To:
- Integrated care board and trust:
- chief executives
- chief operating officers
- chairs
- chief people officers/human resource (HR) directors
- medical directors
- directors of nursing
- directors of communication
cc:
- Regional:
- directors
- performance and improvement directors
- medical directors
- directors of nursing
- directors of workforce
- deputy directors for emergency preparedness, resilience and response
- directors of communication
Dear colleagues
Industrial action by BMA resident doctors – 14 to 19 November 2025
The BMA resident doctors committee has announced industrial action from 7:00am on Friday 14 November to 6:59am Wednesday 19 November.
This letter outlines the approach being taken by NHS England and the steps we are asking you to take ahead of, during, and after industrial action.
Preparing for industrial action
We all now have significant experience of dealing with industrial action and we ask that you use that existing knowledge to inform planning ahead of this action. This will include moving staff and resources to focus on the following priorities:
- maintaining emergency care, including maternity services
- maintaining flow, ensuring appropriate and efficient discharge and length of stay
- maintaining elective care to the fullest extent possible – with at least 95% of elective activity continuing when compared to the level that would otherwise have been scheduled
- maintaining priority treatments, including urgent elective surgery and cancer care
It will be important for systems and trusts to try to maintain normal levels of booked activity and consider what is cancelled over the entirety of the cumulative period of disruption (both on the days of action and the days either side). Particular attention should be given to planning urgent elective surgery (P1 and P2), cancer care (particularly for patients who have already been waiting over 62 days, or who are likely to pass day 62 if their appointment needs to be rescheduled), and long waiters.
Reducing volumes of bookings and rescheduling appointments and other activity should only happen in exceptional circumstances to safeguard patient safety. This should be undertaken in consultation with your NHS England Regional Chief Operating Officer.
Maintaining at least 95% of elective activity is a minimum requirement, with the expectation that many providers will deliver higher than this level.
Reporting expectations
Pre action – risk self-assessment for ICBs
We understand the likely impacts of resident doctor action based on previous experience. Rather than a full pre-action assurance and assessment, we are asking ICBs to identify and quantify the following, using the same risk template as issued previously, in July 2025:
- patient safety concerns
- significant service changes, including reduced volumes of planned activity
- operational and service delivery risks and issues.
- staffing and rota fill levels
- risks from concurrent events or issues (for example, IT upgrades and major events).
ICBs should share this intelligence with NHS England regional teams and will be advised regionally of this deadline.
A copy of the self-assessment template is enclosed with this letter.
Pre action – estimate of elective impacts
NHS England will conduct 2 pre-action SitRep data collections via the Strategic Data Collection Service (SDCS):
- Activity sitrep:
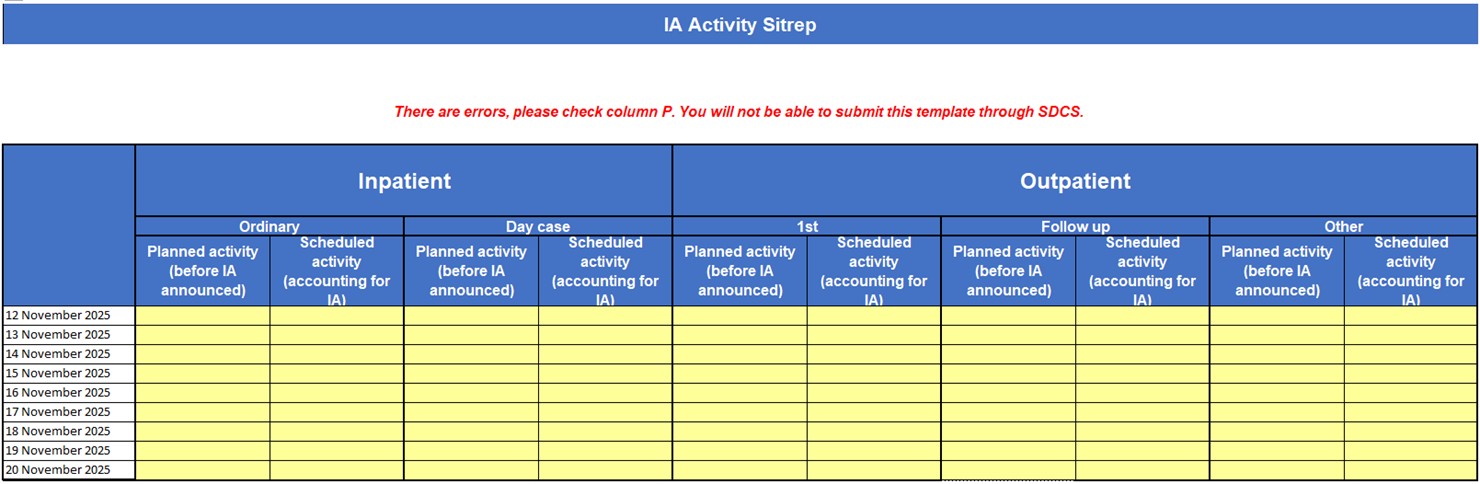
This is a new sitrep that will be collected from acute trusts on Tuesday 11 November 2025 and will collect planned activity (run rates) and scheduled activity (accounting for industrial action) for inpatient and outpatient activity for each day of the period 12 November to 20 November 2025. This data will be used to show the extent to which providers are planning to maintain elective activity to the fullest possible extent during industrial action. The collection will open at 9am on Tuesday 11 November 2025 and the deadline for submission is 4pm the same day. The template will be available to download from SDCS from 9am on the day the collection is running.
A screenshot of the template for this can be found in Annex B. Guidance for completion will be provided directly to registered submitters.
All acute trusts are requested to submit data.
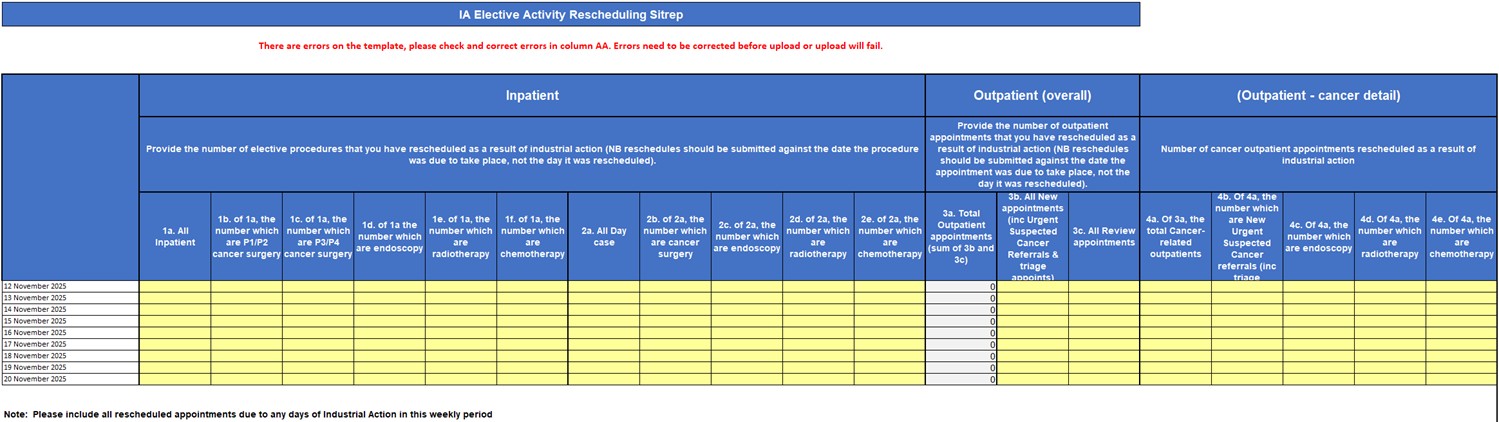
- Industrial action rescheduled activity sitrep:
This will collect information from acute trusts on activities rescheduled due to industrial action. The collection will request the figures of rescheduled activity for the 9-day period of 12 November to 20 November inclusive. This collection will be open at 9am on Wednesday 12 November and the deadline for submission is 1pm on Thursday 13 November. A screenshot of the template for this can be found in Annex D. Guidance for completion is provided as Annex E.
All acute trusts are requested to submit data, even if it is a nil return.
Data collections during industrial action
On the days of action, trusts and ICBs should consider the impact on patient safety and aim to mitigate this using normal operational procedures, including escalation of operational pressures escalation levels (OPEL) and actions and critical incident declaration for operational pressures.
NHS England will request updates through regional teams on the impacts of any escalating pressures, and will respond to operational and critical incident declarations as normal.
No new formal (national) industrial action data collections are planned on the days of action.
Any concerns about patient safety should be addressed at a local level, wherever possible. Where concerns cannot be addressed locally, they should be escalated through normal operational channels to NHS England regional teams.
NHS England executives will, however, be monitoring hospital activity closely using the Acute Healthcare Operational Data Flow (HODF) collection, which was previously referred to as ‘faster data flows data’. It is therefore essential that the data you submit through this collection is accurate, complete, and submitted on time.
HODF returns will offer the most timely indication of the extent to which providers have maintained elective activity levels. Please review your current data submission processes and take any necessary steps to ensure that:
- submissions are made daily by 10am, covering all activity up to midnight the previous day. Resubmissions to cover the period before the industrial action can also be accepted. This should happen no later than the 10 am on 14 November to cover 31 October to 13 November inclusive, with the data being submitted daily up to and including 20 November
- data quality checks are in place to identify and resolve any discrepancies. Details of these are set out in Annex F
- relevant teams understand the importance of maintaining data continuity during industrial action and appropriate business continuity plans are in place to support the actions above
This ask is in line with the ongoing work to improve acute HODF data quality. Details have already been shared with analytical teams and we are working toward making this the main, timely data source for future crisis management decision making in the NHS.
Throughout the period of industrial action, you will be provided with daily emails summarising your trust’s position, based on your HodF data, and you will be asked to provide confirmation that the information is accurate.
Post action data collections
NHS England will conduct 2 sitrep data collections through the Strategic Data Collection Service (SDCS):
- Industrial action workforce sitrep.
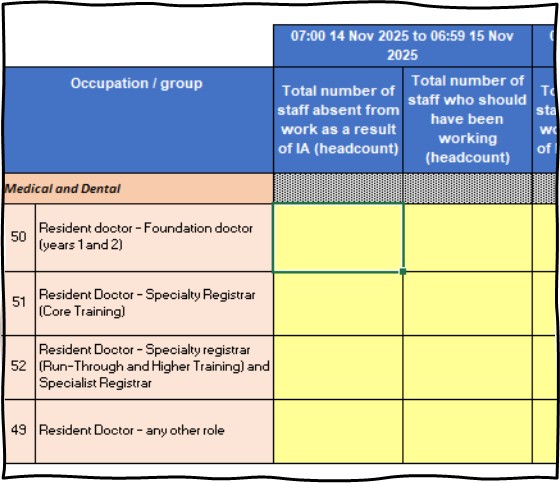
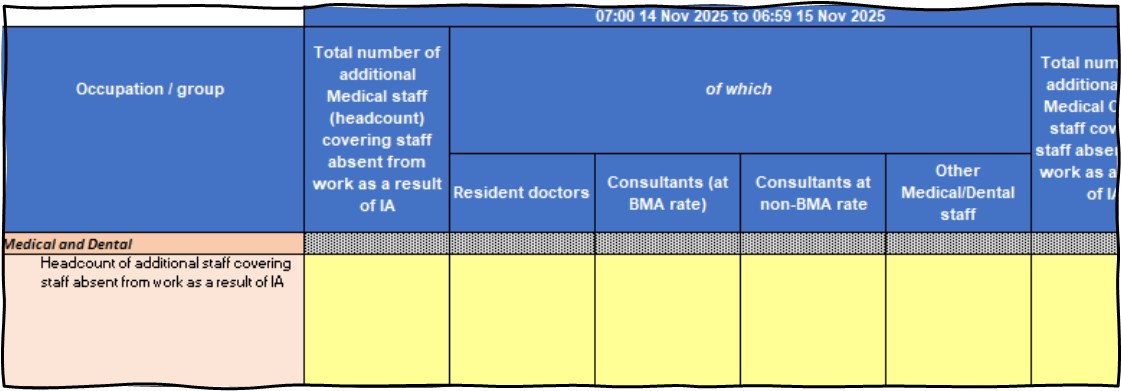
This will collect numbers of staff taking part in the industrial action and the total numbers of staff due to be at work. This data will be collected once and will open at 9am on Wednesday 19 November and close at 1am on Thursday 20 November. The template will be available to download from SDCS from 9am on the 1st day the collection is running. A screenshot of the template for this can be found in Annex C. Please note the new requirement to distinguish between different resident doctor grades and plan to capture this information in advance.
All provider trusts (including ambulance, mental health, community and acute trusts) are requested to submit data, even if it is a nil return.
- Industrial action rescheduled activity sitrep:
This will collect information from acute trusts on activities rescheduled due to industrial action. The collection will be open for all acute trusts and will request the figures for rescheduled activity for the 9-day period of 12 November to 20 November inclusive. Submissions will be made through the SDCS platform, which will open at 9am on Wednesday 19 November and close at 1pm on Thursday 20 November. It will not be reopened. A screenshot of the template for this can be found in Annex D. Guidance for completion is provided in Annex E.
All acute trusts are requested to submit data, even if it is a nil return.
All acute organisations are required to upload a return where there are any changes to the rescheduled submission made prior to the action.
Missing returns will be highlighted to regional chief operating officers for follow-up.
Highlights of the data collected for 12 November to 20 November 2025 will confirm the summary position following the period of industrial action, and will be published on NHS England’s website.
Recovering from industrial action
As well as managing the period of industrial action effectively, it is important that recovery is strong and activity levels do not fall in the weeks that follow.
We therefore ask that you plan beyond the period of industrial action. NHS England regional teams will continue to provide support and will monitor real-time data to identify and address issues promptly.
Given that we will soon be in the main winter period, this level of oversight and support may need to remain in place through to January. We will take stock of this toward the end of November and discuss it with you.
Patient safety mitigation approach
We acknowledge that, despite the comprehensive contingency plans being put in place, there may still be circumstances where mitigations are insufficient, and that there may be a need to request resident doctors return to work for a limited period in order to maintain safe patient care.
This measure is not in place to avoid disruption caused by strike action. It is in place to ensure that, in unexpected and extreme circumstances, patients will continue to receive safe care. It is designed to be responsive to patient safety concerns arising during strike action, rather than pre-empting the impacts of strike action.
Where local resolution can’t be reached, the following clinical escalation route should be followed:
- Clinical director of the relevant service.
- Trust medical director.
- Regional medical director.
Only after this process has been fully followed will a request be considered nationally — and, if appropriate, escalated to the BMA. This ensures national decisions are well-evidenced and clinically justified.
To support this, we have a national multidisciplinary team on hand to review requests promptly and provide a clear and timely response when required.
Trust medical directors — supported by regional medical directors — are best placed to make judgements about what can safely proceed. While the primary clinical discussion is direct from provider to region, providers should also ensure their ICB is made aware of this request, to ensure the ICB can maintain its system oversight of industrial action. This is the model we continue to work to: clinically led, locally driven, and focused on patients.
Once the BMA has approved a derogation, a local trust may contact resident doctors and seek their return to work.
Resident doctors on strike need not return to work unless the need for derogations is confirmed by the BMA.
That being said, NHS England and the BMA both recognise it may be necessary, as an exception, for a trust to contact resident doctors in the event of a mass casualty event, explaining the situation and seeking their immediate return to work, while simultaneously escalating the situation as described above.
The derogation / patient safety mitigation request form is enclosed with this communication to reduce administrative burden and to enable timely decision-making.
Management of training and deployment
Resident doctors can be redeployed during industrial action if this is necessary to ensure patient safety and no other staff are available to cover. Prior approval is required from the postgraduate dean and doctors should not be placed outside their area of competence. Those choosing not to strike are advised to remain in familiar clinical areas to maintain patient safety, with proper induction and supervision if redeployed.
Doctors participating in industrial action must not take locum or bank shifts elsewhere, as this raises professionalism concerns. Should this occur, a discussion should take place with the Postgraduate Dean as Responsible Officer.
Time taken for industrial action counts as absence from training and may affect progression, triggering reviews if thresholds are exceeded, as outlined in the Gold Guide. All absences must be reported appropriately.
Missed teaching due to strikes should be rescheduled before programme completion to ensure training continuity. Further information is available at Annex A.
BMA rate care and pay rates
The British Medical Association (BMA) has re-introduced its own guidance on standard pay rates for consultants in England when participating in non-contractual work.
Bank (Locum) pay rates are determined locally and negotiating mechanisms through providers should be maintained. NHS England expects that providers should not adopt the BMA’s rate card or, where this has been agreed previously, this should be re-evaluated. We strongly encourage collaborative arrangements with neighbouring trusts, with data sharing agreements across local ICBs to minimise competition between organisations. Where incentivised pay rates are offered, we expect those to be within the normal ranges and not raised in response to industrial action (that is: negotiated upward to keep services safe).
The NHS Employers website offers guidance on extra contractual work.
Many thanks for your continued cooperation and support in providing this information and ensuring a high return rate.
Yours sincerely,
Mike Prentice, National Director for Emergency Planning and Incident Response, NHS England
Annex A – Management of training and deployment
Redeployment
Redeployment of resident doctors, where needed to ensure patient safety and where other staff are not available to cover, is possible in line with the current guidance. Prior approval is needed from the postgraduate dean. However, given that it is likely there will be an impact on all clinical settings, resident doctors who choose not to strike are probably better remaining in their usual areas of work, working with senior colleagues and other staff to ensure a safe patient environment instead of moving to an unfamiliar setting. If redeployment is necessary, a clear departmental induction and provision for clinical supervision is necessary. No doctor in postgraduate training should be expected to work outside their area of competence.
If a resident doctor has chosen to take industrial action, they should not undertake a locum or bank shift elsewhere in the NHS. This should be regarded as a professionalism issue and there should be a discussion with the postgraduate dean as Responsible Officer.
Training time absence allowance
Time out for industrial action counts towards absences from training and therefore the following guidance in the Reference Guide for Postgraduate Foundation and Specialty Training in the UK (Gold Guide) applies:
Absences from training can impact on certification (or completion) date:
3.183: Absences from training (including OOP not approved towards training), other than for study leave or annual leave, may affect an individual’s ability to demonstrate capability and progression through the curriculum. The GMC has therefore determined that within each 12-month period where a postgraduate doctor in training has been absent for a total of 14 days or more (when they would normally be at work), a review will be triggered of whether they need to have their core training programme end date or their CCT date extended. This review would normally occur at the ARCP.
3.185: For foundation doctors, where a postgraduate doctor in training has been absent for both statutory (for example, maternity/paternity/adoption) and non-statutory reasons for a total of 20 working days or more within each 12-month period, an early review will be triggered with regard to whether they need to have their F1 or F2 training extended. The duration of provisional registration regulations must be taken into account.
3.186: The GMC’s Good Medical Practice states that it is the responsibility of each individual postgraduate doctor in training to be honest and open, and to act with integrity. As such, they should ensure that NHSE WTE, NES, HEIW or NIMDTA is aware of their absences through the relevant reporting processes. This information will be shared with the relevant College/Faculty and the GMC.
It is vital that our foundation doctors and resident doctors in specialty training programmes can continue to progress in their training and that informed decisions can be made about their progression. We are therefore reminding you of the requirement to record any time out of training that occurs due to industrial action so that we can monitor the impact on their training. We will require this to be submitted along with the wider SDCS return.
Training and teaching scheduled for strike days
Any formal teaching or training that cannot take place, either because trainers can’t be released to provide teaching or resident doctors who are not taking part in industrial action are not able to be released, should be delivered on an alternative day, prior to resident doctors rotating or completing their programme.
Annex B – screenshot of activity sitrep
Annex C – screenshot of workforce sitrep
Part A
Part B
Annex D – screenshot of industrial action rescheduled activity sitrep
Annex E – Guidance for industrial action sitrep collections – November 2025
Rescheduled activity sitrep
Column name | Guidance |
|---|---|
|
Date |
Specify the day that the appointment was originally planned for |
|
1a. All inpatient |
A count of all standard inpatient (that is, Not Day case) appointments or procedures scheduled for the specified date that have been changed by the provider due to industrial action. This includes both appointments where a new date has been provided and those where a new date has not yet been confirmed. |
|
1b. of 1a, the number that are P1 or P2 cancer surgery |
Of all those in 1a, the number that were for P1 or P2 surgeries relating to a cancer pathway. |
|
1c. of 1a, the number that are P3 or P4 cancer surgery |
Of all those in 1a, the number that were for P3 or P4 surgeries relating to a cancer pathway. |
|
1d. of 1a the number that are endoscopy |
Of all those in 1a, the number that were for endoscopies relating to a cancer pathway. |
|
1e. of 1a, the number that are radiotherapy |
Of all those in 1a, the number that were for radiotherapy. |
|
1f. of 1a, the number that are chemotherapy |
Of all those in 1a, the number that were for chemotherapy. |
|
2a. All Day case |
Any Day Case inpatient appointment/ procedure scheduled for the specified date that has been changed by the provider due to industrial action. This includes both appointments where a new date has been provided and those where a new date has not yet been confirmed. |
|
2b. of 2a, the number which are cancer surgery |
Of all those in 2a, the number that were for surgeries relating to a cancer pathway. |
|
2c. of 2a, the number which are endoscopy |
Of all those in 2a, the number that were for endoscopies relating to a cancer pathway. |
|
2d. of 2a, the number which are radiotherapy |
Of all those in 2a, the number that were for radiotherapy. |
|
2e. of 2a, the number which are chemotherapy |
Of all those in 2a, the number that were for chemotherapy. |
|
3a. All outpatient appointments (sum of 3b & 3c) |
This is a count of all outpatient appointments or procedures scheduled for the specified date that have been changed by the provider due to industrial action. This includes both appointments where a new date has been provided and those where a new date has not yet been confirmed. This cell is auto calculated from the contents of 3b and 3c. Do not try to enter data directly into this column. |
|
3b. All new appointments (including urgent suspected cancer referrals and triage appoints) |
Of all those in 3a, how many rearranged appointments are new appointments, including those from an urgent suspected cancer referral, including triage appointments. |
|
3c. All review appointments |
Of all those in 3a, how many rearranged appointments are review appointments. |
|
4a. Of 3a, all that are cancer-related |
Count of all cancer related outpatient appointments or procedures scheduled for the specified date that have been changed by the provider due to industrial action. This includes both appointments where a new date has been provided and those where a new date has not yet been confirmed. |
|
4b. Of 4a, the number that are new urgent suspected cancer referrals (including triage appoints) |
Of all those in 4a, how many rearranged appointments are new, urgent suspected cancer referral appointments, including triage appointments. |
|
4c. Of 4a, the number that are endoscopy |
Of all those in 4a, how many rearranged appointments are for a endoscopy appointment relating to a cancer pathway. |
|
4d. Of 4a, the number that are radiotherapy |
Of all those in 4a, how many rearranged appointments are for a radiotherapy appointment. |
|
4e. Of 4a, the number that are chemotherapy |
Of all those in 4a, how many rearranged appointments are for a chemotherapy appointment. |
New request from November 2025: Additional activity sitrep to capture current planned activity levels
Planned activity (before industrial action announced): the level of activity that trusts planned for on each day prior to any announcement of industrial action. This should align with monthly plans submitted in the 2025/26 planning round.
Scheduled activity (accounting for industrial action): The level of activity on each day that trusts are currently expecting to deliver, taking into account industrial action.
These figures should align with the activity definitions used for planning (see below). For all activity, we’re asking for NHS-commissioned activity for specific acute treatment functions.
Ordinary admission: Any patient admitted electively with the expectation that they will remain in hospital for at least 1 night, including a patient admitted with this intention who leaves hospital for any reason without staying overnight, should be counted as an ordinary admission. A patient admitted electively with the intent of not staying overnight, but who does not return home as scheduled, should also be counted as an ordinary admission.
Day Case admission: must be an elective admission, for which a ‘decision to admit’ has been made by someone with the ‘right of admission’. Any patient admitted electively during the course of a day with the intention of receiving care, who does not require the use of a hospital bed overnight and who returns home as scheduled, should be counted as a day case. If this original intention is not fulfilled and the patient stays overnight, such a patient should be counted as an ordinary admission. Where clinical care is provided as a series of day case activities (for example, chemotherapy or radiotherapy), this should be recorded as regular day or night activity (and therefore not be included in the day case count).
Outpatient attendance: A count of all outpatient attendances taking place within the period, whether taking place within a consultant clinic session or outside a session.
Specifically, the number of outpatient attendances for which:
‘Attended or did not attend code’ = 5 or 6
‘Treatment function code’ is not 812 (diagnostic imaging)
Split by 1st attendance, follow up attendance or other (including not known), we would normally expect ‘other’ to be zero.
Note that 2025/26 planning definitions are also available at Activity and Performance Guidance – NHS Planning – Futures (requires a Futures account). See EM10a and EM10b for elective inpatient definitions and EM8 and EM9 for the outpatient definitions.
Workforce sitrep
Reference to occupation codes are as defined in version 19.0 of the NHS Occupation Code Manual:
National workforce data set (NWD) and NHS occupation codes
For completion of the sitrep, include all staff in the relevant occupation codes within the sitrep group.
For any additional staff not specified, provide total numbers in the ‘other occupational group’ line.
Total number of staff absent from work – only include those who are absent due to industrial action.
Total number of staff who should have been working – headcount of those who should have been working if no one was absent.
Staff taking part in industrial action should be reported by the organisation where the staff member would have been working had they not been on strike that day. Where the organisation the staff member would have been working is not an NHS trust or ICB (for example, a junior doctor working in general practice), the NHS trust that is their lead employer should include them in their report. It is important that staff involved in the action are only reported once.
Medical and dental staff groups
Sitrep group | Occupation codes |
|---|---|
|
Medical and Dental |
M* |
|
Medical / dental – consultant |
Not applicable |
|
Resident doctor – in foundation or specialty training including GP |
Include all relevant staff with occupation codes beginning with ‘M’. |
|
Resident doctor – any other role
| |
|
Medical / dental – other (for example staff, associate specialist and specialty (SAS)) | |
|
General medical / dental practitioner |
Nursing and midwifery staff groups
Sitrep group | Occupation codes |
|---|---|
|
Nursing staff and midwives |
NMC Registered NA, NC, NE, N0-7, NB |
|
Adult and general |
N*A |
|
Mental health |
N*D, N*E |
|
Learning disabilities |
N*F, N*G |
|
Children and young people |
N*B, N*L |
|
Midwives |
N2C |
|
Maternity support workers |
N9C |
|
Health visitors |
N3H |
|
District or community |
N*H, N*K, exclude N3H |
|
Other registered nurses |
N*J, P2*, P3*, N*C exclude N2C |
|
Nursing associates, support to NMC registered and students | |
|
Student nurses |
P1* |
|
Nurse associates |
NG*, NF* |
|
Trainee nurse associates |
NH* |
|
Nursing auxiliary / nursing assistant / healthcare assistant (including Health / clinical / nursing support worker) |
H1*, H2*, exclude H*P and H*R N8, N9* exclude N9C |
Ambulance staff groups
Sitrep group | Occupation codes |
|---|---|
|
Ambulance staff |
A |
|
Consultant paramedic Advanced paramedic Specialist paramedic |
A4* A5* A6* |
|
Paramedic |
AB* |
|
Assistant practitioner Emergency / urgent care support worker |
A7* A8* |
|
Ambulance technician / associate practitioner |
AE* |
|
Emergency call handlers Emergency medical dispatchers |
A8E |
|
Non-emergency call handlers Non-emergency medical dispatchers |
G2E, G3E |
|
Ambulance care assistant |
A9C |
Other staff groups
Sitrep group | Occupation codes |
|---|---|
|
Scientific, therapeutic and technical Staff |
S |
|
Occupational therapy |
S*C |
|
Physiotherapy |
S*E |
|
Radiography – diagnostics and therapeutic |
S*F, S*G |
|
Pharmacy |
S*P |
|
Operating theatres |
S*T |
|
Applied psychology |
S*L |
|
Psychological therapy |
S*M |
|
Chiropody / podiatry Dietetics Orthoptics/optics Art/music/drama therapy Speech and language therapy Osteopathy |
S*A S*B S*D S*H S*J S*V |
|
Qualified other scientific, therapeutic and technical Multi therapies Dental |
S*X S*K S*R |
|
Assistant practitioner Student/trainee Assistant |
S5* S8* S9* Exclude S5U, S8U and S9U |
|
Healthcare science and public health Scientific staff |
U |
|
Life sciences |
U*A, U*B, U*C, U*D |
|
Physiological sciences | U*E, U*F, U*G |
|
Physical sciences and biomedical engineering |
U*H, U*J |
|
Clinical bioinformatics |
U*K |
|
Public health sciences |
U*L, U*M |
|
Social services |
S*U |
|
Social workers |
S1U, S6U, S7U |
|
Social care managers |
S0U |
|
Social care support staff |
S5U, S8U, S9U |
|
Administration and estates staff |
G, H |
|
Central functions |
G*A, H*P |
|
Hotel, property and estates |
G*B, H*R |
|
Scientific, therapeutic and technical support |
G*C Directly supporting patient care but with no direct patient contact |
|
Clinical support |
G*D Directly supporting patient care in a clinical area (for example, medical records clerk, medical secretary) |
Additional healthcare professionals providing cover for staff on strike
To calculate more refined estimates of the full national cost of industrial action, additional information is requested to capture the number and type of staff who worked in addition to normal planned rotas on days of industrial action.
These columns should be used only for the number additional staff (headcount) brought in to provide cover for those on, or expected to be on, strike (that is: i.e. staff who would not normally have been scheduled to work on that day).
The total number (headcount – whole number) for additional ‘medical’ and ‘non-medical clinical’ staff is mandatory; the breakdown by type is optional. However, please complete on best endeavours all the ‘of which’ type fields for which there are headcount estimates available within the timeframe. An optional comments box will be provided to provide brief notes (to a maximum of 255 characters) to help interpretation of the information or to highlight any limitations of national use.
New metric 1: Total number of additional medical and dental staff (headcount) covering staff absent from work as a result of industrial action for the period of action (each day) [mandated]
- Total number of additional medical and dental staff employed on the strike day to provide cover for staff taking (or expected to take) industrial action.
- 1a: of which resident doctors
- additional medical/dental doctors in training (for example, F1, F2s, StRs, SHOs, SpRs/SpTs/GPRs) employed on the strike day to provide cover for staff taking (or expected to take) industrial action
- 1b: of which consultants at BMA rate
- additional consultants employed at BMA non-contractual rate card on the strike day to provide cover for staff taking (or expected to take) industrial action. Please report in the consultant non-BMA rate category (1c) if there is a time constraint in identifying consultant BMA rate and non-BMA rates
- 1c: of which consultants at non-BMA rate
- additional consultants employed at non-BMA extra-contractual rate on the strike day to provide cover for staff taking (or expected to take) industrial action. Please report in the consultant non-BMA rate category (1c) if there is a time constraint in identifying consultant BMA rate and non-BMA rates.
- 1d: of which other medical/dental staff
- additional other medical or dental staff (for example, staff grade, associate specialist and specialty (SAS), LEDs employed on the strike day to provide cover for staff taking or expected to take industrial action)
New metric 2: Total number of additional non-medical clinical staff covering staff absent from work as a result of industrial action for the period of action (each day) [mandated]
- Additional non-medical clinical staff employed on the strike day to provide cover for staff taking or expected to take industrial action (for example, healthcare professionals who are not doctors or dentists but are involved in direct patient care and treatment).
Annex F – Healthcare Operational Data Flow (HODF) data quality requirements
To ensure reliable and consistent reporting, providers should:
- maintain consistency in daily submissionsfor all 001 APC Admission, 003 APC Discharge, and 004 Outpatient data collections, following the established standard:
- include all new, newly recorded, or changed admissions, discharges, or outpatient records within the 24-hour period (00:00:00 to 23:59:59) prior to the day of submission. (Reference: Healthcare Operational Data Flows: Acute Data Set – NHS England Digital)
- ensure completeness of key fields, as outlined in the Healthcare Operational Data Flows Acute Data Set Specification v1.0 – National Reporting – Futuresor the HODF Data Set on NHS Data Dictionary.
For 001 APC Admission and 003 APC Discharge:
- A) HOSPITAL PROVIDER SPELL IDENTIFIER – ID 16 (both datasets)
- B) ORGANISATION IDENTIFIER (CODE OF PROVIDER) – ID 3 (both datasets)
- C) LOCAL PATIENT IDENTIFIER (EXTENDED) – ID 8 (both datasets)
- D) START DATE (HOSPITAL PROVIDER SPELL) – ID 22 (Admission)
- E) METHOD OF ADMISSION (HOSPITAL PROVIDER SPELL) – ID 20 (Admission)
- F) INTENDED MANAGEMENT CODE – ID 26 (Admission)
- G) PATIENT CLASSIFICATION CODE – ID 20 (Discharge)
- H) DISCHARGE DATE (HOSPITAL PROVIDER SPELL) – ID 30 (Discharge)
Please note: Fields (a), (b), and (c) are essential for linking admission and discharge files, enabling accurate classification of activity types (Day Case, Ordinary Admission, and RDNA). Currently, an average of 9.1% of discharge records lack matching admission information, with variation across providers.
For 004 Outpatient:
- ORGANISATION IDENTIFIER (CODE OF PROVIDER) – ID 3
- APPOINTMENT DATE – ID 21
- ATTENDANCE STATUS – ID 25
- CONSULTATION TYPE – ID 27
For all collections:
- CDS UNIQUE IDENTIFIER – ID2
- NHS NUMBER – ID11
- POSTCODE OF USUAL ADDRESS – ID13
- PERSON BIRTH DATE – ID15
Please note: Field 1 is essentially for forming the primary key alongside ORGANISATION IDENTIFIER (CODE OF PROVIDER) in the 3 datasets. Failure to complete this column effectively makes the data submitted unusable after the primary key de-duplication is applied.
Field 2, 3 and 4 will allow for best leaky PID checks in the submitted data and also prevents large scale redaction to the various ID columns (which occurs when these are not provided).
- Where data submissions have been missed or there are gaps in the data that need rectifying, data can be resubmitted at any time.
While not the focus of this ask, please note that for the current collection (002) only, each day of admitted patient care needs a corresponding row of data. For example, if a patient remained in a bed from 1 to 3 October, we would expect 3 rows for the patient in the current inpatient admission with the following ReportingPeriodStartDate/ReportingPeriodEndDate:
- 2025-10-01
- 2025-10-02
iii. 2025-10-03
Monitoring and support
The HODF Data Quality Monitoring Tool can be used nationally, regionally, and locally to assess data coverage and completeness. It includes Admission and Outpatient data, is refreshed daily, and is accessible via FutureNHS: Acute HODF DQ Report – National Reporting – Futures (log-in required). 1-to-1 support is available to all trusts through the Data Liaison Service (DLS) to provide any clarifications required and support troubleshooting. Contact details for your regional data liaison manager can be found in the table below:
Region | Data liaison manager | Contact details |
|---|---|---|
|
East of England | Lynn Steele | Tel: 07702 422824 Email: l.steele2@nhs.net |
|
London | Jon Ensor | Tel: 07842 323478 Email: Jonathan.ensor@nhs.net |
|
Midlands | Paul Steele | Tel: 07985 215 306 Email: Paul.steele2@nhs.net |
|
North East and Yorkshire |
Ela Bonsall | Tel: 07592 397838 Email: ela.bonsall1@nhs.net |
|
North West |
Julie Whittaker | Tel: 07900 980528 Email: Julie.whittaker5@nhs.net |
|
South East |
Ross Jenkins | Tel: 07783 873761 Email: ross.jenkins1@nhs.net |
|
South West |
Antoinette Salvador | Tel: 07901118466 Email: antoinette.salvador@nhs.net |

