Executive summary
1. The total waiting list and unique patient number have fallen despite disruption from ongoing industrial action and sustained demand, with reductions also seen in the number of people waiting more than 18 and 52 weeks for care. Over 1.55 million patients began treatment in October 2023, 7.4% more than the previous month.
2. Pressure has continued in emergency departments across the country, with more than 2.1 million A&E attendances and over 545,000 emergency admissions in November 2023.
3. Ambulance services also faced continued high demand, with more than 826,000 calls to 999 answered by staff throughout the month, an average of 27,500 every day. However, average response times to category one and two incidents improved in November.
4. Continuing industrial action in the NHS has had a significant impact on patients. Since strikes began, more than one million acute inpatient and outpatient appointments have been rescheduled.
5. Demand for cancer services continued at record levels in October 2023, with the number of urgent suspected cancer referrals at 126% of pre-pandemic levels.
6. There is sustained demand for mental health services, with five million patients accessing care in 2022/23, an increase of more than one million in five years. The NHS has now rolled out specialist perinatal mental health services in all areas of the country, and last year treated more than 51,000 new mothers, up nearly 70% compared to three years ago.
7. In October 2023, 37.2 million GP appointments took place. Of these, 39.3% took place on the same day they were booked and 70.9% were carried out face to face.
Urgent and emergency care
Urgent and emergency care (UEC) services faced high levels of demand in November. Winter pressures and high bed occupancy inevitably impacted hospital flow.
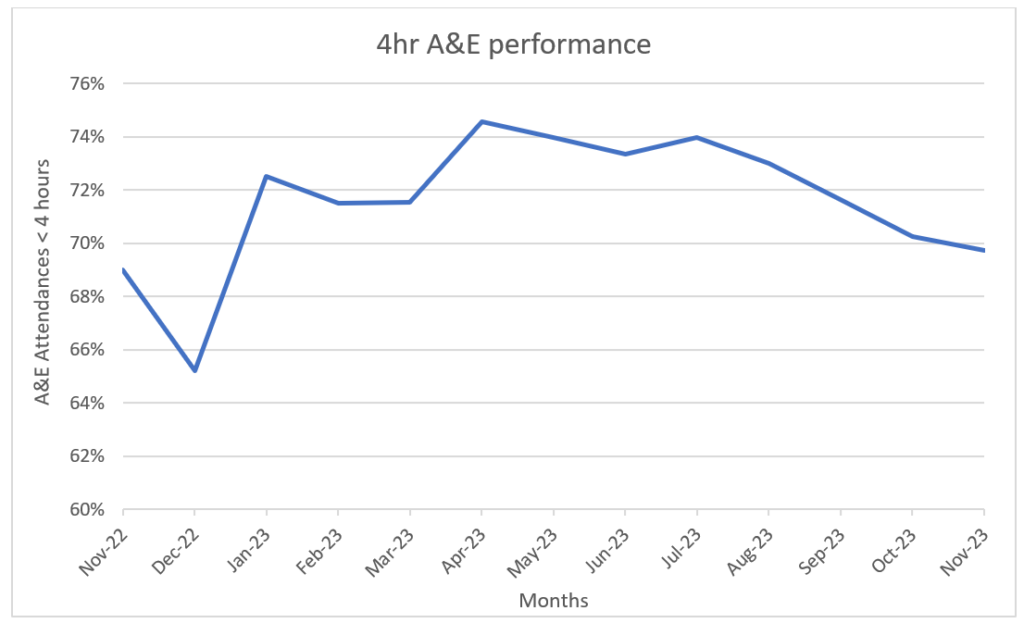
There were 2,162,122 attendances in A&Es across England, an average of 72,071 per day. 69.7% of patients attending A&E were admitted, transferred or discharged within 4 hours. This compares to 69% in November 2022.
Percentage of patients seen within 4 hours in A&E departments
Ambulance services answered 826,023 calls to 999, or 27,534 per day. They also handled 709,217 incidents. 365,645 of incidents were conveyed to A&E, or 12,188 per day, an increase of 1.5% compared to October and 4.3% more than the same point last year.
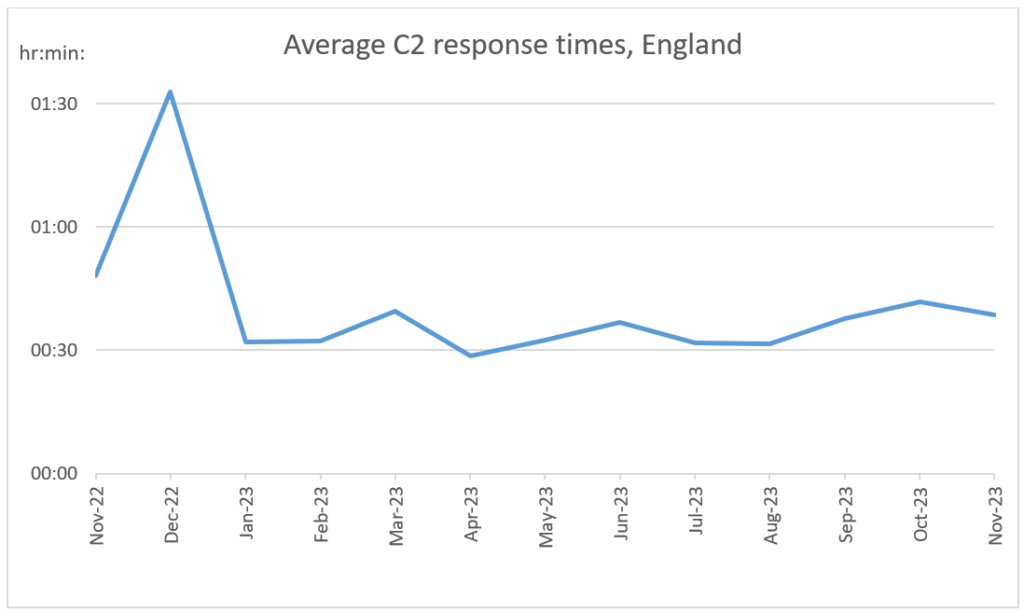
The average response time for a category two call was 38 minutes and 30 seconds. This is 9 minutes and 40 seconds faster compared to the same month last year (England, excluding London, had an average C2 response time of 48 minutes and 10 seconds in November 2022).
Average C2 response times, England
In July we introduced an incentive scheme to encourage providers to go further on achieving the two key ambitions in the UEC recovery plan. This included completing at least 90% of ambulance handovers within 30 minutes during the second half of 2023/24.
To support this, we have introduced monthly data showing known handover times for NHS trusts. In November, the mean time of known handovers was 35 minutes and 4 seconds.
We recently started publishing a new dataset which captures the time between a patient being ready to leave hospital and their actual date of discharge. We have received submissions from 58.5% of trusts, which will support collaborative action across the NHS, local government, and social care to improve discharge planning and patient flow.
This month we have expanded the publication to include average discharge delays (excluding zero-day delays), and information on discharges from trusts by local authority.
During October, 86.7% of patients with a hospital stay of one night or longer left hospital on their discharge ready date. Of those who stayed in hospital beyond their discharge ready date, 31.5% left hospital one day after their discharge ready date and 6.4% had an extended stay of 21 days or more.
Elective recovery
Three days of joint industrial action by junior doctors and consultants inevitably impacted planned care in October. During the week of Monday 2 October, 118,026 inpatient and outpatient appointments had to be rescheduled.
Despite this, the total waiting list reduced by 65,518 (1%) compared to September. As of the end of October, there were 7.71 million waits for care and an estimated 6.44 million unique patients on the elective waiting list.
1,553,941 patients started treatment in October, an increase of 7% from September. 991,389 started treatments within 18 weeks of referral. This is an increase of 5% from last month.
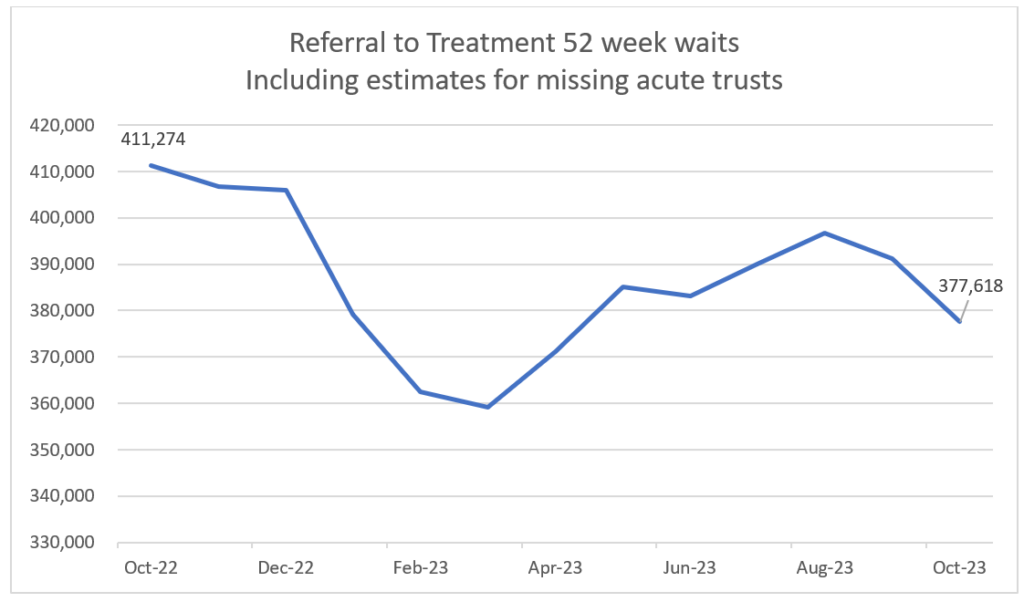
Progress was made in reducing some of the longest waits for care. As of the end of October, 377,618 (5%) patients were waiting more than a year for treatment. This is down by 13,504 compared to September.
Referral to treatment 52 week waits
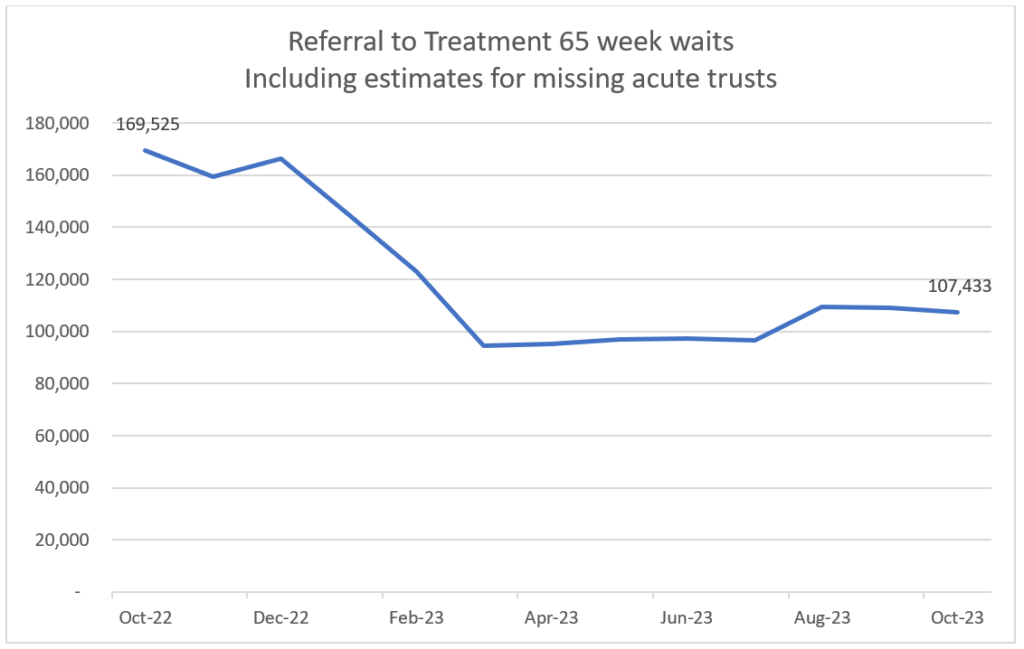
107,433 (1%) patients were waiting more than 65 weeks for treatment. This is down by 2% from September.
Referral to treatment 65 weeks waits
Cancer
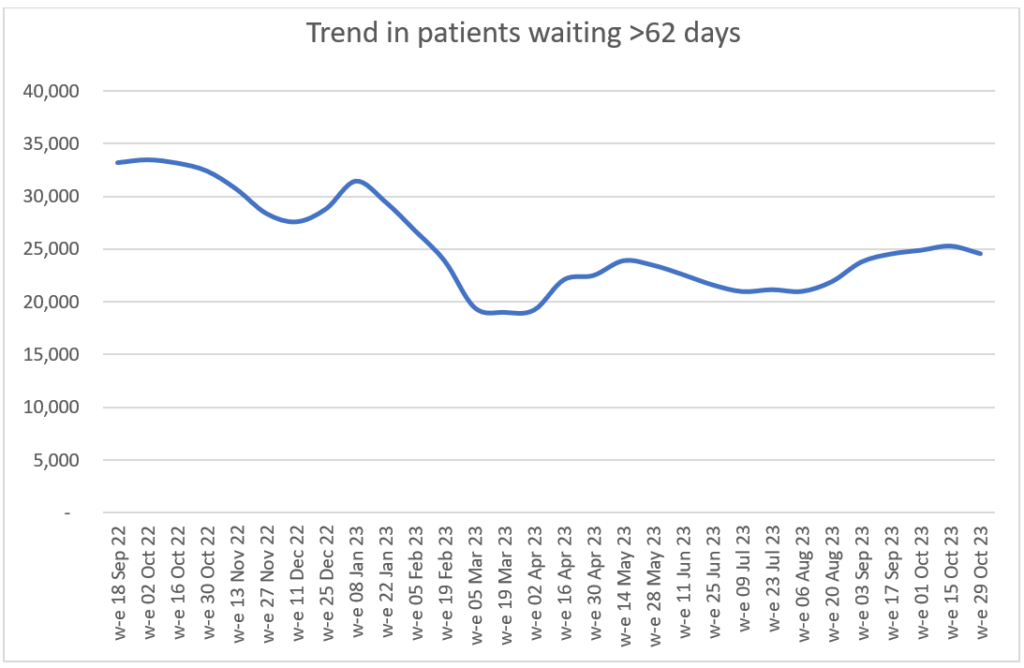
Demand for cancer services continued at record levels in October 2023 with the number of urgent suspected cancer referrals at 126% of pre-pandemic levels. To meet high demand, treatment is also at record levels and there has been a reduction in the 62-day cancer backlog as a result.
Urgent suspected cancer referrals first seen
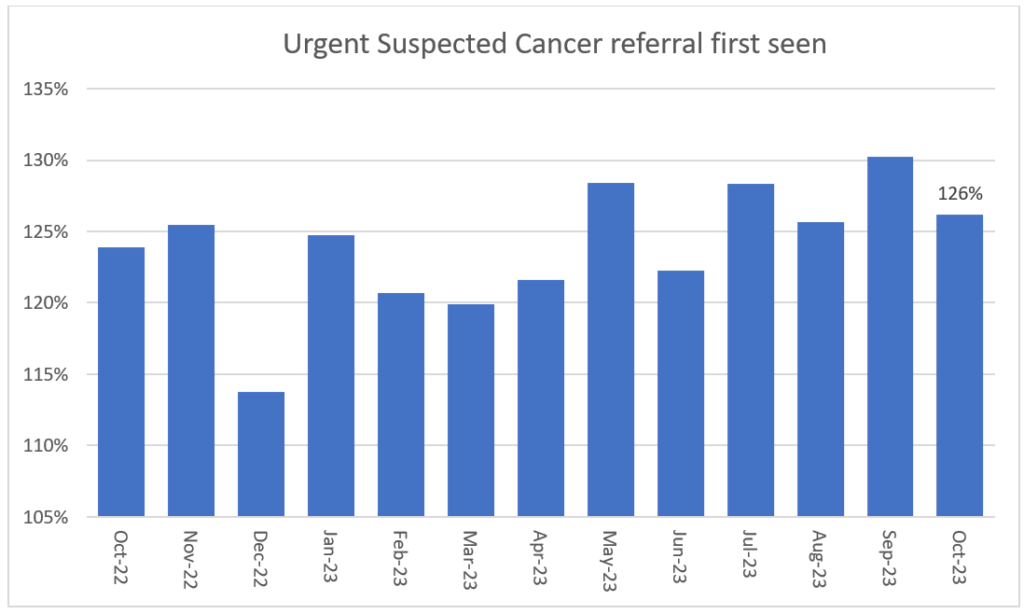
Over 335,000 people received treatment for cancer over the last year between November 2022 and October 2023 – the highest year on record, and up by more than 22,000 on the same period pre-pandemic.
GPs have been referring people for urgent cancer checks in record numbers since March 2021. Since then, NHS staff have seen over a million more people than in the same period prior to the pandemic.
The increase in referrals has contributed to the NHS diagnosing more cancer at an early stage than ever before. We are diagnosing a higher proportion of cancers at an early stage now than ever before – about 2% higher than before the pandemic.
Survival is also at an all-time high. In 2023, the Annals of Oncology published findings showing that cancer deaths are around 10% lower in the UK compared to just 5 years ago.
The NHS is working hard to keep up with this increase in demand. It has been accelerating the installation of new diagnostic capacity, much of it in Community Diagnostic Centres.
The backlog has already reduced by 14,000 people since its peak last summer, and despite the recent seasonal increase, NHS staff remain focused on ensuring that people who have been waiting longest or who need care most urgently are seen first.
Trend in patients waiting more than 62 days
Mental health
More people than ever before are now in contact with NHS services for support for their mental health, with almost five million patients in contact with services in 2022/23, an increase of more than 1 million in 5 years.
During this time, the NHS has rolled out specialist community perinatal services in all areas of the country, and more than 53,000 new mums were treated over the last year, up nearly 70% compared to 3 years ago.
With around 1 in 4 women experiencing mental health problems during pregnancy and the 24 months after giving birth, the NHS is committed to keep increasing the support available to mothers.
New Maternal Mental Health Services (MMHS) are being rolled out to provide psychological therapy for women experiencing moderate to severe or complex mental health difficulties directly arising from birth trauma or perinatal loss.
Since 2020, 38 MMHS have been established, with services planning to be operational in all 42 ICS areas by March 2024.
Support for children and young people (CYP) with eating disorders is also a top priority for the NHS. Our recent prevalence report highlights that between 2017 and 2023, the number of those suffering from an eating disorder has increased, especially among girls.
In a context of increased demand, we are treating more CYP with an eating disorder than ever before, and our access and waiting time standard in this area is improving.
In October 2023:
- 63.7% CYP started urgent eating disorder treatment within 1 week, compared to 60.8% in June 2023.
- 76.9% CYP started routine eating disorder treatment within 4 weeks, compared to 66.7% in June 2023.

