Executive summary
The NHS made further progress in reducing long waits for patients in February, despite disruption from another five days of industrial action and winter demand.
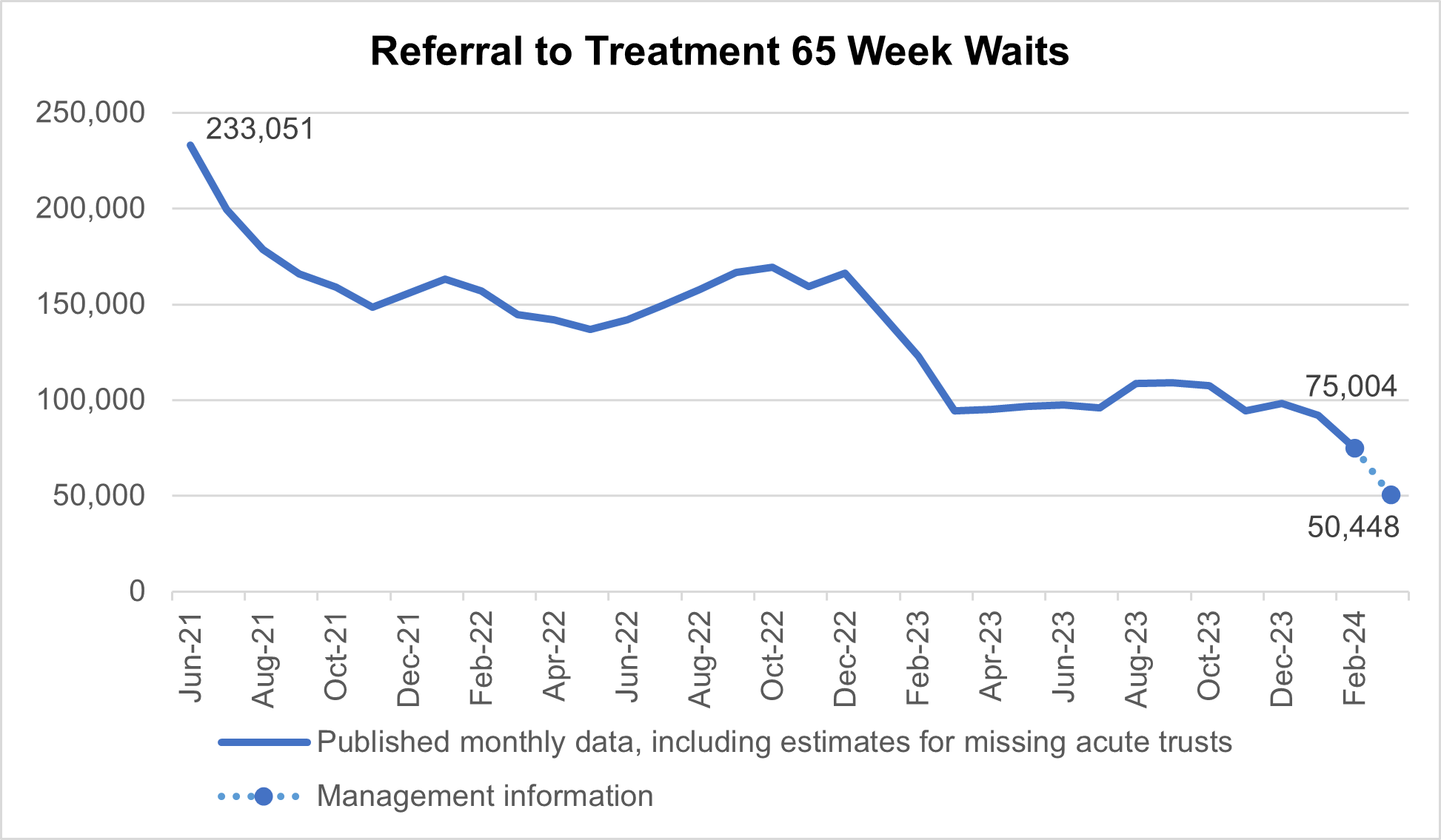
The number of patients waiting more than 65 weeks for treatment was 75,004 at the end of February, down by 19% from 92,213 in January and down by 68% from a peak of 233,051 in June 2021. Additional management data [1] published this month suggests a further reduction between February and March, with 50,448 patients waiting more than 65 weeks for treatment as of the end of March.
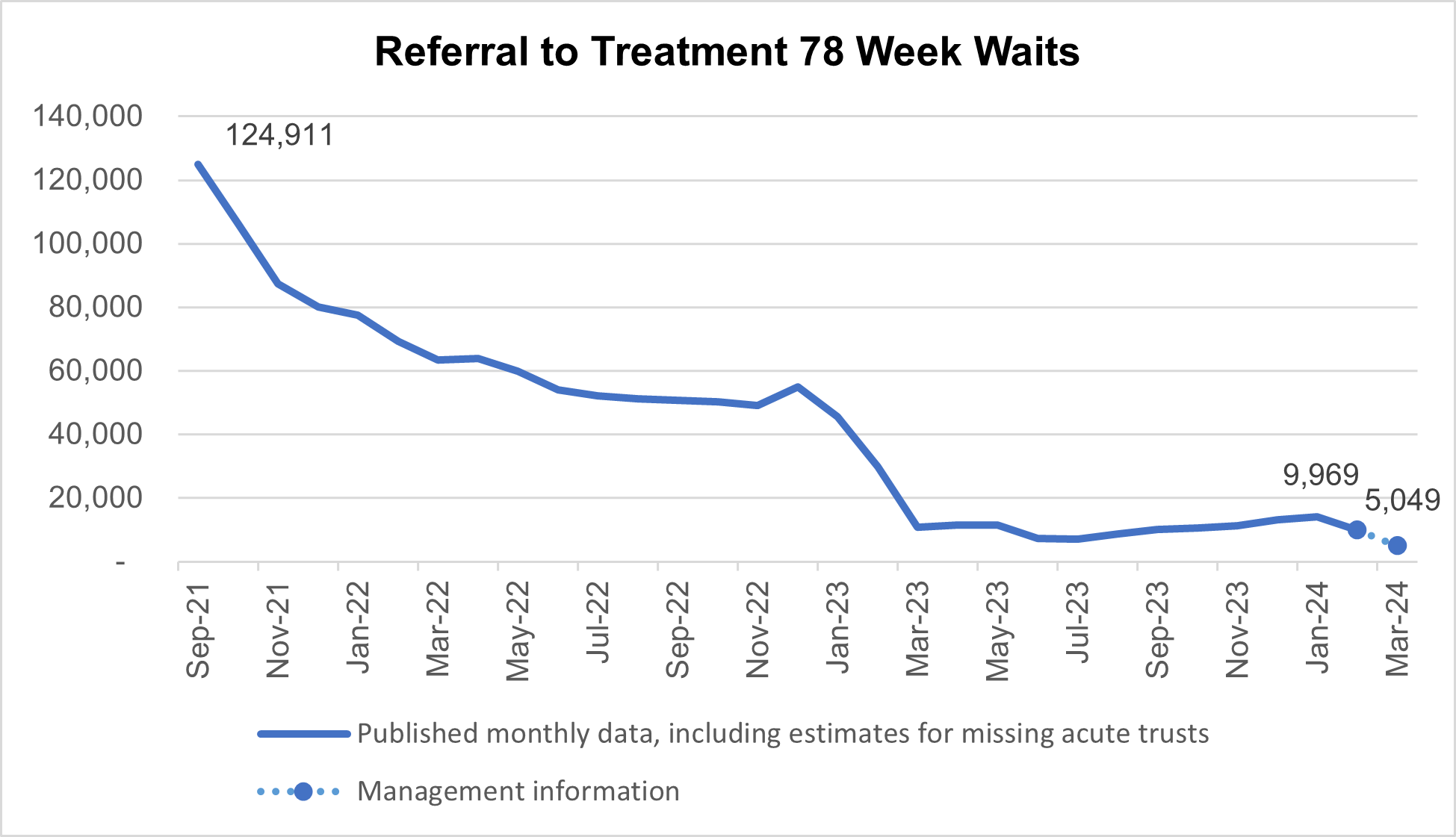
9,969 patients were waiting more than 78 weeks for treatment at the end of February, down 29% from 14,013 in January and down by 92% from a peak of 124,911 in September 2021. Additional management data suggests a further reduction between February and March, with 5,049 patients waiting more than 78 weeks for treatment as of the end of March.
In March, there were 2,352,113 attendances in A&Es across England. 74.2% of patients attending A&E were admitted, transferred or discharged within four hours. This compares to 70.9% in February and 71.5% in March 2023. Performance over the course of the year was significantly improved on last year.
Ambulance services answered 801,495 calls to 999, or 25,855 per day. There were 382,325 incidents where a patient was conveyed to an A&E. The average ambulance response time for a category 2 call was 33 minutes and 50 seconds. This is 5 minutes and 43 seconds faster compared to March 2023.
Almost 345,000 people received their first treatment for cancer over the last year between March 2023 and February 2024 – the highest year on record, and up by around 58,000 on the same period pre-pandemic.
In February 2024, 780,963 children and young people accessed NHS mental health services. The NHS is rolling out new initiatives, such as mental health support teams in schools and colleges which are on track to cover over 4 million pupils and learners in spring 2024, increasing to around 5 million in spring 2025.
[1] Management information for the latest month is taken from the Waiting List Minimum Dataset which is subject to less validation than the published monthly figures and does not include estimates for missing providers (133 of 135 acute trusts submitted data for the latest month).
Urgent and emergency care
The NHS’s delivery plan for recovering urgent and emergency (UEC) services set out two ambitions for improving patient flow through the pathway.
The first target was to admit, transfer or discharge 76% of patients in emergency departments within four hours of arrival by March 2024. The second was to improve ambulance response times for category 2 incidents to an average of 30 minutes over 2023/24.
These ambitions were created in response to a particularly pressured winter where patient ‘flow’ was slowed through hospitals due to discharge problems and demands from flu and Covid-19.
While progress was expected to vary throughout the year due to levels of demand, seasonality, and industrial action, the overall aim was to see continued improvement.
In March, there were 2,352,113 attendances in A&Es across England, of which 1,745,434 spent less than four hours in A&E and 606,679 were in A&E for more than four hours.
The year to March for A&E services saw 26.2 million attendances, up 6% on 24.8 million pre-pandemic (year to March 2019). The yearly average shows emergency admissions are up 6.4% on the preceding 12-month period.
74.2% of patients attending A&E were admitted, transferred or discharged within four hours. This compares to 70.9% in February and 71.5% in March 2023.
This means performance over the course of the year was significantly improved on last year.
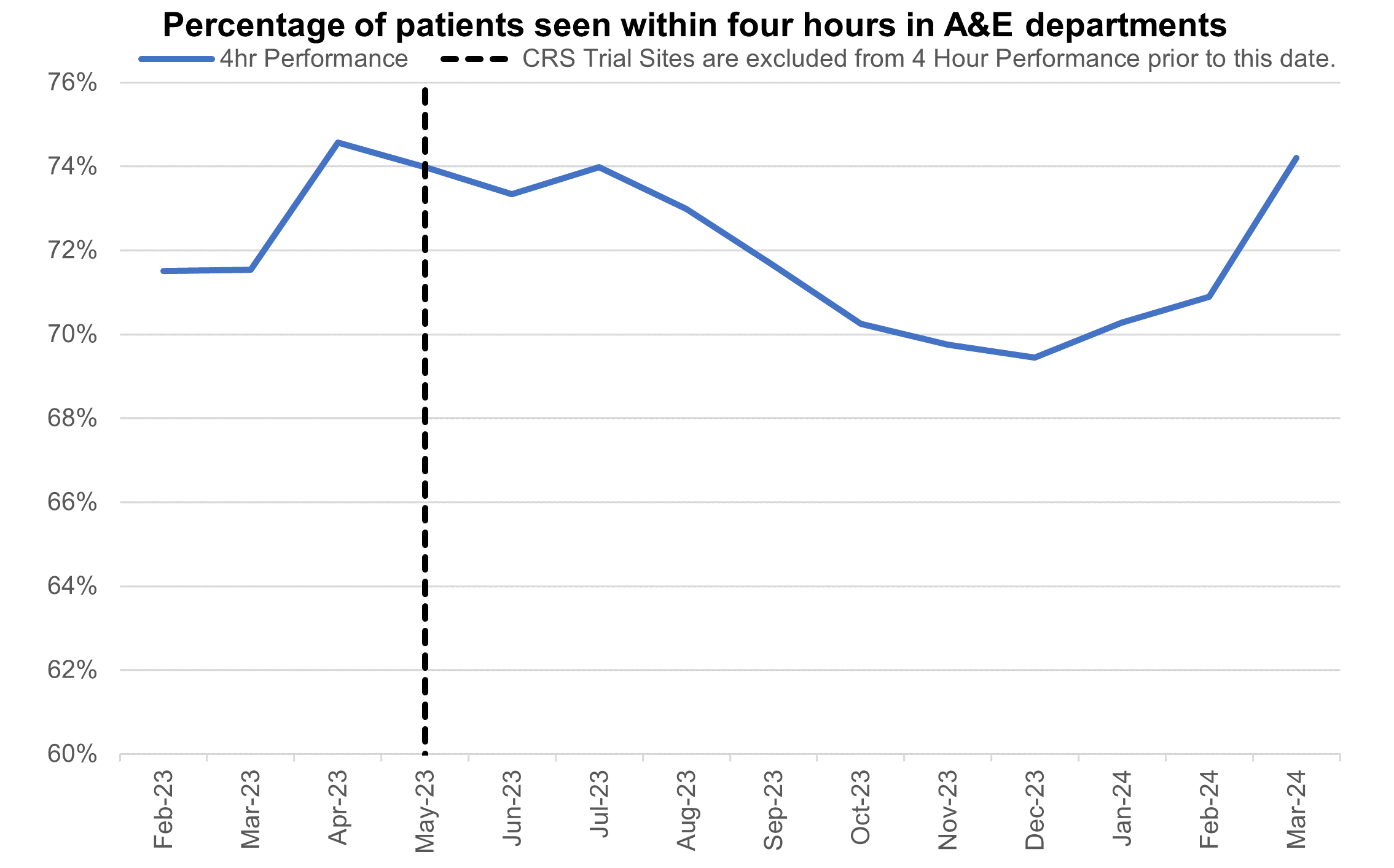
Percentage of patients seen within four hours in A&E departments
Ambulance services answered 801,495 calls to 999, or 25,855 per day. There were 382,325 incidents where a patient was conveyed to an A&E.
The average ambulance response time for a category 2 call was 33 minutes and 50 seconds. This is 5 minutes and 43 seconds faster compared to March 2023.
This means the category 2 mean response time for the whole year was 36 minutes 23 seconds, over 13 minutes faster than the previous year.
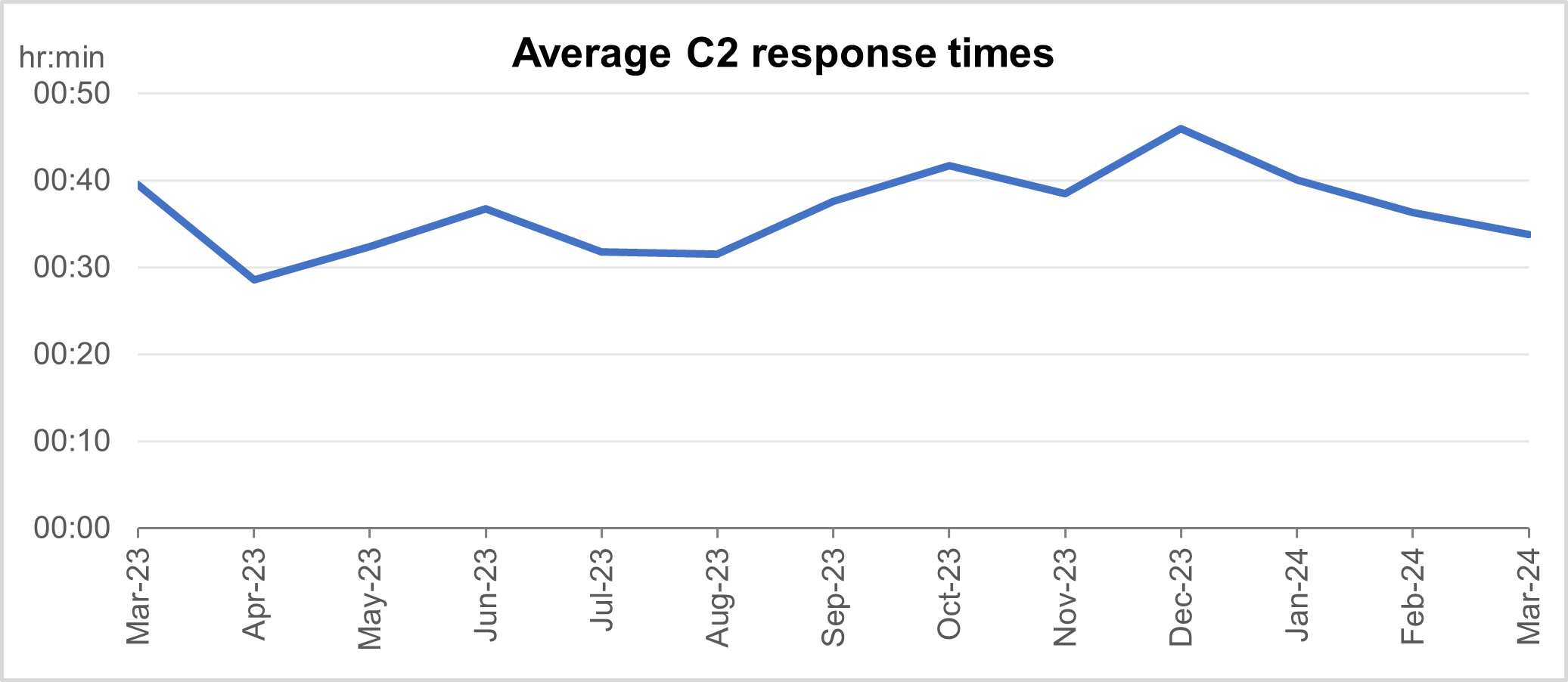
Average category 2 response times
Elective recovery
In February, despite disruption from another five days of industrial action and winter demand, the NHS made further progress in reducing long waits for patients.
1,476,736 patients started treatment, an increase of 0.5% per working day compared to February 2023 (1,399,288 patients started treatment in February 2023). 940,394 started treatment within 18 weeks of referral.
The number of patients waiting more than 65 weeks for treatment was 75,004 at the end of February, down from 92,213 (19%) in January and down by 68% from a peak of 233,051 in June 2021. Additional management data [2] published this month suggests there was a further reduction between February and March, with 50,448 patients waiting more than 65 weeks for treatment as of the end of March.
[2] Management information for the latest month is taken from the Waiting List Minimum Dataset which is subject to less validation than the published monthly figures and does not include estimates for missing providers (133 of 135 acute trusts submitted data for the latest month).
Referral to treatment 65 week waits
9,969 patients were waiting more than 78 weeks for treatment at the end of February, down from 14,013 (29%) in January and down by 92% from a peak of 124,911 in September 2021. Again, the additional management data suggests a further reduction between February and March, with 5,049 patients waiting more than 78 weeks for treatment as of the end of March.
Referral to treatment 78 week waits
This month’s statistics are reflective of the recent changes to the reporting requirements of community services pathways [3] meaning all community services (eg community paediatrics and community medicine) should now be recorded within community datasets rather than the referral to treatment data. This is estimated to have affected the number of 65 and 78 week waits by about 2500 and 1400 respectively.
[3] From February 24, community services pathways (eg community paediatrics and community medicine) should now be recorded within community datasets rather than the referral to treatment data. This change is reflected in the change between January and February 24: it is estimated there were about 4,900 fewer 52 week waiters, 2,500 fewer 65 week waiters and 1,400 fewer 78 week waiters as a result of the change.
Cancer
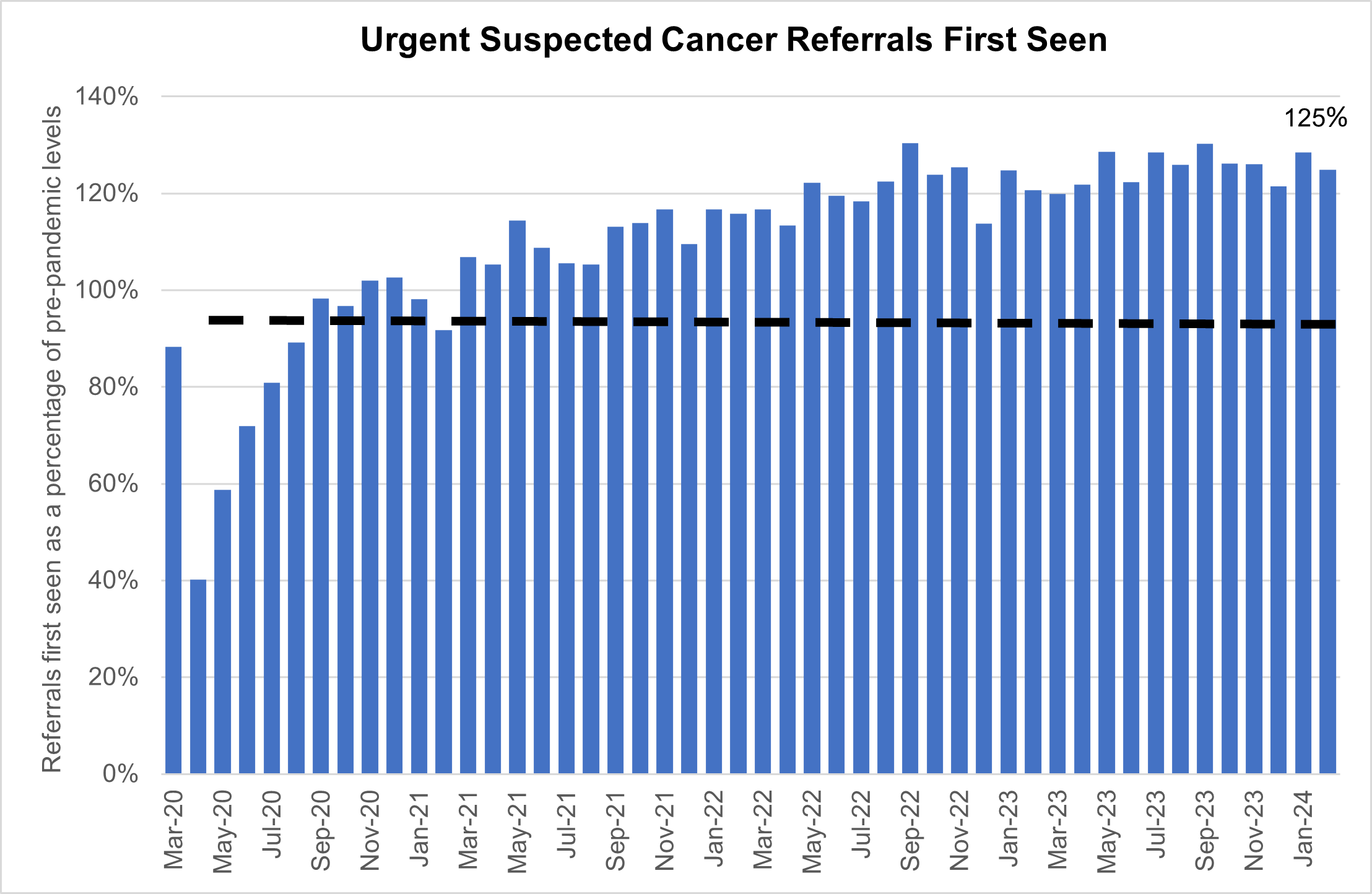
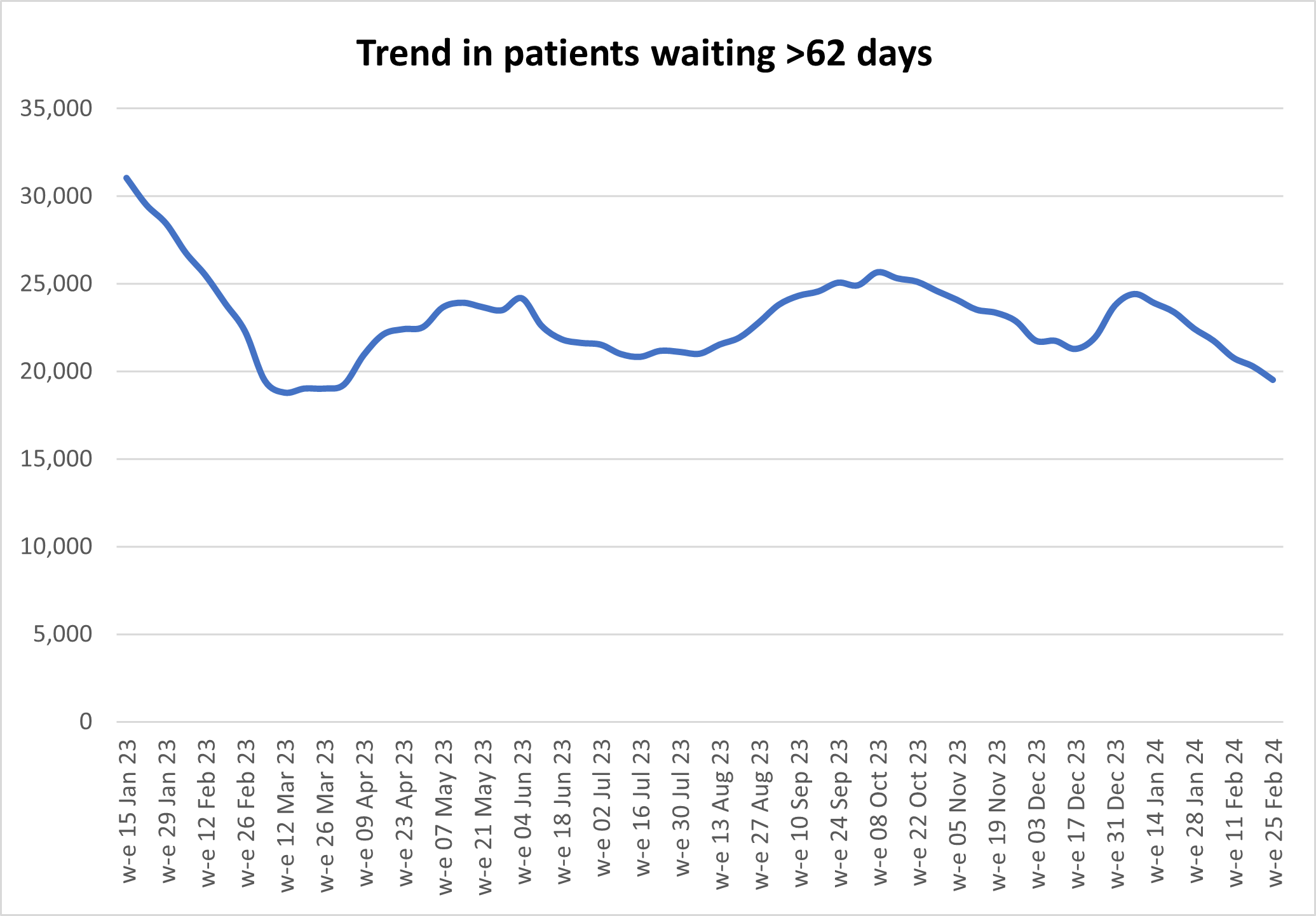
Demand for cancer services continued at record levels in February 2024 with the number of urgent suspected cancer referrals at 125% of pre-pandemic levels. To meet high demand, treatment is also at record levels and there has been a reduction in the 62- day cancer backlog as a result.
Urgent suspected cancer referrals first seen
Over 344,000 people received their first treatment for cancer over the last year between March 2023 and February 2024 – the highest year on record, and up by around 32,000 on the same period pre-pandemic.
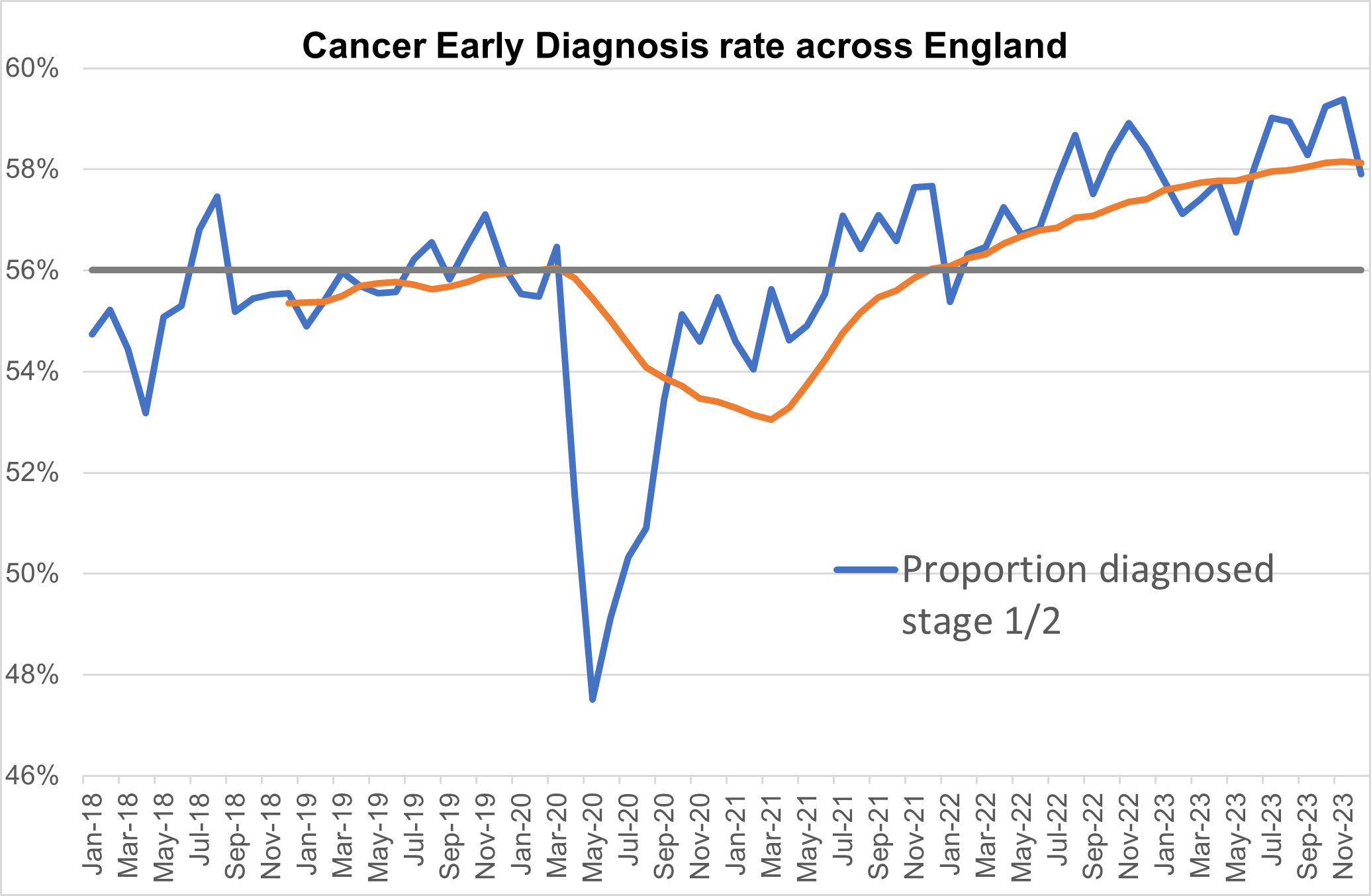
GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over a million more people than in the same period prior to the pandemic. The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic.
Survival is also at an all-time high. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
Cancer early diagnosis rate across England
The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in community diagnostic centres.
The backlog has already reduced over 10,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Trend in patients waiting more than 62 days
Mental health
More people than ever before are now in contact with NHS services for support for their mental health, with almost five million patients in contact with services in 2022/23, an increase of more than one million compared to 2016/17. This includes 1.1 million children and young people, 1.3 million adults in contact with core community mental health services, 1.2 million adults in contact with NHS talking therapies services, and 85,000 people in contact with specialist perinatal mental health services.
Services across the country have made great efforts to improve access and reduce waiting times, but this comes against a backdrop of increased needs and complex conditions. It is particularly the case for children and young people – about one in five children and young people aged 8 to 16 years had a probable mental disorder. This compares to around one in nine 5 to 16-year-olds in 2017. The pandemic and its aftermath have exacerbated the factors that contribute to poor mental health such as isolation, financial anxiety and long-term illness. Demand for mental health care is at an all-time high, with bed occupancy still above 95% across NHS mental health hospitals.
The NHS keeps working hard to continue to expand its mental health offer, supported by an extra £2.3 billion a year by April 2024. This includes improving children and young people’s community services and rolling out new initiatives, such as mental health support teams in schools and colleges which are on track to cover over 4 million (44%) pupils and learners in spring 2024 [4], increasing to around 5 million (around 50%) in spring 2025. These teams offer support for common mental health mild to moderate conditions such as anxiety and depression and can refer those who need more specialised care to local mental health services.
In February 2024, 780,963 children and young people accessed NHS mental health services. This is 266,999 above the NHS Long Term Plan baseline (513,964).
[4] Confirmation expected to be published May 2024.