be co-existing with other conditions such as frailty, cognitive impairment, neurodevelopmental conditions or substance use.[12]
Access
Integrated care boards’ (ICBs’) access targets are available on FutureNHS (log in required). In MHSDS access is calculated based on the first appointment[13] the client attends once they have agreed to partake in an IPS service (this may occur during the initial session, in which case it should be counted as the first appointment).[14] IPS is open to all those who want to work and should operate a zero exclusion policy (ie include those with co-occurring conditions such as SMI and drug and alcohol dependency), not refusing access (in favour of the patient accessing IPS via D&A services) unless they themselves choose this option. Mental health professionals play a key role in routinely discussing employment with service users and their attitudes on the employability of people with mental illness are repeatedly identified as a common implementation barrier that needs to be addressed to improve access to IPS for all that wish to return to, or retain, competitive paid employment (Lettieri A et al 2022; Craig T et al 2014).
Workforce
All IPS teams should comprise of team leaders (Agenda for Change (AfC) Band 6) and ESs (AfC Band 5). Some services have introduced senior ESs (AfC Band 6) and service managers (AfC Band 7/8a). Where services pay less than the recommended salaries for these posts, they are unlikely to be able to retain staff and the outcomes delivered are inferior to those of services that pay staff at the appropriate salary levels. A mature service operating to high fidelity would be expected to employ a team leader for every 6 ESs, and a service manager for every 5 team leaders. Peer support workers can also play a critical role in extending the delivery of IPS. Peer support workers can offer service users access to people with lived experience, empathy and encouragement and the chance to sense-check fears or concerns. However, in an IPS service, the peer support worker role must remain separate from the role of the ES, and IPS fidelity requires that each ES carries out all phases of the employment service.
Caseload
ESs are recommended to carry an active caseload of 20 to 25 clients at any one time. A caseload of 20 or below is required for the maximum score of 5 on IPS fidelity item 1 – caseload size. Caseloads of 21 – 25 would score 4 out of 5 for this fidelity item. Team leaders will carry a caseload of up to 10 clients at any one time and will manage the team and assign work to the ESs. Caseloads consist of both new employment and job retention cases. Where resourcing allows, services may wish to consider having job retention specialists within their team of ESs to ensure a greater emphasis is placed upon early intervention and prevention of job loss as well as supporting transition periods. Over the course of a year, an ES will work with up to 50 clients. There are no fixed time-limits to the duration of IPS support. However, services may choose to review with unemployed clients after 9 months of support and with in-work (retention) clients after 4 months of support. This should be done on a case-by-case basis.
Fidelity
IPS is an evidence-based model. Services need to be assessed against the IPS fidelity model regularly – currently every 2 years – with guided self-assessments produced in interim years. The fidelity scale comprises 25 items and a maximum score of 125. To be recognised as an IPS service, a score of 74 or more is required. IPS Grow (the implementation support package for IPS provided by the VCSE social finance) deliver all fidelity reviews. High-fidelity services can achieve the IPS Grow quality mark (good or exemplary). Due to previous misconceptions around the scoring system, it is important to emphasise that fidelity scores are not detrimentally impacted if the service accepts GP, primary care or self-referral.[15]
Outcomes
The purpose of IPS is to support clients into competitive paid employment (not volunteering or an education offer) along with job retention support. Benchmarking suggests that a new IPS service should be achieving a minimum of 30% – 40% of clients into employment or helping them to retain their existing employment. Mature, high-performing services (higher fidelity scoring services) would be expected to achieve job outcome rates of between 40% and 55%. Employer engagement is particularly important and services score poorly in their fidelity reviews if they do not do this effectively. Commissioners should promote employer engagement and monitor job outcomes as part of their contract with the IPS service.
Integration
IPS services need to be integrated with clinical teams and multi-disciplinary teams (MDTs) to promote referrals and ensure clinical involvement and oversight of their clients’ mental health needs whilst seeking and retaining employment. IPS teams can be co-located with EIP teams, CMH teams, primary care networks (PCNs) or standalone. If standalone, IPS team members will need to integrate in other ways with EIP and CMH teams to ensure MDT working takes place. The level of integration will impact on the volume of referrals received and overall system support for IPS and employment support. IPS should be prioritised for integration within transformed CMH models and enabled to receive referrals from GPs, primary care and self-referral.
Data
All IPS services should flow data to the MHSDS.[16] They can do this independently or via a contracting trust. Support to flow data is available from NHS Digital and IPS data is reported in a dashboard on FutureNHS (log in required). Commissioners should ensure that the IPS services they commission have the capability to flow data into MHSDS and embed this as a criteria when selecting a service provider. There are a set of standard metrics that all IPS services should be using to track performance and the delivery of outcomes.
Co-production can build the capabilities and improve the impact of IPS services. Co-production refers to working collaboratively with clients to give them a voice, listen and involve them in making decisions that shape future services. Some services also refer to the additional work they do with other stakeholders as co-production. While maintaining fidelity to the IPS model, commissioners may wish to consider involving clients in the co-design of service specifications and evaluating tendering exercises.
People with lived experience can play a key role in co-delivery, including involvement in the recruitment of ESs and team leaders. Co-evaluation of services to understand client experiences and identify areas of good practice and improvement is also beneficial. IPS Grow have shared good practice examples of co-production in IPS services and are as part of a consortium, including the Centre for Mental Health, developing a half day learning module, funded by Health Education England, on how services could better develop and integrate the principles of co-production within their planning and operations.
Contracting for IPS services
Resources:
Our survey of ICB contract arrangements in place with IPS providers show that there are two main varieties of contracting arrangements:
- ICB contracts with trusts payable through either a block contract or separate commission. Trusts will either provide the service in-house or will sub-contract the IPS service to an independent provider. Typically, these are VCSE but there are some local authority, housing association and private sector providers.
- ICB contracts directly with providers, the majority of these are VCSE providers.
Detail required in contracts
The NHS Long Term Plan targets for local IPS services should be clearly identified in contracts in order to improve awareness amongst commissioners, providers and other stakeholders. IPS contracts should specify the number of clients that should access the service within a given financial year. This number should be the Long Term Plan access target, wherever possible. In the case of block contracts, service specifications should outline who the service is for, the parameters of the service, expected referrals, access levels and outcomes.
Short term contracts (less than 3 years) with IPS providers should be avoided as these undermine the ability of the service to plan ahead and can impact negatively on the ability to recruit and retain staff. Providers on short term contracts report an inability to advertise for permanent positions due to uncertainty of funding and these short-term contracts are less appealing to prospective employees.
The value of contracts should be calculated based on the local Long Term Plan target for IPS access, the cost of staff and the caseload that they can support over the lifetime of the contract. Baseline CMH funding has been calculated to ensure there are sufficient funds to invest in IPS to achieve year-on-year increases in access.
Whichever approach is taken to contract with an IPS provider, the commissioner should ensure that there are adequate arrangements in place for the IPS team to be integrated within the clinical teams as outlined above and that the service has the infrastructure required to support effective delivery, including access to clinical systems and appropriate referral pathways.
Commissioning a VCSE provider
Contracting a VCSE provider to deliver IPS can enable the service to utilise existing relationships with employers and models of engagement with people with SMI, and can offer a very person-centred, non-clinical service which is highly valued by patients. The services are often agile and can operate between organisational boundaries to extend services to clients with SMI that they would not normally be able to access through secondary mental health pathways.
IPS contracts with VCSE organisations should be funded to the same rate as NHS services. VCSE services can deliver cheaper IPS services than an NHS equivalent service, but staff should still be paid at the same recommended rates (information on recommended NHS bandings are provided in the workforce section above). Where VCSE services currently employ ESs and team leaders on a lower salary than NHS services, they should look to create parity of pay with NHS services. Underpaying staff has been shown to result in staff migration to better paying roles, which undermines the sustainability of IPS providers and can have a detrimental impact on the clients they serve.
Short term contracts with VCSE organisations can also lead to financial instability and result in inability to recruit and retain staff. It is essential that these organisations are supported by contracts that enable parity with trust providers.
Performance management of both VCSE and trust providers is vital to achieve maximum return on the investment in IPS services. Where trusts are not the IPS service provider, commissioners should consider how they can build referrals and IPS access targets into existing performance management arrangements with trusts.
Employment support landscape
Thanks to the robust evidence base, Department for Work and Pensions (DWP) investment in IPS has increased significantly since 2021. The model is now also used as a solution to address unemployment for people with D&A dependency and moderate physical and mental health concerns in primary care (the latter is only currently present in two sites in England – South Yorkshire Mayoral Combined Authority and West Midlands Combined Authority – but is due to expand during 2023/24). DWP have also increased the number of EA in NHS Talking Therapies.
The cohorts and intensity of support provided in each of these services are different (see Appendices 1, 2 and 3), however there is some crossover between cohorts seen in NHS Talking Therapies, IPS in Primary Care and IPS in D&A as well as between cohorts for IPS for SMI and D&A. 60% of the clients accessing IPS in D&A have a diagnosed mental health illness and feedback from these services suggests that clients accessing IPS SMI with a D&A dependency are often refused access until their substance dependency has been resolved. IPS for SMI should not refuse clients due to substance dependency, however clients should be able to choose which service best meets their needs. Zero exclusion is an important principle of IPS delivery in all settings. SMI services should not screen patients for any other factors, such as perceived job readiness, symptoms, presentation or reasons for / frequency of previous job loss. SMI services should promote the option to self-refer for IPS support to all patients.
There is a need to establish a mechanism to count access of clients in IPS D&A that have a SMI for the purposes of measuring delivery against the NHS Long Term Plan targets. All D&A services will be reporting access through a new data reporting tool (being developed by IPS Grow). Over time, it is hoped that this tool can capture the number of clients with a co-occurring condition of SMI.
Given the range of IPS and alternative employment support services that are increasingly on offer at a local level, commissioners are encouraged to deliver an integrated, network-wide approach so that there is a “graded offer”[17] available according to need, with clear referral pathways and distinctions made between the needs and services provided for different cohorts (those with mild to moderate, complex and severe mental health needs).
IPS workforce expansion
The existing IPS workforce is estimated to be approximately 650 in 2022/23 and needs to expand to approximately 1,650 to deliver access of 55K in 2023/24. IPS providers across the country report that recruitment is difficult, and they are not getting the number or quality of applicants to fulfil their recruitment initiatives.
IPS staff are recruited for their attitude, values and ability to connect with people with SMI for the purposes of understanding their needs and supporting them to gain or retain employment, rather than formal qualifications. Suitable candidates can come from many occupational groups and do not have to have any recruitment experience or experience of working in mental health. IPS Grow has published an overview of a typical IPS ES and IPS team leader role, responsibilities and person specification.
The profile of IPS career paths is low and more needs to be done to market these roles and create a future recruitment pipeline in order to increase access to IPS. Particularly in light of the expected expansion of EA in NHS Talking Therapies and ES in IPS D&A services, the various employment services mentioned in the previous section need to work together for the recruitment and retention of workforce.
Resources will be added to the IPS workspace on the FutureNHS platform (log in required) in due course to provide additional clarity around the differing role profiles, responsibilities and person specifications for each programme, including potential career paths within and across different services.
NHS England are commissioning a recruitment partner to support the development of resources to improve recruitment to IPS vacancies. These resources will include a candidate database, standardised job descriptions, advertisements and the organisation of recruitment centres to improve the quality of recruitment practices in IPS. This support will be made available in 2023/24. In the meantime, where providers are struggling to recruit permanent staff through their normal processes, they may choose to make use of recruitment agencies and other local recruitment support. However, providers should avoid temping agencies/recruiting staff on a temporary basis, given that a higher turnover of ES is known to increase client drop-out rates and lower service outcomes. It typically takes up to 3 months for a newly recruited ES to learn the role, and up to a further 3 months to perform well against targets.
In addition to this recruitment initiative, a 3-year programme of training has been agreed, to work with the existing and new IPS workforce to increase their skills and deliver improved outcomes for clients. This will include a training programme to improve the quality and effectiveness of employer engagement and leadership training targeted for team and service leads. Details of the 6 courses to be developed and run over the next 3 years are provided below:
- Training for team leaders (4-day course)
- 8 cohorts, available from June 2023
- Training in employer engagement (applying train-the-trainer methodology)
- 8 cohorts, available from October 2023
- Job retention e-learning
- Available from January 2024
- Case management e-learning
- Available from November 2023
- Co-production training
- 2 cohorts initially, available from November 2024
- Advanced team leader training
- 2 cohorts initially, available from June 2025
Between May 2021 and January 2023, the Centre for Mental Health and IPS Grow have delivered team leader training to 9 cohorts, reaching over 135 team leaders. Feedback on the training has been consistently high, with the latest cohort rating the course as 10/10 overall and managers of team leaders overwhelmingly recommending the course to others (rating it 9.2/10).
All booking for upcoming training will go through the Centre for Mental Health and carry no cost.
Peer support workers can also play a critical role in extending the delivery of IPS. Peer support workers can offer service users access to people with lived experience, empathy and encouragement and the chance to sense-check fears or concerns.
In an IPS service, the peer support worker role must remain separate from the role of the ES. As such, peer support workers are not expected to carry a caseload or undertake core functions of the ES. IPS fidelity requires that each ES carries out all phases of the employment service, including intake, engagement, assessment, job placement, job coaching, and follow-along support. However, peer support workers can play an important role in helping people with SMI to consider employment prior to joining an IPS service (step up), providing additional support during an IPS service, and extending follow-along support after the end of the IPS service (step down). IPS services may also consider how career pathways can be created between peer support worker roles and ES roles, including the package of training and support they provide.
Integrating IPS and maximising referrals
Resources:
The NHS Long Term Plan requires the transformation of CMH to develop new models of care to provide better access and improved outcomes for people with SMI. IPS should be embedded within these transformed models and systems should extend access within these models to a wider range of local health partners (including PCNs to enable GP / mental health practitioner / social prescriber referrals) to enable access for people with SMI that are being treated in primary care. A patient with complex mental health needs or SMI should be able to access IPS services without needing to be registered with or in receipt of secondary care CMH services. This is particularly important in the case of transformed models, where more CMH services are delivered via primary care.
Where systems are extending referrals from primary care into IPS, they must ensure that services are resourced sufficiently to achieve their Long Term Plan targets. Additional workforce and investment are likely to be required, and resources may need to be moved around to ensure an entire PCN has access to IPS. Investment will also need to be supported by the development of appropriate IPS pathways within primary care, alongside appropriate clinical oversight, risk management and governance mechanisms.
IPS is an evidence-based model which identifies key organisational and operational components required to deliver the best outcomes for people with SMI, including integration with clinical teams. Service quality is measured using the IPS fidelity scale. IPS Grow undertakes fidelity reviews and award high-fidelity services with the IPS Grow quality mark.
The fidelity model does not restrict systems from enabling referrals from GPs or primary care into IPS for SMI. Commissioners should consider the following actions to enable the integration of IPS in new models of CMH and PCNs:
- Using flexibilities of existing contracts to encourage providers to take referrals from primary care to IPS. If contracts explicitly prohibit this, commissioners should consider contract variations and planned re-commissioning rounds as opportunities to expand access for people with SMI via primary care.
- Simplifying the number of pathways and relationships with clinical teams required to support clients referred from primary care.
- Developing organisational arrangements with PCNs for the purposes of providing clinical oversight and managing clinical risk of primary care clients in IPS.
- Establishing formalised collaboration between the IPS workers and primary care and / or colocation of teams.
- Supporting the sharing of data and reporting of IPS access through the MHSDS.
Black Country Healthcare NHS Foundation Trust, Oxford Health NHS Foundation Trust and Norfolk and Waveney IPS services all accept referrals from primary care into their IPS for SMI service and have contributed to case studies (on NHSFuture – log in required) that highlight the key tenants of their approach (in line with the above fidelity principles) and how they overcame challenges to implement successful services. It is important to emphasise that these are IPS for SMI services, and are distinct from DWP-commissioned IPS in primary care, a service currently available in only two sites in England, which provides IPS to people with moderate physical and mental health concerns in primary care (see appendices 1, 2 and 3).
Pathways should be developed to allow people with SMI to access IPS in a manner and setting that meets their needs. It is expected that people with SMI will access IPS alongside other CMH services in parallel, if appropriate for their needs; accessing one CMH service should not affect one’s ability to access other CMH services. The case studies (on NHSFuture – log in required) from the Kent and Medway and Cornwall IPS services are examples of providers that are well integrated within CMH teams and enjoy strong links with EIP.
Similarly, as part of the zero-exclusion IPS principle and fidelity item, services should actively promote self-referral to people with SMI. Services can promote self-referral through the trust/treatment team, including by displaying posters in host sites, attending client/service user meetings and distributing promotional material (eg leaflets, emails, SMS). Once a person with SMI has self-referred themselves for IPS support, ESs should seek that person’s consent to contact their treatment team and share information, so that care is integrated.
SMS text messaging has shown promise as a way of promoting IPS employment support to people with SMI. Clients can be signposted to IPS service websites and telephone numbers, or to have a discussion with their treatment team. Services may wish to consider text messaging as a promotional tool within secondary and primary care settings. Information Governance should be fully considered; for example, patients must have given consent to be contacted via text in this way. Services should work with their trust/treatment team information governance lead to ensure that text messaging processes are in line with relevant policies and legislation, eg General Data Protection Regulation (GDPR).
Moreover, the voluntary sector has a vital role to play in CMH transformation. IPS services should work closely with social prescribing link workers, community connectors and other third sector staff to ensure that people with SMI can access employment support alongside secondary or primary care. As with self-referral, ESs should seek consent to contact their client’s treatment team and share information, so that care is integrated.
The diagram below shows how transformed models and IPS pathways might work.
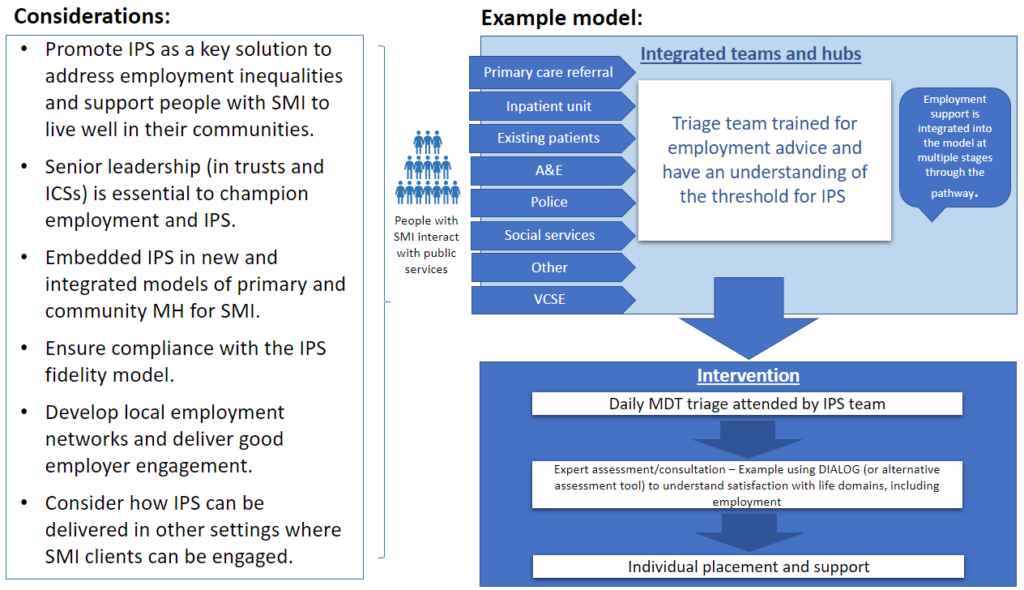
The example model image shows the following:
Considerations
- Promote IPS as a key solution to address employment inequalities and support people with SMI to live well in their communities.
- Senior leadership (in trusts and ICSs) is essential to champion employment and IPS.
- Embedded IPS in new and integrated models of primary and community mental health for SMI.
- Ensure compliance with the IPS fidelity model.
- Develop local employment networks and deliver good employer engagement.
- Consider how IPS can be delivered in other settings where SMI clients can be engaged.
Example model for integrated teams and hubs
Starting point
People with SMI interact with public services.
Example services
- Primary care referral
- In-patient unit
- Existing patients
- A&E
- Police
- Social services
- Other
- VCSE
Support
Triage team trained for employment advice and have an understanding of the threshold for IPS. Employment support is integrated into the model at multiple stages throughout the pathway.
Intervention
- Daily MDT triage attended by IPS team.
- Expert assessment/consultation – example using DIALOG (or alternative assessment tool) to understand satisfaction with life domains, including employment.
- Individual placement and support.
Improving data quality
Since April 2021 all IPS services have been required to flow data to the MHSDS. Almost all providers are now flowing at least some data, however the quality is variable due to missing / invalid entries and ongoing challenges with capturing activity from non-NHS services where data sharing agreements are not yet in place to enable direct data entry on MHSDS. The common issues that have been reported to the national team include:
- MHSDS does not record data in the same way that IPS teams do; for example, MHSDS records “access” as first contact after referral whereas teams go further, recording “access” only after completion of a vocational profile.
- Commissioners are unable to reconcile the data that providers are reporting locally with that on the MHSDS.
- A number of non-NHS services report that they do not have adequate access to the hardware and clinical systems that they need for the purposes of recording client details and there is a lot of manual data handling.
There are a range of resources that can be used to improve the quality of IPS data, which include:
- FutureNHS IPS Hub. Includes MHSDS dashboard, data quality workshops and data resources (log in required).
- NHS Digital (2021) Step-by-step guide: from registration to successful submission of the
- NHS Digital. MDSDS data quality submission summary tool.
- Direct support from NHS Digital MHSDS team: mhsdsdq@nhsdigital.nhs.uk
- Direct support from NHS Data Liaison team: dataliaison@nhs.net
- NHS Digital. Mental health services dataset – data quality dashboard.
- NHS Digital. Improving the quality of EIP and IPS data in MHSDS webinar.
- Devon’s guide to governance and information sharing between NHS and VCSE (log in required).
- Future NHS. IPS Grow support includes:
- advice and guidance for IPS commissioners and providers
- development of tools and templates
- sharing best practice and communities of practice
- delivery of fidelity reviews
- support for recruitment and
Commissioners should also continue to ensure that adequate scrutiny is placed on IPS services’ data and performance at a local level, to drive data quality improvements.
Given the complexity of the challenge, systems may wish to consider funding a specific data role within IPS services, so that adequate time can be ring-fenced to improve data accuracy as well as provide evidence for fidelity reviews.
Appendix 1. Characteristics of IPS services and wider employment support
|
|
Employment Advisors (EAs) in NHS Talking Therapies (formerly Improving Access to Psychological Therapies (IAPT)) |
Individual placement and support (IPS) | ||
|
IPS for severe mental illness (SMI) |
IPS in drug and alcohol treatment |
IPS in Primary Care | ||
|
Who is the intervention intended for? |
People with depression and anxiety receiving NHS Talking Therapies treatment, who are in work and out of work. |
People with SMI or complex mental health. ‘SMI’ covers a range of needs and diagnoses, including but not limited to: psychosis, bipolar disorder, ‘personality disorder’ diagnosis, eating disorders, severe depression and mental health rehabilitation needs –some of which may be co-existing with other conditions. |
People in structured community treatment for drug and/or alcohol misuse. Other eligibility criteria are (i) working age, (ii) able to work legally in the UK, (iii) wants and is in need of support to find or to retain employment. |
People with common mental health or physical health disabilities. Other eligibility criteria are (i) working age, (ii) able to work legally in the UK, (iii) wants and is in need of support to find or to retain employment, (iv) not taking part in any other DWP funded employment programme. |
|
Outputs |
In 2021/22, the number of people starting employment support in EA in NHS Talking Therapies sites was 35,000. This is expected to increase to 100,000 per year from 2024/25. |
In 21/22, the number of people accessing IPS for SMI was 20,850. The NHS Long Term Plan target is for 55,000 people to access IPS for SMI during 2023/24. |
Once full roll-out has been achieved in 2024-25, we expect the IPS teams to work with approximately 13,000 people per year. |
The outcomes will be confirmed once the commercial exercise has been completed.
|
|
Caseload |
Mixed caseload including people who are in work and out of work. Support 100 – 120 NHS Talking Therapies clients per year. |
Each IPS ES should carry 20 – 25 active cases at any one time and between 40 – 50 cases over the course of a year. |
Expectation that IPS specialists will work with 40-50 people per year, with reduced caseload sizes for team leaders. |
Expectation that IPS specialists will have a caseload of 25 with reduced caseload sizes for team leaders. |
|
Proportion of clients supported |
The number of people receiving employment support is on average 15% of those who complete NHS Talking Therapies treatment. Proportion varies from site to site from 5% to 30% across current sites. EAs in NHS Talking Therapies currently has 40% coverage across England, with expansion plans to provide 100% coverage and support 100K people by 24/25). |
The number of people with SMI totals 530K, the target of 44K seen in IPS in 22/23 equates to 8% of this total population. |
This will vary somewhat from area to area, but overall, we would expect the IPS teams to work with around 5% of the treatment population per year once full roll-out has been achieved. |
Intention is to support up to 1,385 individuals from April 2023 to March 2025 across 6 upper tier authorities in England. |
|
Proportion in work / out of work |
67% in work including those off sick from work, 33% out of work. |
Recommendation that retention clients (in work) should be no more than 25%. However, please note that since April 2021 all job retention cases are counted as accessing IPS following removal of the job retention cap in MHSDS. |
Recommendation that retention clients (in work) should be no more than 15%. |
25% of caseload to be in work but struggling to remain in work. 75% out of work. |
|
Approach |
Client, EA and therapists work together to set employment goals and deliver bespoke action plan. |
ES works with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques and supporting employers to make reasonable adjustments. |
ES and treatment keyworker/clinician work with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques, and supporting employers to make reasonable adjustments/job carve. |
ES and healthcare professionals work with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques, and supporting employers to make reasonable adjustments/job carve. |
|
Intervention model |
Provision of information, advice and guidance to empower client to make better decisions. |
In depth support to meet the client’s needs to gain new or retain existing employment. |
In depth support to meet the client’s needs to gain new or retain existing employment. |
In depth support, focussing on personalised job matching and wrap around support to find and retain work. |
|
When support provided |
Before treatment starts, during treatment, between treatment and for a limited period post discharge from treatment. |
After self-referral or referral from a secondary care, primary care or voluntary sector team. Clients should be offered IPS on accessing the service and during any subsequent reviews. |
Clients are informed about IPS when first accessing the service. They can access IPS at any point in their structured treatment journey, and should be offered IPS upon accessing the service, through key working and at 6-month reviews. |
Individuals will be referred by their GP or can self-refer. Other organisations including Jobcentre Plus will sign-post individuals to the support. |
|
Number of sessions |
Between one to six sessions as standard, average of four sessions. More if required. |
As many sessions as required over the period the client is accessing IPS. |
Target is weekly meetings for first month and then fortnightly. |
Target is weekly meetings for first month and then fortnightly. |
|
Delivery models |
By phone, video conferences, face to face in person, in groups (virtual and in person). |
By phone, video conferences, face to face in person, in groups (virtual and in person). |
By phone, video conferences, face to face in person, in groups (virtual and in person). |
By phone, video conferences, face to face in person, in groups (virtual and in person). |
|
Length of intervention |
Typically, up to three to four months support, more if required, not unlimited. |
IPS is a time-unlimited service, meaning that there are no fixed limits to the duration of support. Clients may have multiple job starts and re-access the service after job loss. Services should monitor active caseload to ensure each ES can support 40 – 50 clients per year. |
Pre-employment support can be offered for up to 9 months, and in-work support for up to 4. These are soft limits and can be extended at the discretion of each team’s senior ES. |
Pre-employment support can be offered for up to 9 months, and in-work support for up to 4. |
|
Additional support |
Money guidance, access to food banks. |
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis. |
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis. |
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis. |
|
Linking with |
Jobcentre Plus, employers, training and education providers, social housing providers, debt counsellors, food banks, trade unions, employment lawyers, law centres. |
Jobcentre Plus, health partners, employers, training and education providers, social housing providers, debt counsellors, food banks, trade unions, employment lawyers, law centres. |
Jobcentre Plus, mental health services and primary care, employers, training and education providers, social housing / supported housing providers, debt counsellors, employment lawyers, law centres. |
Jobcentre Plus, mental health services and primary care, employers, training and education providers, social housing / supported housing providers, debt counsellors, employment lawyers, law centres. |
|
Refer onto |
Access to Work mental health support, Jobcentre Plus, other employment support providers including IPS and specialist providers, for example ES for people with Neurodiversity. |
Access to Work, IPS in D&A if co-occurring condition of SMI and drug/alcohol dependency if agreement reached that that would be a more appropriate setting. |
Other employment support providers, including IPS for SMI where the clients are also accessing secondary mental health services and if agreement reached that that would be a more appropriate setting. |
Access to Work, community support, specialist provision. |
Table description:
Who is the intervention intended for?
Employment Advisers (EAs) in NHS Talking Therapies (formerly Improving Access to Psychological Therapies (IAPT))
People with depression and anxiety receiving NHS Talking Therapies treatment, who are in work and out of work.
Individual placement and support for severe mental illness
For people with severe mental illness (SMI) or complex mental health. ‘SMI’ covers a range of needs and diagnoses, including but not limited to: psychosis, bipolar disorder, ‘personality disorder’ diagnosis, eating disorders, severe depression and mental health rehabilitation needs – some of which may be co-existing with other conditions.
Individual placement and support in drug and alcohol treatment
For people in structured community treatment for drug and/or alcohol misuse. Other eligibility criteria are (i) working age, (ii) able to work legally in the UK, (iii) wants and is in need of support to find or to retain employment.
Individual placement and support in primary care
For people with common mental health or physical health disabilities. Other eligibility criteria are (i) working age, (ii) able to work legally in the UK, (iii) wants and is in need of support to find or to retain employment, (iv) not taking part in any other DWP funded employment programme.
Outputs
Employment Advisers (EAs) in NHS Talking Therapies
In 2021/22, the number of people starting employment support in EA in NHS Talking Therapies sites was 35,000. This is expected to increase to 100,000 per year from 2024/25.
Individual placement and support for severe mental illness
In 21/22, the number of people accessing IPS for SMI was 20,850. The NHS Long Term Plan target is for 55,000 people to access IPS for SMI during 2023/24.
Individual placement and support in drug and alcohol treatment
Once full roll-out has been achieved in 2024-25, we expect the IPS teams to work with approximately 13,000 people per year.
Individual placement and support in primary care
The outcomes will be confirmed once the commercial exercise has been completed.
Caseload
Employment Advisers (EAs) in NHS Talking Therapies
Mixed caseload including people who are in work and out of work. Support 100 – 120 NHS Talking Therapies clients per year.
Individual placement and support for severe mental illness
Each IPS employment specialist should carry 20 – 25 active cases at any one time and between 40 – 50 cases over the course of a year.
Individual placement and support in drug and alcohol treatment
Expectation that IPS specialists will work with 40-50 people per year, with reduced caseload sizes for team leaders.
Individual placement and support in primary care
Expectation that IPS specialists will have a caseload of 25 with reduced caseload sizes for team leaders.
Proportion of clients supported
Employment Advisers (EAs) in NHS Talking Therapies
The number of people receiving employment support is on average 15% of those who complete NHS Talking Therapies treatment. Proportion varies from site to site from 5% to 30% across current sites. EAs in NHS Talking Therapies currently has 40% coverage across England, with expansion plans to provide 100% coverage and support 100K people by 24/25).
Individual placement and support for severe mental illness
The number of people with SMI totals 530K, the target of 44K seen in IPS in 22/23 equates to 8% of this total population.
Individual placement and support in drug and alcohol treatment
This will vary somewhat from area to area, but overall, we would expect the IPS teams to work with around 5% of the treatment population per year once full roll-out has been achieved.
Individual placement and support in primary care
Intention is to support up to 1,385 individuals from April 2023 to March 2025 across 6 upper tier authorities in England.
Proportion in work / out of work
Employment Advisers (EAs) in NHS Talking Therapies
67% in work including those off sick from work, 33% out of work.
Individual placement and support for severe mental illness
Recommendation that retention clients (in work) should be no more than 25%. However, please note that since April 2021 all job retention cases are counted as accessing IPS following removal of the job retention cap in MHSDS.
Individual placement and support in drug and alcohol treatment
Recommendation that retention clients (in work) should be no more than 15%.
Individual placement and support in primary care
25% of caseload to be in work but struggling to remain in work. 75% out of work.
Approach
Employment Advisers (EAs) in NHS Talking Therapies
Client, EA and therapists work together to set employment goals and deliver bespoke action plan.
Individual placement and support for severe mental illness
Employment specialist works with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques and supporting employers to make reasonable adjustments.
Individual placement and support in drug and alcohol treatment
Employment specialist and treatment keyworker/clinician work with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques, and supporting employers to make reasonable adjustments/job carve.
Individual placement and support in primary care
Employment specialist and healthcare professionals work with clients that are either out of work, or at risk of losing their job, to gain secure employment. IPS includes a rapid job search, confidence building, CV development, employer engagement and interview techniques, and supporting employers to make reasonable adjustments/job carve.
Intervention model
Employment Advisers (EAs) in NHS Talking Therapies
Provision of information, advice and guidance to empower client to make better decisions.
Individual placement and support for severe mental illness
In depth support to meet the client’s needs to gain new or retain existing employment.
Individual placement and support in drug and alcohol treatment
In depth support to meet the client’s needs to gain new or retain existing employment.
Individual placement and support in primary care
In depth support, focussing on personalised job matching and wrap around support to find and retain work.
When support provided
Employment Advisers (EAs) in NHS Talking Therapies
Before treatment starts, during treatment, between treatment and for a limited period post discharge from treatment.
Individual placement and support for severe mental illness
After self-referral or referral from a secondary care, primary care or voluntary sector team. Clients should be offered IPS on accessing the service and during any subsequent reviews.
Individual placement and support in drug and alcohol treatment
Clients are informed about IPS when first accessing the service. They can access IPS at any point in their structured treatment journey, and should be offered IPS upon accessing the service, through key working and at 6-month reviews.
Individual placement and support in primary care
Individuals will be referred by their GP or can self-refer. Other organisations including Jobcentre Plus will sign-post individuals to the support.
Number of sessions
Employment Advisers (EAs) in NHS Talking Therapies
Between one to six sessions as standard, average of four sessions. More if required.
Individual placement and support for severe mental illness
As many sessions as required over the period the client is accessing IPS.
Individual placement and support in drug and alcohol treatment
Target is weekly meetings for first month and then fortnightly.
Individual placement and support in primary care
Target is weekly meetings for first month and then fortnightly.
Delivery models
Employment advisers (EAs) in NHS Talking Therapies
By phone, video conferences, face to face in person, in groups (virtual and in person).
Individual placement and support for severe mental illness
By phone, video conferences, face to face in person, in groups (virtual and in person).
Individual placement and support in drug and alcohol treatment
By phone, video conferences, face to face in person, in groups (virtual and in person).
Individual placement and support in primary care
By phone, video conferences, face to face in person, in groups (virtual and in person).
Length of intervention
Employment advisers (EAs) in NHS Talking Therapies
Typically, up to three to four months support, more if required, not unlimited.
Individual placement and support for severe mental illness
IPS is a time-unlimited service, meaning that there are no fixed limits to the duration of support. Clients may have multiple job starts and re-access the service after job loss. Services should monitor active caseload to ensure each ES can support 40 – 50 clients per year.
Individual placement and support in drug and alcohol treatment
Pre-employment support can be offered for up to 9 months, and in-work support for up to 4. These are soft limits and can be extended at the discretion of each team’s senior employment specialist.
Individual placement and support in primary care
Pre-employment support can be offered for up to 9 months, and in-work support for up to 4.
Additional support
Employment Advisers (EAs) in NHS Talking Therapies
Money guidance, access to food banks.
Individual placement and support for severe mental illness
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis.
Individual placement and support in drug and alcohol treatment
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis.
Individual placement and support in primary care
Access to welfare benefits advice is a core part of the offer. Additional advice, support and signposting on a case-by-case basis.
Linking with
Employment Advisers (EAs) in NHS Talking Therapies
Jobcentre Plus, employers, training and education providers, social housing providers, debt counsellors, food banks, trade unions, employment lawyers, law centres.
Individual placement and support for severe mental illness
Jobcentre Plus, health partners, employers, training and education providers, social housing providers, debt counsellors, food banks, trade unions, employment lawyers, law centres.
Individual placement and support in drug and alcohol treatment
Jobcentre Plus, mental health services and primary care, employers, training and education providers, social housing/supported housing providers, debt counsellors, employment lawyers, law centres.
Individual placement and support in primary care
Jobcentre Plus, mental health services and primary care, employers, training and education providers, social housing/supported housing providers, debt counsellors, employment lawyers, law centres.
Refer onto
Employment advisers (EAs) in NHS Talking Therapies
Access to Work mental health support, JCP, other employment support providers including IPS and specialist providers, for example ES for people with neurodiversity.
Individual placement and support for severe mental illness
Access to Work, IPS in D&A if co-occurring condition of SMI and drug/alcohol dependency if agreement reached that that would be a more appropriate setting.
Individual placement and support in drug and alcohol treatment
Other employment support providers, including IPS for SMI where the clients are also accessing secondary mental health services and if agreement reached that that would be a more appropriate setting.
Individual placement and support in primary care
Access to Work, community support, specialist provision.
Appendix 2. Overview of the models

Description of the models in appendix 2:
Employment advisers (EAs) in NHS Talking Therapies (formerly IAPT) for anxiety and depression:
- For people with anxiety and/or depression receiving NHS Talking Therapies treatment (in or out of work).
- Client, employment advisor and therapist work together to set employment goals and deliver a bespoke action plan.
- Access is via the NHS Talking Therapies service and offer can be taken up by the client at any time during treatment.
- Typically there are 1-6 sessions provided.
- Delivered by phone, video conferencing, face to face and in groups (virtual and in person).
Individual placement and support for severe mental illness:
- For people with severe mental illness or complex mental health (out of work, or at risk of losing their job).
- Employment specialists work with clients on rapid job searches, confidence building, CV development, employer engagement, interview techniques and reasonable adjustments.
- Open access for anyone with severe mental illness or complex mental health, at any time. Clients can self-refer or be referred into the service from a secondary care, primary care or voluntary sector team.
- No fixed time limits, but services should monitor active caseload to ensure each employment specialist supports 40 to 50 clients per year.
- Delivered by phone, video conferencing, face to face and in groups (virtual and in person).
Individual placement and support in drug and alcohol treatment
- For people in structured community treatment for drug and/or alcohol misuse (in need of support to find or retain employment).
- Employment specialists work with clients on rapid job searches, confidence building, CV development, employer engagement, interview techniques and reasonable adjustments.
- Access is via the community treatment team for drug and/or alcohol misuse and the offer can be taken up by the client any time during their treatment.
- Typically pre-employment support offered for 9 months, and in-work support for up to 4 months.
- Delivered by phone, video conferencing, face to face and in groups (virtual and in person).
Individual placement and support in primary care
- For people with common mental health or physical health disabilities (wants and is in need of support to find or to attain employment and not taking part in any other DWP funded employment programme).
- Employment specialists work with clients on rapid job searches, confidence building, CV development, employer engagement, interview techniques and reasonable adjustments.
- Access is via GP or self-referral. Other organisations, including Jobcentre Plus, will signpost individuals.
- Typically pre-employment support offered for 9 months, and in-work support for up to 4 months.
- Delivered by phone, video conferencing, face to face and in groups (virtual and in person).
Appendix 3. Mapping the patient cohorts who can receive access to employment support
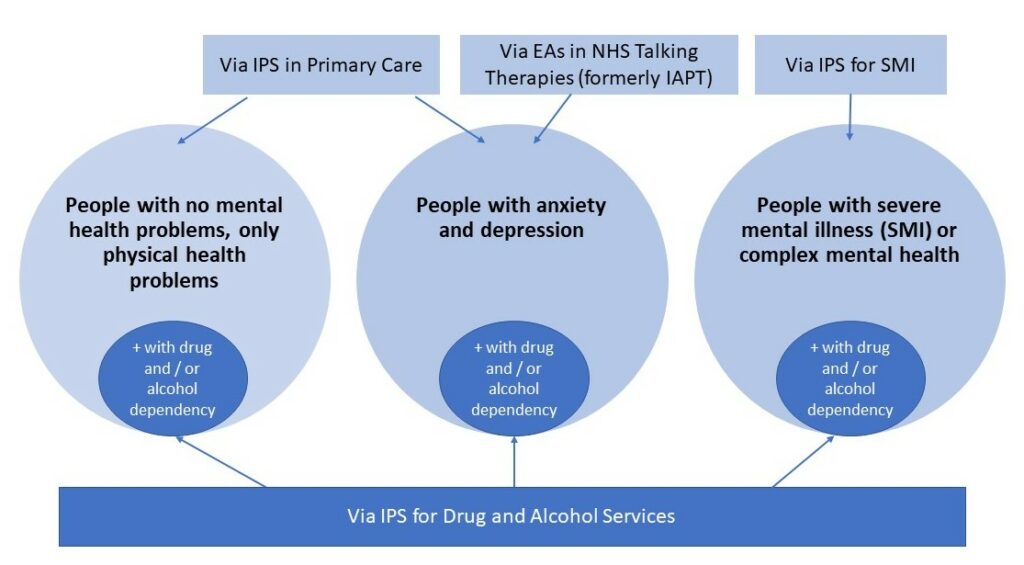
Image description:
People with no mental health problems, only physical health problems can access employment support via IPS in primary care. If they also have drug and/or alcohol dependency, they can also access employment support via IPS for D&A services.
People with anxiety and depression can access employment support via IPS in primary care and via EAs in NHS Talking Therapies. If they also have drug and/or alcohol dependency, they can also access employment support via IPS for D&A services.
People with severe mental illness or complex mental health can access employment support via IPS for SMI. If they also have drug and/or alcohol dependency, they can also access employment support via IPS for D&A services.
Acronyms
CMH = community mental health
CQC = Care Quality Commission
D&A = drugs and alcohol
EA = employment advisors
EIP = early intervention in psychosis
ES = employment specialist
ICB = integrated care board
ICS = integrated care system
IPS = individual placement and support
MDTs = multi-disciplinary teams
MHSDS = Mental Health Services Data Set
PCNs = primary care networks
SMI = severe mental illness
VCSEs = voluntary organisations, charities and social enterprises
Note: NHS Talking Therapies was formally referred to as ‘Improving Access to Psychological Therapies (IAPT)’.
References
[1] The evidence for IPS is drawn from 27 randomised controlled trials, originating from around 15 countries. Research by Brinchmann B et al (2019) concluded that IPS efficacy can be generalised between different countries and that the evidence of efficacy is very strong. IPS has demonstrated especially effective outcomes for young adults, including those with first episode psychosis.
[2] The EIP access and waiting time standard guidance also specifies that “As part of a comprehensive package of NICE care, individuals should be able to access IPS, either via the secondary mental health service or via other locally commissioned services”.
[3] Centre for Mental Health (2022) Briefing 59: IPS – a guide for ICSs.
[4] Royal College of Psychiatrists (2022) Addressing patients’ occupational, educational and psychosocial needs as an essential aspect of mental health care. A definition of “good work” is provided in this position statement. The 8 listed (but non-exhaustive) characteristics include job security, pay reflective of the role, safe and healthy environment, encouragement of productivity and prevention of isolation, appropriate autonomy and control, appropriate balance of power between workers and employer, work-life balance, appropriate career progression.
[5] The University of Manchester (2022) National confidential inquiry into suicide and safety in mental health (NCISH) found that 47% of patients who died by suicide in the UK during 2009 – 2019 were unemployed. A systematic review and meta-analysis of studies on midlife suicide similarly found that unemployment “was present in 43.2% of midlife suicide decedents and was associated with an almost fourfold increased risk of suicide.”
[6] Hoffmann H et al 2014 found that “the cumulative benefits of competitive work…[reduced] vulnerability to relapse and hospitalization”. Reme SE et al 2019 found that “the IPS group reported significant improvements in psychological distress, symptoms of depression, subjective health complaints, functioning, health-related quality of life, and global well-being, compared to the control group at 12-months follow-up.”
[7] Public Health England (2018) SMI and physical health inequalities: briefing. Compared to the general population, people under-75 in contact with mental health services in England have death rates that are: 6.6 times higher for respiratory disease, 6.5 times higher for liver disease, 4.1 times higher for cardiovascular disease and 2.3 times higher for cancer (NHS Digital (2021) Excess under 75 mortality rates in adults with serious mental illness – 2018 to 2020).
[8] Adult social care outcomes framework (ASCOF) data for England in 2021-22, which is based on the MHSDS, shows that nationally 6% of working age adults (18 – 69) who were in contact with mental health services at the end of the reporting month were recorded as being employed. Royal College of Psychiatrists (2021) National clinical audit of psychosis employment spotlight audit report, using a case-note sample of 4,935 of which 85% had an employment or education status recorded, highlighted that only 8% of people with psychosis were recorded as being in paid work.
[9] Office for National Statistics reports that the employment rate for 16 – 64 year olds was 75.1% in 2021.
[10] Ramsay CE et al 2011 found that, when asked, 80% of people experiencing first-episode psychosis said they wanted help finding a job. Gühne U et al 2021 found that 77.3% of people with SMI had a strong (59.8%) or moderate (17.5%) preference for employment.
[11] Hoffmann H et al (2014) found that the IPS group on average had approximately 60 days fewer inpatient bed days over a 5-year period. The Personal Social Services Research Unit (PSSRU) produces NHS national costing data for mental health services and states the average mental health bed day cost for 2021 was £428 (PSSRU (2021) Unit costs of health and social care). Therefore, the savings due to fewer bed days are conservatively £20,000 (and up to £25,000) per person over 5 years.
[12] SMI defined here as per the NHS Long Term Plan. Complex mental health includes difficulties associated with a diagnosis of a ‘personality disorder’.
[13] An appointment is referred to as a “care contact” in all MHSDS guidance. Face-to-face, video or telephone appointments count towards the access target, as well as talk type for a person unable to speak. Any other methods, such as email or SMS, do not count as access.
[14] On the clinical system, the appointment will need to be recorded as a clinical contact rather than an administrative contact for it to count towards access. If a client does not agree to partake in the IPS service during the initial session, it should be counted as an administrative contact rather than clinical and will not count towards access. Page 50 of the NHS Digital (2022) MHSDS v5.0 user guidance, states that for all care contacts (not just initial ones): “activities typically completed by administrative staff where the primary purpose of that activity is administrative in nature (arranging appointments, appointment reminders, notification of test results) via any consultation mechanism should not flow. There may be instances where administrative staff perform activity relevant to the person’s care (for example, recording of outcome measures). In these cases that activity should flow.” It is worth noting that to enable activity to flow into MHSDS, it will need to be labelled as “clinical” rather than “administrative” on the clinical system. This is true for all activity, not just initial appointments.
[15] The IPS fidelity model does not restrict systems from extending referrals to GPs or primary care. IPS should be prioritised for integration in CMH teams and in PCNs. Systems should consider the following enabling actions: using flexibilities of existing contracts or contract variations/planned re-commissioning rounds to open up IPS access to people with SMI in primary care; simplifying pathways and relationships with clinical teams to support clients referred from primary care; developing organisational arrangements with PCNs for the purposes of providing clinical oversight and managing clinical risk of primary care clients in IPS; establishing formalised collaboration between the IPS workers and primary care and/or co-location of teams; supporting the sharing of data and reporting of IPS access through the MHSDS.
[16] Note that all IPS D&A services should flow data to the National Drug Treatment Monitoring System (NDTMS).
[17] NHS Confederation (2020) Ensuring appropriate employment support for people with mental health problems.

